Podcast
Questions and Answers
A 28-year-old female presents with abdominal pain and diarrhea. Endoscopic findings reveal discontinuous areas of inflammation in the terminal ileum and cecum. Which of the following pathological features is most indicative of Crohn's disease?
A 28-year-old female presents with abdominal pain and diarrhea. Endoscopic findings reveal discontinuous areas of inflammation in the terminal ileum and cecum. Which of the following pathological features is most indicative of Crohn's disease?
- Continuous superficial ulceration of the mucosa
- Diffuse infiltration of neutrophils in the lamina propria
- Focal intestinal inflammation with skip lesions (correct)
- Formation of pseudopolyps
A 35-year-old male with Crohn's disease develops a fever and severe abdominal pain. Imaging reveals an intra-abdominal abscess. Which of the following is the most appropriate next step in management?
A 35-year-old male with Crohn's disease develops a fever and severe abdominal pain. Imaging reveals an intra-abdominal abscess. Which of the following is the most appropriate next step in management?
- Administration of anti-TNF-α antibodies
- High-dose corticosteroids
- Surgical drainage of the abscess (correct)
- Initiation of exclusive enteral nutrition
A 25-year-old patient with Crohn's disease is being evaluated for anemia. Lab results indicate low serum iron, vitamin B12, and folate levels. What is the most likely underlying cause of these deficiencies in the context of Crohn's disease?
A 25-year-old patient with Crohn's disease is being evaluated for anemia. Lab results indicate low serum iron, vitamin B12, and folate levels. What is the most likely underlying cause of these deficiencies in the context of Crohn's disease?
- Increased red blood cell destruction
- Malabsorption due to ileal disease (correct)
- Autoimmune destruction of parietal cells
- Dietary restriction of iron and vitamins
Which of the following is a recognized extra-intestinal manifestation associated with Crohn's disease?
Which of the following is a recognized extra-intestinal manifestation associated with Crohn's disease?
A 30-year-old male with Crohn's disease presents with recurrent perianal fistulae that are not responding to conventional treatments. Which of the following antibiotics is most specifically indicated for healing perianal fistulae in Crohn's disease?
A 30-year-old male with Crohn's disease presents with recurrent perianal fistulae that are not responding to conventional treatments. Which of the following antibiotics is most specifically indicated for healing perianal fistulae in Crohn's disease?
What is the primary mechanism of action for vedolizumab in the treatment of Crohn's disease?
What is the primary mechanism of action for vedolizumab in the treatment of Crohn's disease?
A colonoscopy report describes a 'string sign' in the terminal ileum of a patient being evaluated for abdominal pain and diarrhea. What condition does this radiographic finding most strongly suggest?
A colonoscopy report describes a 'string sign' in the terminal ileum of a patient being evaluated for abdominal pain and diarrhea. What condition does this radiographic finding most strongly suggest?
Which of the following immunological markers is most likely to be elevated in a patient with Crohn's disease, although it is less often seen compared to ulcerative colitis?
Which of the following immunological markers is most likely to be elevated in a patient with Crohn's disease, although it is less often seen compared to ulcerative colitis?
A 22-year-old patient with Crohn's disease presents with symptoms suggestive of small bowel obstruction. Which of the following is a common cause of small bowel obstruction in Crohn's disease?
A 22-year-old patient with Crohn's disease presents with symptoms suggestive of small bowel obstruction. Which of the following is a common cause of small bowel obstruction in Crohn's disease?
What is the primary goal of nutritional therapy in managing Crohn's disease?
What is the primary goal of nutritional therapy in managing Crohn's disease?
A patient with Crohn's disease presents with symptoms of fatigue, glossitis, and peripheral neuropathy. Which of the following is the most likely cause of these symptoms, considering common deficiencies associated with Crohn's disease?
A patient with Crohn's disease presents with symptoms of fatigue, glossitis, and peripheral neuropathy. Which of the following is the most likely cause of these symptoms, considering common deficiencies associated with Crohn's disease?
A 45-year-old male with a long-standing history of Crohn's disease presents with new onset jaundice, elevated alkaline phosphatase, and fatigue. Imaging reveals inflammation and fibrosis of the bile ducts. Which of the following is the most likely diagnosis?
A 45-year-old male with a long-standing history of Crohn's disease presents with new onset jaundice, elevated alkaline phosphatase, and fatigue. Imaging reveals inflammation and fibrosis of the bile ducts. Which of the following is the most likely diagnosis?
A 32-year-old female with Crohn's disease is being treated with azathioprine. She reports persistent nausea and elevated liver enzymes. Which of the following is the most appropriate next step in managing this patient?
A 32-year-old female with Crohn's disease is being treated with azathioprine. She reports persistent nausea and elevated liver enzymes. Which of the following is the most appropriate next step in managing this patient?
In a patient with Crohn's disease, which of the following findings on a barium follow-through study would be most indicative of long-standing, chronic disease, rather than an acute inflammatory process?
