Podcast
Questions and Answers
What is a significant disadvantage of using dialysis catheters?
What is a significant disadvantage of using dialysis catheters?
- They can be used immediately for dialysis.
- They are less prone to infections compared to AV grafts.
- They may cause long-term damage to the veins. (correct)
- They require less maintenance than AV grafts.
Which statement is true regarding AV grafts compared to dialysis catheters?
Which statement is true regarding AV grafts compared to dialysis catheters?
- AV grafts are less prone to infections.
- AV grafts typically have a shorter maturation time. (correct)
- AV grafts are easier to maintain than dialysis catheters.
- AV grafts require more than one operation to place.
What is a common requirement if a dialysis catheter becomes infected?
What is a common requirement if a dialysis catheter becomes infected?
- It requires complete removal and prolonged antibiotics. (correct)
- It requires temporary removal and no antibiotics.
- It needs to be replaced with a new catheter.
- It must be cleaned weekly to prevent infection.
What is a potential risk associated with the use of dialysis catheters over time?
What is a potential risk associated with the use of dialysis catheters over time?
Which statement accurately reflects the longevity of AV grafts?
Which statement accurately reflects the longevity of AV grafts?
Which of the following conditions is primarily characterized by impaired insulin secretion and variable degrees of insulin resistance?
Which of the following conditions is primarily characterized by impaired insulin secretion and variable degrees of insulin resistance?
What is the first phase of insulin release triggered by?
What is the first phase of insulin release triggered by?
What crucial role do muscle and fat cells play in relation to insulin?
What crucial role do muscle and fat cells play in relation to insulin?
What is the primary method for diagnosing diabetes mellitus?
What is the primary method for diagnosing diabetes mellitus?
Which of the following conditions is NOT a complication associated with diabetes mellitus?
Which of the following conditions is NOT a complication associated with diabetes mellitus?
What happens to insulin release when blood glucose levels return to normal physiological values?
What happens to insulin release when blood glucose levels return to normal physiological values?
Which of the following processes is initiated by insulin binding to its receptor?
Which of the following processes is initiated by insulin binding to its receptor?
What is the main storage form of glucose in the human body?
What is the main storage form of glucose in the human body?
What is the primary mechanism of action for sulfonylureas?
What is the primary mechanism of action for sulfonylureas?
Which of the following classes of oral anti-diabetic drugs is mainly known for its insulin-sensitizing effects?
Which of the following classes of oral anti-diabetic drugs is mainly known for its insulin-sensitizing effects?
For patients with type 2 diabetes who don’t respond to lifestyle changes, which is a recommended therapeutic approach?
For patients with type 2 diabetes who don’t respond to lifestyle changes, which is a recommended therapeutic approach?
Which mechanism is primarily attributed to biguanides?
Which mechanism is primarily attributed to biguanides?
What effect do thiazolidinediones potentially have beyond lowering blood glucose?
What effect do thiazolidinediones potentially have beyond lowering blood glucose?
What role do α-glucosidase inhibitors play in diabetes management?
What role do α-glucosidase inhibitors play in diabetes management?
How do dipeptidyl peptidase-4 inhibitors contribute to diabetes management?
How do dipeptidyl peptidase-4 inhibitors contribute to diabetes management?
What underlying condition is associated with macrovascular disease in diabetes?
What underlying condition is associated with macrovascular disease in diabetes?
What causes the vascular complications in Non Proliferative Diabetic Retinopathy (NPDR)?
What causes the vascular complications in Non Proliferative Diabetic Retinopathy (NPDR)?
What is the primary cause of vision loss in patients with Diabetic Retinopathy?
What is the primary cause of vision loss in patients with Diabetic Retinopathy?
What is a significant risk factor for the progression of Proliferative Diabetic Retinopathy (PDR)?
What is a significant risk factor for the progression of Proliferative Diabetic Retinopathy (PDR)?
Which treatment method is utilized to manage leaking blood vessels in diabetic retinopathy?
Which treatment method is utilized to manage leaking blood vessels in diabetic retinopathy?
What is the primary underlying mechanism of diabetic neuropathy?
What is the primary underlying mechanism of diabetic neuropathy?
What complication arises if the abnormal vessels in PDR are not treated?
What complication arises if the abnormal vessels in PDR are not treated?
What is diabetic neuropathy primarily characterized by?
What is diabetic neuropathy primarily characterized by?
Which of the following is NOT a manifestation of diabetes mentioned in the content?
Which of the following is NOT a manifestation of diabetes mentioned in the content?
What is the fasting plasma glucose (FPG) level indicative of diabetes?
What is the fasting plasma glucose (FPG) level indicative of diabetes?
