Podcast
Questions and Answers
In Crohn's disease, which part of the gastrointestinal tract is most commonly affected?
In Crohn's disease, which part of the gastrointestinal tract is most commonly affected?
- The rectum
- The terminal ileum and colon (correct)
- The esophagus
- The stomach
Which of the following is a characteristic pattern of inflammation in Crohn's disease?
Which of the following is a characteristic pattern of inflammation in Crohn's disease?
- Transmural inflammation
- Inflammation limited to the mucosal layer
- Continuous inflammation from rectum upward
- Patchy or discontinuous inflammation ('skip lesions') (correct)
What type of immune response is predominantly associated with Crohn's disease?
What type of immune response is predominantly associated with Crohn's disease?
- IgE-mediated (allergic response)
- Th1-dominant (cell-mediated immunity) (correct)
- Th2-dominant (humoral immunity)
- B-cell mediated (antibody production)
A patient presents with crampy abdominal pain, non-bloody diarrhea, weight loss, and perianal fistulas. Which condition is most likely?
A patient presents with crampy abdominal pain, non-bloody diarrhea, weight loss, and perianal fistulas. Which condition is most likely?
Which of the following is a typical clinical symptom of Ulcerative Colitis (UC)?
Which of the following is a typical clinical symptom of Ulcerative Colitis (UC)?
What is the depth of inflammation typically seen in Ulcerative Colitis (UC)?
What is the depth of inflammation typically seen in Ulcerative Colitis (UC)?
Which of the following extraintestinal manifestations is commonly associated with both Crohn's disease and Ulcerative Colitis?
Which of the following extraintestinal manifestations is commonly associated with both Crohn's disease and Ulcerative Colitis?
Which of the following complications is more common in Crohn's disease than in Ulcerative Colitis?
Which of the following complications is more common in Crohn's disease than in Ulcerative Colitis?
What is the primary difference between diverticulosis and diverticulitis?
What is the primary difference between diverticulosis and diverticulitis?
Which of the following is a risk factor associated with the development of diverticulosis?
Which of the following is a risk factor associated with the development of diverticulosis?
A patient presents with LLQ abdominal pain, fever, and leukocytosis. Which condition is most likely?
A patient presents with LLQ abdominal pain, fever, and leukocytosis. Which condition is most likely?
Which complication is LEAST likely to arise from diverticulitis?
Which complication is LEAST likely to arise from diverticulitis?
In the context of appendicitis, what is the most common initiating factor in its pathophysiology?
In the context of appendicitis, what is the most common initiating factor in its pathophysiology?
What is the typical progression of pain in appendicitis?
What is the typical progression of pain in appendicitis?
Which physical exam finding is highly suggestive of appendicitis?
Which physical exam finding is highly suggestive of appendicitis?
Which of the following lab results would you expect to see in a patient with appendicitis?
Which of the following lab results would you expect to see in a patient with appendicitis?
A key distinction between Ulcerative Colitis and Crohn's disease lies in the pattern and depth of inflammation. If a biopsy report indicates 'transmural inflammation with skip lesions,' which condition is most likely?
A key distinction between Ulcerative Colitis and Crohn's disease lies in the pattern and depth of inflammation. If a biopsy report indicates 'transmural inflammation with skip lesions,' which condition is most likely?
A patient with known Crohn's disease presents with signs of B12 deficiency and steatorrhea. Where in the GI tract is the disease most likely active and causing these symptoms?
A patient with known Crohn's disease presents with signs of B12 deficiency and steatorrhea. Where in the GI tract is the disease most likely active and causing these symptoms?
A researcher is studying the pathogenesis of Inflammatory Bowel Disease (IBD). They hypothesize that a specific genetic mutation leads to a dysfunctional NOD2 receptor, predisposing individuals to Crohn's Disease. How would this affect the immune response in the gut?
A researcher is studying the pathogenesis of Inflammatory Bowel Disease (IBD). They hypothesize that a specific genetic mutation leads to a dysfunctional NOD2 receptor, predisposing individuals to Crohn's Disease. How would this affect the immune response in the gut?
Consider a scenario where a patient presents with symptoms suggestive of diverticulitis. After initial management, the patient's condition deteriorates rapidly, exhibiting signs of systemic inflammatory response syndrome (SIRS), including high fever, tachycardia, and hypotension, alongside severe abdominal pain. Imaging reveals free air in the abdomen. Considering the patient's presentation, what is the most likely underlying complication driving the rapid deterioration?
Consider a scenario where a patient presents with symptoms suggestive of diverticulitis. After initial management, the patient's condition deteriorates rapidly, exhibiting signs of systemic inflammatory response syndrome (SIRS), including high fever, tachycardia, and hypotension, alongside severe abdominal pain. Imaging reveals free air in the abdomen. Considering the patient's presentation, what is the most likely underlying complication driving the rapid deterioration?
Flashcards
Location of Crohn's Disease
Location of Crohn's Disease
Anywhere in the GI tract, most common in the terminal ileum & colon
Location of Ulcerative Colitis
Location of Ulcerative Colitis
Begins in the rectum and extends proximally in the colon with a continuous pattern.
