Podcast
Questions and Answers
At what week of intrauterine life does the complete fusion of Mullerian ducts occur?
At what week of intrauterine life does the complete fusion of Mullerian ducts occur?
- 10 weeks (correct)
- 5 months
- 18 weeks
- 20 weeks
The septa resolves to form a single uterine cavity by 18-20 weeks of intrauterine life.
The septa resolves to form a single uterine cavity by 18-20 weeks of intrauterine life.
True (A)
From which embryonic structure do the ovaries develop?
From which embryonic structure do the ovaries develop?
genital ridge
The lower 2/3rd of the vagina develops from the __________.
The lower 2/3rd of the vagina develops from the __________.
Match the following mullerian malformations with their classifications:
Match the following mullerian malformations with their classifications:
Which of the following is a use of MRI in gynecological investigations?
Which of the following is a use of MRI in gynecological investigations?
Transvaginal ultrasound (TVS) is easy to perform in postmenopausal females.
Transvaginal ultrasound (TVS) is easy to perform in postmenopausal females.
What is the transitional zone (TZ) size indicative of adenomyosis on MRI?
What is the transitional zone (TZ) size indicative of adenomyosis on MRI?
The _____ is the best investigation for soft tissue evaluation in gynecological conditions.
The _____ is the best investigation for soft tissue evaluation in gynecological conditions.
Match the following conditions with their corresponding imaging technique:
Match the following conditions with their corresponding imaging technique:
Which of the following characteristics distinguishes a cystocele from Gartner's cyst?
Which of the following characteristics distinguishes a cystocele from Gartner's cyst?
Gartner's cyst is typically located on the posterior wall of the vagina.
Gartner's cyst is typically located on the posterior wall of the vagina.
What is the management approach for an asymptomatic Gartner's cyst?
What is the management approach for an asymptomatic Gartner's cyst?
The __________ is responsible for forming the majority of the female internal genitalia.
The __________ is responsible for forming the majority of the female internal genitalia.
Match the following conditions to their descriptions:
Match the following conditions to their descriptions:
What classification represents the mildest form of defect in female reproductive organs?
What classification represents the mildest form of defect in female reproductive organs?
The T-shaped uterus is a common finding associated with in-utero exposure to DES.
The T-shaped uterus is a common finding associated with in-utero exposure to DES.
What is the most common cancer associated with vaginal adenosis?
What is the most common cancer associated with vaginal adenosis?
In the classification of defects, the defect known as __________ is described as having a flat-topped uterus.
In the classification of defects, the defect known as __________ is described as having a flat-topped uterus.
Match the following features with their respective defects:
Match the following features with their respective defects:
Which duct is responsible for developing female internal genitalia?
Which duct is responsible for developing female internal genitalia?
The Wolffian Duct primarily contributes to the development of female reproductive organs.
The Wolffian Duct primarily contributes to the development of female reproductive organs.
What are the remnants of the Wolffian Duct found in females called?
What are the remnants of the Wolffian Duct found in females called?
At ___ weeks, the Mullerian Duct forms internal genital organs in females.
At ___ weeks, the Mullerian Duct forms internal genital organs in females.
Match the following ducts with their corresponding origins:
Match the following ducts with their corresponding origins:
What is a characteristic feature of a bicornuate uterus?
What is a characteristic feature of a bicornuate uterus?
A septate uterus has a divided fundus.
A septate uterus has a divided fundus.
What is the approximate distance between the horns of a bicornuate uterus?
What is the approximate distance between the horns of a bicornuate uterus?
An __________ uterus appears split into two separate compartments.
An __________ uterus appears split into two separate compartments.
Match the uterine shapes with their descriptions:
Match the uterine shapes with their descriptions:
What is the primary purpose of SIS (Saline Infusion Sonography)?
What is the primary purpose of SIS (Saline Infusion Sonography)?
Hysterosalpingography (HSG) can be performed on a patient who is currently pregnant.
Hysterosalpingography (HSG) can be performed on a patient who is currently pregnant.
What type of dye is used in the Hysterosalpingography procedure?
What type of dye is used in the Hysterosalpingography procedure?
During the SIS procedure, saline appears __________ on ultrasound.
During the SIS procedure, saline appears __________ on ultrasound.
Match the following procedures with their primary indications:
Match the following procedures with their primary indications:
What is one of the primary uses of Hysterosalpingography (HSG)?
What is one of the primary uses of Hysterosalpingography (HSG)?
Hysteroscopy is primarily a therapeutic procedure that eliminates all uterine pathologies.
Hysteroscopy is primarily a therapeutic procedure that eliminates all uterine pathologies.
Name one possible filling defect that can be identified during an HSG procedure.
Name one possible filling defect that can be identified during an HSG procedure.
_________ media is used to visualize the uterine cavity during hysteroscopy.
_________ media is used to visualize the uterine cavity during hysteroscopy.
Match the following distension media with their type.
Match the following distension media with their type.