Which treatment is most commonly recommended for type 1 diabetes mellitus?
Which treatment is most commonly recommended for type 1 diabetes mellitus?
What is the recommended age to aim for an HbA1c level of less than 7%?
What is the recommended age to aim for an HbA1c level of less than 7%?
What complication is very likely in the presence of diabetes mellitus?
What complication is very likely in the presence of diabetes mellitus?
Which of the following conditions indicates impaired glucose regulation based on an oral glucose tolerance test (OGTT)?
Which of the following conditions indicates impaired glucose regulation based on an oral glucose tolerance test (OGTT)?
Which of the following is not typically part of the treatment options for managing diabetes?
Which of the following is not typically part of the treatment options for managing diabetes?
What is the primary treatment goal regarding blood glucose levels during the day for individuals with diabetes?
What is the primary treatment goal regarding blood glucose levels during the day for individuals with diabetes?
Which of the following statements about islet cell antibodies in diabetes is correct?
Which of the following statements about islet cell antibodies in diabetes is correct?
What triggers the autoimmune destruction of pancreatic β-cells in Type 1 diabetes mellitus (DM)?
What triggers the autoimmune destruction of pancreatic β-cells in Type 1 diabetes mellitus (DM)?
What is a common characteristic of Type 2 diabetes mellitus (DM) regarding insulin levels?
What is a common characteristic of Type 2 diabetes mellitus (DM) regarding insulin levels?
Which statement accurately describes the onset of Type 1 and Type 2 diabetes mellitus?
Which statement accurately describes the onset of Type 1 and Type 2 diabetes mellitus?
What condition is commonly associated with insulin resistance in Type 2 DM?
What condition is commonly associated with insulin resistance in Type 2 DM?
In what way does Type 2 diabetes mellitus typically manifest in childhood due to recent trends?
In what way does Type 2 diabetes mellitus typically manifest in childhood due to recent trends?
What outcomes are characterized by Type 1 diabetes mellitus as it progresses?
What outcomes are characterized by Type 1 diabetes mellitus as it progresses?
What distinguishes Type 2 diabetes mellitus's response to insulin from that of Type 1 diabetes mellitus?
What distinguishes Type 2 diabetes mellitus's response to insulin from that of Type 1 diabetes mellitus?
What factors contribute to the high prevalence of Type 2 diabetes mellitus in older adults?
What factors contribute to the high prevalence of Type 2 diabetes mellitus in older adults?
Flashcards
What is diabetes mellitus?
What is diabetes mellitus?
Diabetes mellitus (DM) is a chronic disease characterized by high blood sugar levels due to either insufficient insulin production or the body's inability to effectively use insulin.
What are some early symptoms of diabetes?
What are some early symptoms of diabetes?
Early symptoms of diabetes include excessive thirst (polydipsia), increased hunger (polyphagia), and frequent urination (polyuria).
What is insulin?
What is insulin?
Insulin is a hormone, produced by the pancreas, that regulates blood sugar levels by allowing glucose (sugar) to enter cells.
Where is insulin produced?
Where is insulin produced?
Signup and view all the flashcards
How is insulin released?
How is insulin released?
Signup and view all the flashcards
How does insulin work?
How does insulin work?
Signup and view all the flashcards
What are the primary target cells for insulin?
What are the primary target cells for insulin?
Signup and view all the flashcards
How is diabetes diagnosed?
How is diabetes diagnosed?
Signup and view all the flashcards
Type 1 Diabetes (T1D)
Type 1 Diabetes (T1D)
Signup and view all the flashcards
Type 2 Diabetes (T2D)
Type 2 Diabetes (T2D)
Signup and view all the flashcards
Insulin Resistance
Insulin Resistance
Signup and view all the flashcards
Hepatic Glucose Production
Hepatic Glucose Production
Signup and view all the flashcards
Juvenile-Onset Diabetes
Juvenile-Onset Diabetes
Signup and view all the flashcards
Adult-Onset Diabetes
Adult-Onset Diabetes
Signup and view all the flashcards
Insulin
Insulin
Signup and view all the flashcards
Pancreatic Beta Cells
Pancreatic Beta Cells
Signup and view all the flashcards
Glomerulopathy
Glomerulopathy
Signup and view all the flashcards
Hemodialysis
Hemodialysis
Signup and view all the flashcards
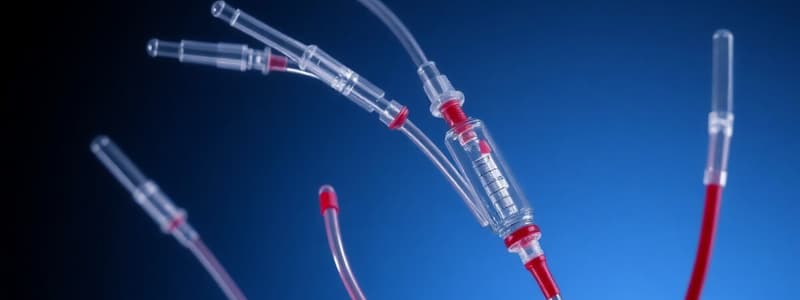
Dialysis Catheter
Dialysis Catheter
Signup and view all the flashcards
AV Graft
AV Graft
Signup and view all the flashcards
Graft Maturation
Graft Maturation
Signup and view all the flashcards
Classes of Oral Anti-Diabetics
Classes of Oral Anti-Diabetics
Signup and view all the flashcards
How do Sulfonylureas work?
