Podcast
Questions and Answers
What is the primary purpose of diagnostic tests in inflammatory bowel disease (IBD)?
What is the primary purpose of diagnostic tests in inflammatory bowel disease (IBD)?
- To assess the extent of the disease and its effects (correct)
- To confirm the presence of an infection in the intestine
- To monitor the effectiveness of surgical treatments
- To evaluate the efficiency of dietary interventions
Which of the following laboratory tests is NOT typically associated with diagnosing complications of IBD?
Which of the following laboratory tests is NOT typically associated with diagnosing complications of IBD?
- Urinalysis (correct)
- Liver function tests
- CBC with hemoglobin and hematocrit
- Stool cultures for infectious agents
In Crohn disease, which complication is the leading indication for surgical intervention?
In Crohn disease, which complication is the leading indication for surgical intervention?
- Bowel obstruction (correct)
- Abscess formation
- Perforation
- Internal fistula
What is a potential consequence of surgical resection in Crohn disease?
What is a potential consequence of surgical resection in Crohn disease?
Which vitamin levels are likely to decrease due to malabsorption in IBD patients?
Which vitamin levels are likely to decrease due to malabsorption in IBD patients?
What is the primary purpose of a strictureplasty in bowel treatment?
What is the primary purpose of a strictureplasty in bowel treatment?
What is the surgical procedure of choice for patients with extensive chronic ulcerative colitis?
What is the surgical procedure of choice for patients with extensive chronic ulcerative colitis?
What is a potential complication that may necessitate a total colectomy in ulcerative colitis patients?
What is a potential complication that may necessitate a total colectomy in ulcerative colitis patients?
What typically happens immediately after a total colectomy with ileal pouch–anal anastomosis?
What typically happens immediately after a total colectomy with ileal pouch–anal anastomosis?
Which factors may prevent a patient from undergoing an ileal pouch–anal anastomosis?
Which factors may prevent a patient from undergoing an ileal pouch–anal anastomosis?
Flashcards are hidden until you start studying
Study Notes
Diagnostic Tests
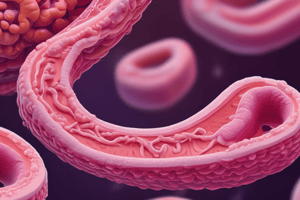
- Sigmoidoscopy, colonoscopy, and barium x-rays are used to identify the characteristic changes of IBD within the bowel mucosa.
- Stool examinations can detect blood and mucus as well as rule out infectious causes of inflammation and diarrhea.
- Complete blood count (CBC) can reveal anemia caused by chronic inflammation, blood loss, and malnutrition; leukocytosis may be due to inflammation and potential abscess formation.
- Elevated sedimentation rate is common during periods of acute inflammation.
- Decreased serum albumin can occur due to malabsorption, malnutrition, protein loss through intestinal lesions, and chronic inflammation.
- Low folic acid and vitamin levels, specifically A, B complex, C, and fat-soluble vitamins, can be caused by malabsorption.
- Elevated liver enzymes such as ALT, alkaline phosphatase, AST, GGTP, and LDH, as well as bilirubin levels, can indicate sclerosing cholangitis.
Surgical Interventions
- Surgery for IBD is usually a last resort, performed when complications of the disease arise or conservative treatments fail.
Crohn Disease
- Bowel obstruction is the most frequent reason for surgery in Crohn's disease.
- Other complications requiring surgery include perforation, fistulas (internal or external), abscesses, and perianal complications.
- Typical treatment involves resection of the affected bowel segment with end-to-end anastomosis, aiming to preserve as much bowel as possible.
- Disease recurrence is common in other areas following removal of affected segments.
- Fistula formation risk increases after surgery.
- Strictureplasties can be used to treat bowel strictures, involving longitudinal incisions in the narrowed segment to relieve constriction while preserving bowel.
Ulcerative Colitis
- Total colectomy (surgical resection and removal of the colon) may be necessary for patients with extensive chronic UC, to treat the disease itself, manage complications like toxic megacolon, perforation, or hemorrhage, or as a prophylactic measure against the high colon cancer risk associated with extensive UC.
- Total colectomy with an ileal pouch-anal anastomosis (IPAA) is the preferred procedure for extensive UC. This involves removal of the entire colon and rectum, creation of a pouch from the terminal ileum, and its connection to the anal canal.
- Temporary loop ileostomy is typically performed concurrently and maintained for 2-3 months to allow the anal anastomosis to heal.
- Once healed, the ileostomy is closed, resulting in 6-8 daily bowel movements through the anus.
- Patients ineligible for IPAA due to factors like advanced age or obesity may require permanent ileostomy or continent ileostomy for management.
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.