Inflammation pattern in Crohn's
Inflammation pattern in Crohn's
Characterized by discontinuous inflammation, also known as skip lesions.
Inflammation pattern in Ulcerative Colitis
Inflammation pattern in Ulcerative Colitis
Signup and view all the flashcards
Depth of Inflammation in Crohn's Disease
Depth of Inflammation in Crohn's Disease
Signup and view all the flashcards
Depth of Inflammation in Ulcerative Colitis
Depth of Inflammation in Ulcerative Colitis
Signup and view all the flashcards
Immune Response Type in Crohn's Disease
Immune Response Type in Crohn's Disease
Signup and view all the flashcards
Immune Response Type in Ulcerative Colitis
Immune Response Type in Ulcerative Colitis
Signup and view all the flashcards
Granulomas in Crohn's Disease
Granulomas in Crohn's Disease
Signup and view all the flashcards
Granulomas in Ulcerative Colitis
Granulomas in Ulcerative Colitis
Signup and view all the flashcards
Fistula & Perforation in Crohn's Disease
Fistula & Perforation in Crohn's Disease
Signup and view all the flashcards
Diverticulosis
Diverticulosis
Signup and view all the flashcards
Diverticulitis
Diverticulitis
Signup and view all the flashcards
Clinical Manifestations of Diverticulitis
Clinical Manifestations of Diverticulitis
Signup and view all the flashcards
Pathophysiology of Appendicitis
Pathophysiology of Appendicitis
Signup and view all the flashcards
Clinical Manifestations of Appendicitis
Clinical Manifestations of Appendicitis
Signup and view all the flashcards
Symptoms of Appendicitis
Symptoms of Appendicitis
Signup and view all the flashcards
Physical Exam Findings in Appendicitis
Physical Exam Findings in Appendicitis
Signup and view all the flashcards
Study Notes
- Crohn's Disease (CD) and Ulcerative Colitis (UC) are inflammatory diseases with distinct characteristics.
Crohn's Disease (CD)
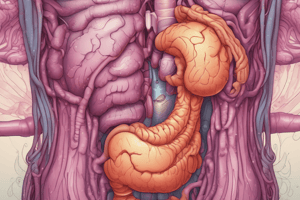
- Can occur anywhere in the GI tract, most commonly in the terminal ileum and colon.
- Pattern of inflammation is discontinuous ("skip lesions").
- Inflammation is transmural, affecting the entire bowel wall.
- Immune response is Th1-dominant (cell-mediated immunity).
- Granulomas are commonly present, and are non-caseating.
- Fistulas and perforations are common due to deep ulcers and transmural inflammation.
- Strictures and obstruction are common due to fibrosis and thickening of the intestinal wall.
- Increased risk of colorectal cancer, especially with longstanding disease.
- Clinical symptoms include crampy abdominal pain, diarrhea (often non-bloody), weight loss, B12 deficiency (ileal involvement), and perianal disease (fissures, abscesses, fistulae).
- Extra-intestinal manifestations include arthritis, uveitis, and skin lesions like erythema nodosum, and gallstones.
Ulcerative Colitis (UC)
- Begins in the rectum and extends proximally in the colon (continuous pattern).
- Inflammation is continuous from the rectum upwards.
- Affects only the mucosal and submucosal layers.
- Immune response is Th2-dominant (humoral immunity).
- Granulomas are rare.
- Fistulas and perforations are rare.
- Strictures and obstruction are less common.
- Increased risk of colorectal cancer correlates with the duration and severity of the disease.
- Clinical symptoms include bloody diarrhea, urgency to defecate, tenesmus, and cramping, often in the LLQ.
- Extra-intestinal manifestations are similar to Crohn's disease, including skin, joints, and eyes.
Diverticulosis
- Defined by the presence of diverticula, which are outpouchings of the mucosa/submucosa through the muscular wall, typically in the sigmoid colon.
- Usually asymptomatic.
- Common in older adults.
- Etiology is linked to increased intraluminal pressure, age, low-fiber diets, obesity, and a sedentary lifestyle, but not primarily caused by fiber deficiency.
Diverticulitis
- Characterized by inflammation or infection of one or more diverticula.
- Affects about 10-15% of individuals with diverticulosis.
- Can lead to complications such as abscess, fistula, obstruction, and perforation.
- Clinical manifestations include LLQ abdominal pain (common in sigmoid disease), fever, leukocytosis, nausea, vomiting, constipation or diarrhea, rebound tenderness, and guarding.
Appendicitis Pathophysiology
- Obstruction of the appendiceal lumen is the most common initiating factor, caused by fecaliths (hardened stool), lymphoid hyperplasia, foreign bodies, or tumors.
- Obstruction leads to bacterial overgrowth, inflammation, and ischemia.
- Can progress to necrosis, perforation, and peritonitis if untreated.
Appendicitis Clinical Manifestations
- Initial vague abdominal pain localizes to the RLQ (McBurney's point).
- Fever, nausea, and vomiting occur.
- Rebound tenderness, guarding, and positive Rovsing's or psoas sign are present.
- Anorexia is common.
- Elevated WBC count with a left shift.
- Pain intensifies with movement or coughing.
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.