How do Sulfonylureas work?
Signup and view all the flashcards
What are Island Cell Antibodies?
What are Island Cell Antibodies?
Signup and view all the flashcards
How do Biguanides work?
How do Biguanides work?
Signup and view all the flashcards
What does it mean when islets are smaller?
What does it mean when islets are smaller?
Signup and view all the flashcards
How do Thiazolidinediones work?
How do Thiazolidinediones work?
Signup and view all the flashcards
Why are complications of diabetes more likely when insulin production is low?
Why are complications of diabetes more likely when insulin production is low?
Signup and view all the flashcards
How do Alpha-glucosidase inhibitors work?
How do Alpha-glucosidase inhibitors work?
Signup and view all the flashcards
What happens when the body doesn't respond to insulin?
What happens when the body doesn't respond to insulin?
Signup and view all the flashcards
Why might oral antidiabetic medication not be helpful?
Why might oral antidiabetic medication not be helpful?
Signup and view all the flashcards
How do Dipeptidyl peptidase-4 inhibitors work?
How do Dipeptidyl peptidase-4 inhibitors work?
Signup and view all the flashcards
What is the diagnostic criterion for diabetes?
What is the diagnostic criterion for diabetes?
Signup and view all the flashcards
What are microvascular complications of Diabetes?
What are microvascular complications of Diabetes?
Signup and view all the flashcards
What are macrovascular complications of Diabetes?
What are macrovascular complications of Diabetes?
Signup and view all the flashcards
What is an Oral Glucose Tolerance Test (OGTT)?
What is an Oral Glucose Tolerance Test (OGTT)?
Signup and view all the flashcards
What is Diabetic Retinopathy?
What is Diabetic Retinopathy?
Signup and view all the flashcards
What is Non-Proliferative Diabetic Retinopathy (NPDR)?
What is Non-Proliferative Diabetic Retinopathy (NPDR)?
Signup and view all the flashcards
What is Proliferative Diabetic Retinopathy (PDR)?
What is Proliferative Diabetic Retinopathy (PDR)?
Signup and view all the flashcards
What is Laser Photocoagulation?
What is Laser Photocoagulation?
Signup and view all the flashcards
What is Diabetic Neuropathy?
What is Diabetic Neuropathy?
Signup and view all the flashcards
What is the pathophysiology of Diabetic Neuropathy?
What is the pathophysiology of Diabetic Neuropathy?
Signup and view all the flashcards
What is Peripheral Artery Disease (PAD)?
What is Peripheral Artery Disease (PAD)?
Signup and view all the flashcards
What is Diabetic Peripheral Neuropathy?
What is Diabetic Peripheral Neuropathy?
Signup and view all the flashcards
Study Notes
Diabetes Mellitus (DM) Definition
- Diabetes mellitus (DM) is characterized by impaired insulin secretion and varying degrees of peripheral insulin resistance leading to hyperglycemia.
- Early symptoms include polydipsia, polyphagia, and polyuria, all related to hyperglycemia.
- Later complications include vascular disease, peripheral neuropathy, and increased susceptibility to infection.
- Diagnosis involves measuring plasma glucose levels.
- Treatment options include diet, exercise, and medications that lower glucose levels, such as insulin and oral antihyperglycemic drugs.
- Prognosis varies depending on the degree of glucose control.
Insulin - The Key to Diabetes
- Insulin is synthesized within the beta cells (β-cells) of the islets of Langerhans in the pancreas.
- The endocrine portion of the pancreas makes up only 2% of its total mass.
- There are typically one to three million pancreatic islets within the pancreas.
- Insulin release occurs in two phases: a rapid initial phase triggered by increased blood glucose levels, and a later sustained, gradual release independent of current blood sugar levels.
- When glucose levels return to normal, insulin secretion from beta cells slows or stops.