In a patient with Crohn's disease, which of the following findings on a barium follow-through study would be most indicative of long-standing, chronic disease, rather than an acute inflammatory process?
A patient with Crohn's disease develops abdominal pain, distension, and signs of peritonitis. Imaging reveals free air in the abdomen. Which of the following is the most likely underlying cause?
A patient with Crohn's disease develops abdominal pain, distension, and signs of peritonitis. Imaging reveals free air in the abdomen. Which of the following is the most likely underlying cause?
A researcher is investigating the genetic basis of Crohn's disease. Which of the following genetic findings would provide the strongest evidence for a significant genetic component in the disease etiology?
A researcher is investigating the genetic basis of Crohn's disease. Which of the following genetic findings would provide the strongest evidence for a significant genetic component in the disease etiology?
A 29-year-old female with Crohn's disease is planning a pregnancy. She is currently in remission on vedolizumab. Which of the following is the most appropriate recommendation regarding her medication?
A 29-year-old female with Crohn's disease is planning a pregnancy. She is currently in remission on vedolizumab. Which of the following is the most appropriate recommendation regarding her medication?
A patient with Crohn's disease who is on long-term corticosteroid therapy is being evaluated for bone health. Which of the following is the most appropriate initial screening test for assessing osteoporosis risk in this patient?
A patient with Crohn's disease who is on long-term corticosteroid therapy is being evaluated for bone health. Which of the following is the most appropriate initial screening test for assessing osteoporosis risk in this patient?
A patient with Crohn's disease presents with a painful, violaceous, and rapidly progressive skin ulcer on the lower extremity. Which of the following conditions is the most likely diagnosis?
A patient with Crohn's disease presents with a painful, violaceous, and rapidly progressive skin ulcer on the lower extremity. Which of the following conditions is the most likely diagnosis?
A patient with Crohn's disease is found to have iron deficiency anemia. Further workup reveals that the patient has had a partial ileectomy. What is the most appropriate treatment for this patient?
A patient with Crohn's disease is found to have iron deficiency anemia. Further workup reveals that the patient has had a partial ileectomy. What is the most appropriate treatment for this patient?
Flashcards
Crohn's Disease Definition
Crohn's Disease Definition
Chronic inflammation affecting any part of the GI tract, most often the terminal ileum.
Crohn's Disease Epidemiology
Crohn's Disease Epidemiology
Peak onset ages 20-40, slightly more common in females.
Crohn's Disease Hallmark
Crohn's Disease Hallmark
Focal, discontinuous inflammation leading to 'skip lesions'. Early lesions include aphthous ulcers.
Transmural Inflammation
Transmural Inflammation
Signup and view all the flashcards
Crohn's Extra-intestinal Symptoms
Crohn's Extra-intestinal Symptoms
Signup and view all the flashcards
Crohn's Lab Findings
Crohn's Lab Findings
Signup and view all the flashcards
Elevated Fecal calprotectin or lactoferrin
Elevated Fecal calprotectin or lactoferrin
Signup and view all the flashcards
Colonoscopy in Crohn's
Colonoscopy in Crohn's
Signup and view all the flashcards
Video capsule endoscopy
Video capsule endoscopy
Signup and view all the flashcards
Corticosteroids for Treatment
Corticosteroids for Treatment
Signup and view all the flashcards
Crohn's Disease Pathogenesis
Crohn's Disease Pathogenesis
Signup and view all the flashcards
Non-caseating granulomas
Non-caseating granulomas
Signup and view all the flashcards
Anemia in Crohn's disease
Anemia in Crohn's disease
Signup and view all the flashcards
Crohn's Disease Imaging option
Crohn's Disease Imaging option
Signup and view all the flashcards
Barium follow-through Crohn's
Barium follow-through Crohn's
Signup and view all the flashcards
Antibiotics in Crohn's Treatment
Antibiotics in Crohn's Treatment
Signup and view all the flashcards
Nutritional Therapy
Nutritional Therapy
Signup and view all the flashcards
Surgery indications (CD)
Surgery indications (CD)
Signup and view all the flashcards
Crohn's disease features.
Crohn's disease features.
Signup and view all the flashcards
Study Notes
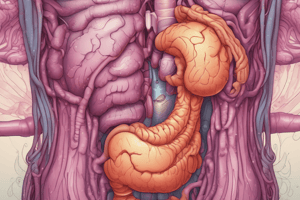
- Crohn's Disease is a chronic inflammatory condition affecting any part of the gastrointestinal tract, most frequently the terminal ileum.
- Slightly more common in females.
Epidemiology
- Peak onset occurs between ages 20-40, with a smaller peak in older adults.
Etiology & Pathogenesis
- Tissue inflammation results from an abnormal immune response to bacterial antigens in the gut lumen.
