Podcast
Questions and Answers
What type of toxin is produced by the difficile disease?
What type of toxin is produced by the difficile disease?
- Exotoxin
- Neurotoxin
- Cytotoxin (correct)
- Endotoxin
Ninety percent of healthy individuals colonize the intestines with difficile disease.
Ninety percent of healthy individuals colonize the intestines with difficile disease.
True (A)
What are the symptoms associated with epidemic typhus?
What are the symptoms associated with epidemic typhus?
Abrupt onset fever, headache, chills, myalgias, arthralgia
The implicated antibiotic should be ____ for treatment.
The implicated antibiotic should be ____ for treatment.
Match the disease with its onset duration:
Match the disease with its onset duration:
Which of the following is NOT a symptom of scrub typhus?
Which of the following is NOT a symptom of scrub typhus?
The enterotoxin produced is heat-sensitive.
The enterotoxin produced is heat-sensitive.
What leads to the loss of fluids in the small intestine in difficile disease?
What leads to the loss of fluids in the small intestine in difficile disease?
Which species of Clostridium is primarily responsible for causing myonecrosis?
Which species of Clostridium is primarily responsible for causing myonecrosis?
Clostridium difficile infection is commonly caused by antibiotic usage.
Clostridium difficile infection is commonly caused by antibiotic usage.
What disease is primarily associated with Clostridium septicum?
What disease is primarily associated with Clostridium septicum?
Clostridium botulinum causes food poisoning through the ingestion of ______.
Clostridium botulinum causes food poisoning through the ingestion of ______.
Match the following Clostridium species with their associated disease:
Match the following Clostridium species with their associated disease:
What is one of the major toxins produced by Clostridium perfringens?
What is one of the major toxins produced by Clostridium perfringens?
Clostridium difficile can cause antibiotic-associated diarrhea five to six weeks after the initiation of antibiotic treatment.
Clostridium difficile can cause antibiotic-associated diarrhea five to six weeks after the initiation of antibiotic treatment.
What type of organism is Clostridium difficile?
What type of organism is Clostridium difficile?
The most severe form of C. difficile disease characterized by profuse diarrhea is called __________.
The most severe form of C. difficile disease characterized by profuse diarrhea is called __________.
Which of the following antibiotics is C. difficile resistant to?
Which of the following antibiotics is C. difficile resistant to?
Match the following Clostridium perfringens characteristics with their descriptions.
Match the following Clostridium perfringens characteristics with their descriptions.
What cleaning measure should be taken after a C. difficile infected patient is discharged from the hospital?
What cleaning measure should be taken after a C. difficile infected patient is discharged from the hospital?
C. difficile is known for causing __________, a serious and potentially life-threatening condition associated with severe gastrointestinal symptoms.
C. difficile is known for causing __________, a serious and potentially life-threatening condition associated with severe gastrointestinal symptoms.
Flashcards are hidden until you start studying
Study Notes
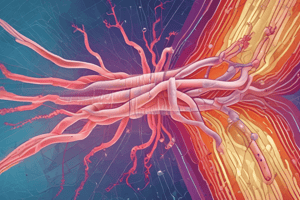
Clostridium difficile Overview
- Confirmed disease through detection of cytotoxin, enterotoxin, or toxin genes in feces.
- Characterized by destruction of blood cells and tissues, leading to severe conditions like sepsis and myonecrosis.
- Highly virulent strains have emerged in hospitals and the community, particularly in Canada, the US, and Europe.
Epidemiology
- Colonizes intestines of 90% of healthy individuals without causing disease.
- Spores detected in hospital environments, especially around beds and bathrooms, serving as a source of exogenous infection.
Treatment, Prevention, and Control
- Antibiotics targeted against C. difficile should be used, though they are less effective against spores.
- Cleaning hospital rooms post-discharge and preventing the spread of spores are crucial.
- Relapse common; additional antibiotic courses might be needed since spores are resistant to standard treatments.
Pathogenesis
- Large anaerobic rods that form spores and produce volatile fatty acids.
- Primary virulence factors are two toxins:
- Enterotoxin: attracts neutrophils, prompting cytokine release.
- Cytotoxin: increases intestinal wall permeability, leading to diarrhea.
Disease Manifestations
- Antibiotic-associated diarrhea: develops within 5-10 days of initial antibiotic treatment; can be self-limited or prolonged.
- Pseudomembranous colitis: most severe form, characterized by profuse diarrhea, abdominal pain, fever, and formation of pseudomembranes in the colon.
Clostridium perfringens
- Major cause of myonecrosis and food poisoning; known for weak spore formation and environmental presence.
- Capable of causing sepsis; often managed with surgical debridement.
- Produces various toxins and enzymes that contribute to its pathogenicity.
Infection Comparison
- Food poisoning by C. perfringens due to ingestion of toxins (intoxication) has clinical variations; symptoms differ from those caused by C. botulinum, affecting treatment strategies and patient outcomes.
High-Risk Patient Populations
- Specific diseases caused by Clostridium septicum require awareness of susceptible groups, particularly immunocompromised individuals.
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.