What defect is characterized by the presence of both Mullerian ducts but only fusion in the vagina and cervix?
What defect is characterized by the presence of both Mullerian ducts but only fusion in the vagina and cervix?
A uterine defect with a longitudinal septum can be identified using 2 LW cannulae during a HSG procedure.
A uterine defect with a longitudinal septum can be identified using 2 LW cannulae during a HSG procedure.
What classification represents the defect known as a septate uterus?
What classification represents the defect known as a septate uterus?
In a uterus diadelphys, the uterus has __________ halves, and the vagina is divided accordingly.
In a uterus diadelphys, the uterus has __________ halves, and the vagina is divided accordingly.
Match the following uterine defects with their classifications:
Match the following uterine defects with their classifications:
Which of the following complications can occur with electrolyte deficient media during a procedure?
Which of the following complications can occur with electrolyte deficient media during a procedure?
Electrolyte rich media can be used with both unipolar and bipolar instruments.
Electrolyte rich media can be used with both unipolar and bipolar instruments.
What is the maximum pressure inside the uterus during a procedure?
What is the maximum pressure inside the uterus during a procedure?
In cases of water intoxication due to electrolyte deficient media, symptoms like __________ and confusion may occur.
In cases of water intoxication due to electrolyte deficient media, symptoms like __________ and confusion may occur.
Match the following instruments with their respective characteristics:
Match the following instruments with their respective characteristics:
Flashcards are hidden until you start studying
Study Notes
Gartner's Cyst
- A swelling found on the antero-lateral wall of the vagina
- Differentiate from Bartholin's cyst, located outside the vestibule, and cystocele, a prolapse of the anterior vaginal wall
- Can be asymptomatic or cause difficulty with intercourse
- Management includes observation for asymptomatic cysts and surgical removal for symptomatic cysts
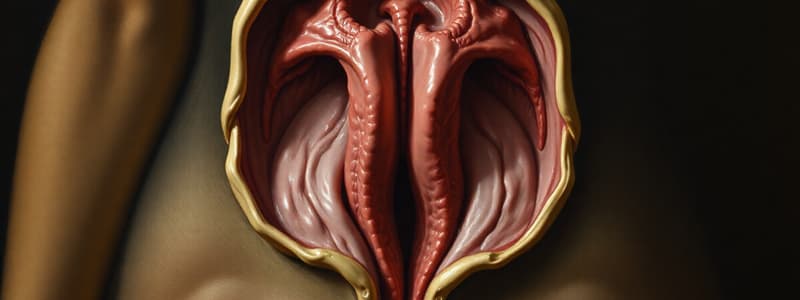
Female Internal Genitalia
- Composed of fallopian tubes, uterus, cervix, and vagina
- Develops from the fusion of the Mullerian ducts
- Initially located lateral to the vagina, then fuse from inferior to superior
- The septum resolves, forming a single uterine cavity, and the fundus of the uterus becomes dome-shaped
Development of Female Internal Genitalia
- Full fusion of Mullerian ducts completes by 10 weeks of intrauterine life
- A single uterine cavity forms by 18-20 weeks of intrauterine life
- Endometrium differentiation occurs by 20 weeks of intrauterine life
- Ovaries develop from the genital ridge
- The lower 2/3rd of the vagina develops from the urogenital sinus
Mullerian Malformations
- Result from defects in the formation and fusion of Mullerian ducts
- Often involve lateral fusion defects
- Classified by the World Health Organization (WHO) and American Society for Reproductive Medicine (ASRM)
USG in Gynecology
- First-line investigation for pelvic pathology, uterine pathology, atypical uterine bleeding, and Mullerian malformations
- 3D USG used for Mullerian malformation visualization
MRI in Gynecology
- Non-invasive and safe for pregnant women
- Best for soft tissue evaluation
- Helps differentiate between endometrium and myometrium
- Effectively visualizes the Transitional Zone (TZ)
MRI Drawbacks
- Transvaginal ultrasound (TVS) is difficult in cases of vaginal narrowing, such as in virgin females and postmenopausal women
MRI Uses
- Adenomyosis: Endometrium grows inside the myometrium, TZ size ≥ 12mm
- Endometrial carcinoma: Visualizes myometrial involvement
- Cervical cancer: Evaluates parametrial involvement
- Mullerian malformations: MRI is the gold standard
Hysteroscopy and HSG
- Hysteroscopy: A procedure to visualize the interior of the uterus for diagnosis and treatment
- Hysterosalpingography (HSG): X-ray procedure using contrast dye to visualize the uterus and fallopian tubes, assessing tubal patency and identifying filling defects
HSG Uses
- Evaluates fallopian tube patency
- Identifies Mullerian malformations
- Visualizes filling defects within the uterine cavity
HSG Filling Defects
- Polyp
- Fibroid
- Asherman's syndrome: Multiple, irregular filling defects
- Genital tuberculosis: Used in conjunction with anti-tuberculosis treatment to evaluate tube patency
Hysteroscopy Advantages
- Direct visualization of the uterine cavity