- It has a strong genetic component, with high concordance among monozygotic twins, along with diet and smoking playing a role.
Pathology
- In 40% of cases, it affects the terminal ileum and cecum
- 20% affects the colon only
- 30% affects the ileum and colon
- 10% affects any part of the GIT, perianal disease, mouth, esophagus, and stomach.
- The hallmark is focal intestinal inflammation and discontinuous disease, leading to 'skip lesions'.
Early Lesions
- Include aphthous ulcers.
- Non-caseating granulomas are present in up to 70% of cases.
- Inflammation is transmural, leading to large ulcers, sinus tracks, fissures, and fistulae.
- Healing leads to extensive fibrosis
Clinical Features
- Symptoms are abdominal pain, diarrhea, weight loss, anorexia, and fever
- Growth retardation is common in children.
- Anemia occurs in 30%, often due to iron, B12, or folate deficiency
- Small bowel obstruction may occur due to strictures
- Colonic Crohn's disease may present with bloody diarrhea.
- Gastroduodenal Crohn's can present as Helicobacter-negative peptic ulcer disease.
- Intestinal affection may be inflammatory, stricturing, or penetrating.
Extra-Intestinal Manifestations
- Arthropathy (including sacroiliitis), with large joints predominantly affected
- Association with ankylosing spondylitis in HLA-B27 patients
- Metabolic bone disease: osteopenia
- Venous and arterial thromboembolic disease
- Skin manifestations: pyoderma gangrenosum and erythema nodosum
- Ocular manifestations: Scleritis, episcleritis, and anterior uveitis
- Gallstones
- Fatty liver, autoimmune hepatitis and primary sclerosing cholangitis
- Renal oxalate stones
Laboratory Investigations
- CBC indicates anemia, increased WBC, and increased platelets.
- Decreased serum iron, B12, and folate levels.
- LFTs show low serum albumin and high CRP.
- Low calcium, magnesium, and zinc levels.
- Stool tests are performed, including stool culture and sensitivity as well as testing for Clostridioides difficile toxin, to exclude infectious colitis.
Differentiation Between IBD and IBS
- Elevated fecal calprotectin or lactoferrin can differentiate between IBD and IBS.
- Immunological markers: ASCA found in up to 50% of Crohn's but less often in Ulcerative Colitis
- p-ANCA is found in 70% of UC but only 15% of Crohn's
Imaging
- Colonoscopy is the gold standard for diagnosing colonic and terminal ileal disease, allowing for mucosal biopsy
- Video capsule endoscopy visualizes all parts of the GIT to detect lesions not visible in other imaging
- Barium follow-through: Standard method for evaluating the small bowel, largely replaced by US, CT, and MRI. A "string sign" can be observed when using this method.
- Small bowel US detects thickened terminal ileum wall, abscesses, and fistulae
- CT enterography is useful in evaluating small bowel disease
- MRI enterography is better than CT for detecting strictures
Treatment
- Corticosteroids are used for rapidly inducing remission, but not as long-term therapy.
- Budesonide is nearly as effective as prednisolone, with fewer side effects.
- Azathioprine or methotrexate are widely used in patients with active CD who fail to taper steroids and require several weeks for action.
- Aminosalicylates like mesalazine are used in treating colonic disease.
- Anti-TNF α antibodies: Infliximab IV infusions and Adalimumab SC.
- Anti-integrin therapy: Vedolizumab.
- Anti-IL-12/IL-23 therapy: Ustekinumab.
Other Novel Oral Therapies
- Tofacitinib selective JAK inhibitors are given orally.
- Metronidazole heals perianal fistulae
- Ciprofloxacin is used in treating complications with good effect
Nutritional Therapy
- Corrects nutritional deficiency
- Elemental diets induce disease remission
Surgery Indications
- Intra-abdominal masses
- Fistulae
- Fibrotic strictures with obstruction
- Toxic megacolon
- Hemorrhage
- Cancer
- Surgical treatment is for complications such as stricture and is not a cure.
Ulcerative Colitis vs Crohn's Disease
- Site of Origin: Terminal ileum in Crohn's, rectum in Ulcerative Colitis
- Pattern of Progression: Skip lesions/irregular in Crohn's, proximally contiguous in Ulcerative Colitis
- Thickness of Inflammation: Transmural in Crohn's, submucosa or mucosa in Ulcerative Colitis
- Symptoms: Crampy abdominal pain in Crohn's, bloody diarrhea in Ulcerative Colitis
- Complications: Fistulas, abscess, obstruction in Crohn's, hemorrhage, toxic megacolon in Ulcerative Colitis
- Radiographic Findings: String sign on barium X-ray in Crohn's, lead pipe colon on barium X-ray in Ulcerative Colitis
- Risk of Colon Cancer: Slightly increased in Crohn's, markedly increased in Ulcerative Colitis
- Surgery: For complications such as stricture in Crohn's, curative in Ulcerative Colitis
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.