- Insulin's primary role is the stimulation of glucose uptake, primarily in muscle and fat cells.
- Muscles utilize glucose for movement and other bodily functions, while fat cells store excess glucose for future use.
- Muscle and fat tissues combined account for approximately two-thirds of all cells in a human body.
Insulin's Mode of Action
- Insulin binds to its receptor, initiating a cascade of protein activation.
- This cascade triggers glucose translocation and influx into cells through the plasma membrane.
- Insulin also promotes glycogen synthesis, the storage form of glucose.
- Furthermore, insulin stimulates glycolysis and fatty acid synthesis, thereby increasing lipid synthesis.
Circadian Rhythm of Insulin
- Insulin levels and blood glucose levels follow a diurnal pattern.
- Blood glucose levels typically peak after consuming a meal, and insulin levels tend to follow these peaks in order to help with the absorption of glucose.
- Blood glucose levels (and insulin levels) naturally fluctuate throughout the day, influenced by eating patterns.
Type 1 and Type 2 Diabetes
- Type 1 DM: Characterized by an absolute absence of insulin production due to autoimmune destruction of pancreatic beta cells, potentially from environmental exposure in susceptible individuals.
- Type 1 generally manifests during childhood or adolescence, though it can occur at any age.
- Type 2 DM: Characterized by inadequate insulin secretion as well as peripheral insulin resistance and increased hepatic glucose production, which leads to elevated glucose levels.
- Type 2 generally develops in adulthood, but is becoming increasingly common in children due to rising rates of childhood obesity.
General Characteristics of Type 1 and Type 2 DM
- Type 1: Typically diagnosed before age 30; marked by severe insulin deficiency; often associated with the presence of detectable islet cell antibodies; and rarely associated with obesity.
- Type 2: Typically diagnosed after age 30; mainly characterized by peripheral insulin resistance and occasionally by moderately low or normal insulin levels; often associated with obesity.
Diagnostic Criteria for Diabetes Mellitus
- Fasting Plasma Glucose (FPG): Normal <100mg/dL, Impaired Glucose Regulation 100-125 mg/dL, Diabetes ≥ 126 mg/dL
- Oral Glucose Tolerance Test (OGTT): Normal <140 mg/dL, Impaired Glucose Regulation 140-199 mg/dL, Diabetes ≥200 mg/dL
Treatment Options and Goals
- Treatment options for both types of diabetes generally include diet, exercise, and medication.
- For Type 1, insulin is essential.
- Type 2 may be treated with oral antihyperglycemics, and even insulin may be necessary in some cases.
- Treatment goals are to maintain blood glucose levels within a specific range throughout the day.
- Aim for HbA1c levels below 7% to optimize long-term health outcomes.
Oral Anti-Diabetic Drugs
- Oral anti-diabetic drugs work through varied mechanisms, which include enhancing pancreatic insulin secretion, increasing peripheral tissue sensitivity to insulin, and decreasing glucose absorption from the gastrointestinal tract.
Diabetic Microvascular and Macrovascular Disease
- Microvascular diseases: lead to complications in small blood vessels. Examples include retinopathy, nephropathy, and neuropathy.
- Diabetic Neuropathy: Nerve damage due to ischemia (due to microvascular dz), excess glucose effects on neurons, or intracellular metabolic changes impairing nerve function. Sensorial and motor symptoms result.
- Macrovascular disease: affect large blood vessels, contributing to other complications like angina pectoris, transient ischemic attacks, strokes, and peripheral arterial disease.
Diabetic Retinopathy
- Diabetic retinopathy involves damage to the blood vessels in the retina.
- Early stages are non-proliferative (NPDR), where blood vessels leak and form deposits.
- Later stages, proliferative retinopathy (PDR), involve abnormal blood vessel growth, which is fragile and can lead to vision loss.
Diabetic Nephropathy
- Diabetic nephropathy causes kidney damage, often beginning with mild increases in blood pressure and albuminuria.
- The pathophysiology is complex and likely involves oxidative stress, excess glucose, and microvascular damage.
- Diabetic nephropathy stages can range from hyperfiltration and glomerular hypertrophy to severe kidney failure.
Diabetic Treatments & Complications Pathways
- Hemodialysis and peritoneal dialysis are treatments for patients with chronic kidney disease, which can be due to diabetes.
- Different surgical pathways for diabetes and complications are used for pancreas, kidney and for obesity, such as gastric banding and gastric bypasses.
- Other options may include simultaneous kidney and pancreas transplantation, which offers a potential treatment solution.
Other Diagnoses Associated with Kidney Transplants
- Kidney transplants are performed for various medical reasons, with diabetes accounting for a significant portion of cases.
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.