- Diagnostic and therapeutic
Hysteroscopy Disadvantages
- Cannot be used therapeutically
Hysteroscopy Procedure
- Patient position: Lithotomy
- Pain relief: Paracervical block with 1% xylocaine (diagnostic), general or regional anesthesia (therapeutic)
- Distension media: Gaseous (CO2) or liquid (absorbed by the body, requiring careful consideration)
Distention Media
- Electrolyte rich media: Ringer's lactate (RL), Normal saline (NS); Active space: Can be used with both unipolar and bipolar instruments, potential for uterine perforation
- Electrolyte deficient media: 1.5% Glycine, 3% Sorbitol, 5% Mannitol; Can be used only with both unipolar and bipolar instruments, risk of water intoxication and hyponatremia
- Normal uterine pressure: 75-80mmHg, maximum: 150mmHg
Hysteroscopy Contraindications
- Pregnancy
- Pelvic infections
- Cervical issues
- Cardiopulmonary disease
Laparoscopy
- Invasive procedure to visualize the exterior of the uterus
- Left and right sides of the patient correspond to the observer's left and right
Laparoscopy Indications
- Infertility
- Endometriosis
- Chronic pelvic pain
- Combined with hysteroscopy for comprehensive evaluation
Laparoscopy Gold Standard
- Pelvic inflammatory disease (PID)
- Tubal palsy: Laparoscopic chromopertubation
Saline Infusion Sonography (SIS)
- Procedure to visualize the uterine cavity using saline and ultrasound
- Used to diagnose polyps or submucous fibroids
SIS Procedure
- Foley's catheter distends the uterine cavity
- Saline, which appears black on ultrasound, is infused
- Pathology is visualized against the black saline background
HSG Procedure
- Water-soluble, iodinated radio-opaque dye (e.g., urograffin) is injected into the uterus via a cannula
- Serial X-rays are taken to track the dye's path
- Done in the pre-ovulatory phase (Day 7-10)
HSG Contraindications:
- Pregnancy
- Active pelvic infection
- Active genital tuberculosis (TB)
Uterine Shapes
- Normal: Pear-shaped
- Didelphys: Split into two separate compartments
- Arcuate: Flattened or curved fundus with a deeper curvature in the center of fundus
- Unicornuate: One horn
- Bicornuate: Two distinct horns
- Septate: A central septum divides the uterus into two chambers
Bicornuate vs. Septate Uterus
| Feature | Bicornuate Uterus | Septate Uterus |
|---|---|---|
| Fundus | Divided | Normal |
| Dye | Cannot differentiate | Normal |
HSG Dye
- Can delineate different sections of the uterus
- May not completely separate compartments in bicornuate and septate uteri
Angles and Distance Between Uterine Horns
- Obtuse angle and 24 cm distance between horns: Likely indicates bicornuate uterus
- Acute angle and 10 cm distance between horns: May be indicative of septate uterus
Table of Uterine Defects
| Class | Defect | Called As | Diagram | Comment |
|---|---|---|---|---|
| II | Bilateral MD present, but fail to fuse or Fusion occurs only in the region of the vagina | Uterus diadelphys; Fundus: two halves; Vagina: two halves or Single | Diagram of a uterus with two halves separated by a midline septum | Complication: Transverse lie. On HSG: 2 LW cannulae for an external os; 2 vaginas. |
| III | Longitudinal septum | Diagram of a uterus with a longitudinal septum | 2 LW cannulae; Obstructed hemivagina | |
| IV | Both MD present, only vagina & cervix fused | Bicornuate uterus; Fundus: two; Cervix: one; Vagina: one | Diagram of a bicornuate uterus | Fundus of uterus: Divided in two. On HSG: Doesn't visualize top of fundis; Cannot differentiate between bicornuate & septate uterus. |
| V | Both MD present, fusion occurs, septa fails to resolve | Septate uterus | Diagram of a septate uterus | Exteriorly: uterus appears normal. Interiorly: Septa present; Fundus: Not divided; Incomplete septa; Complete septa. |
Electrolyte Rich vs Deficient Distention Media
- Electrolyte Rich Media: Can be used only with bipolar instruments; Active space; Can lead to uterine perforation; Stop procedure when fluid deficit = 2.5L
- Electrolyte Deficient Media: Can be used only with both unipolar and bipolar instruments; Risk of water intoxication (e.g., nausea, vomiting, headache); Hyponatremia can occur (e.g., delirium, confusion) except with mannitol; Stop procedure when fluid deficit = 1L
Invasive Procedures
- SIS: Saline Infusion Sonography; Procedure to visualize the uterine cavity using saline and ultrasound; Used to diagnose polyps or submucous fibroids
- HSG: Hysterosalpingography; Procedure to visualize the uterus and fallopian tubes using X-ray with contrast dye; Used to assess tubal patency and identify filling defects
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.