Podcast
Questions and Answers
What condition may individuals with diabetes experience when changing positions from sitting or lying down to standing up?
What condition may individuals with diabetes experience when changing positions from sitting or lying down to standing up?
- Orthostatic hypertension
- Chronic fatigue
- Cardiac dysrhythmia
- Postural hypotension (correct)
What is one potential symptom of postural hypotension in people with diabetes?
What is one potential symptom of postural hypotension in people with diabetes?
- Increased heart rate at rest
- Dizziness upon standing (correct)
- Severe headaches
- Rapid weight gain
In which situation is postural hypotension most likely to occur for individuals with diabetes?
In which situation is postural hypotension most likely to occur for individuals with diabetes?
- While standing still for long periods
- When going from sitting or lying down to standing up (correct)
- During a meal
- After intense physical exercise
Why might people with diabetes experience postural hypotension?
Why might people with diabetes experience postural hypotension?
What is the primary characteristic of postural hypotension?
What is the primary characteristic of postural hypotension?
What is one of the main functions of the kidneys in the short term?
What is one of the main functions of the kidneys in the short term?
How does short-term regulation by the kidneys differ from long-term regulation?
How does short-term regulation by the kidneys differ from long-term regulation?
What characterizes the short-term role of the kidneys in blood pressure regulation?
What characterizes the short-term role of the kidneys in blood pressure regulation?
Which statement best describes the duration of influence for the kidneys' short-term regulation?
Which statement best describes the duration of influence for the kidneys' short-term regulation?
In what way do the kidneys regulate arterial pressure in the short term?
In what way do the kidneys regulate arterial pressure in the short term?
What is the primary function of angiotensin converting enzyme (ACE) in the lungs?
What is the primary function of angiotensin converting enzyme (ACE) in the lungs?
Which one of the following statements about angiotensin 2 is true?
Which one of the following statements about angiotensin 2 is true?
What effect does angiotensin 2 have on blood vessels?
What effect does angiotensin 2 have on blood vessels?
Which of the following is NOT a result of the action of angiotensin 2?
Which of the following is NOT a result of the action of angiotensin 2?
What is the sequence of steps that leads to the production of angiotensin 2?
What is the sequence of steps that leads to the production of angiotensin 2?
What two factors does mean arterial pressure depend on?
What two factors does mean arterial pressure depend on?
What is the significance of having questions or concerns in the context of this document?
What is the significance of having questions or concerns in the context of this document?
How does the total peripheral resistance (TPR) affect blood flow?
How does the total peripheral resistance (TPR) affect blood flow?
Who authored this document on arterial pressure control?
Who authored this document on arterial pressure control?
What does the abbreviation 'Abbreviation' likely refer to in this context?
What does the abbreviation 'Abbreviation' likely refer to in this context?
Which statement accurately reflects the role of total peripheral resistance in the vascular system?
Which statement accurately reflects the role of total peripheral resistance in the vascular system?
In terms of blood flow regulation, what is the relationship between mean arterial pressure and total peripheral resistance?
In terms of blood flow regulation, what is the relationship between mean arterial pressure and total peripheral resistance?
What action is implied by the phrase 'If you have any questions or concerns'?
What action is implied by the phrase 'If you have any questions or concerns'?
Which of the following factors would NOT affect mean arterial pressure?
Which of the following factors would NOT affect mean arterial pressure?
What might be the primary intent of this document regarding arterial pressure?
What might be the primary intent of this document regarding arterial pressure?
What triggers the secretion of renin from the kidneys?
What triggers the secretion of renin from the kidneys?
Which cells in the kidney are responsible for secreting renin?
Which cells in the kidney are responsible for secreting renin?
What is the role of angiotensinogen in the RAAS?
What is the role of angiotensinogen in the RAAS?
Where is angiotensinogen produced in the body?
Where is angiotensinogen produced in the body?
Which of the following is NOT a component of the RAAS?
Which of the following is NOT a component of the RAAS?
Flashcards
Arterial Pressure
Arterial Pressure
Arterial pressure is the pressure of blood in the arteries, the blood vessels that carry blood away from the heart.
Control of Arterial Pressure
Control of Arterial Pressure
The regulation and control of blood pressure within a healthy range.
Key Information
Key Information
Information, often presented concisely, used to highlight important points in a document.
Abbreviation
Abbreviation
Signup and view all the flashcards
Explanation
Explanation
Signup and view all the flashcards
Postural Hypotension
Postural Hypotension
Signup and view all the flashcards
Diabetes
Diabetes
Signup and view all the flashcards
Low Blood Pressure
Low Blood Pressure
Signup and view all the flashcards
Postural Hypotension in Diabetes
Postural Hypotension in Diabetes
Signup and view all the flashcards
Transitioning from Sitting or Lying to Standing
Transitioning from Sitting or Lying to Standing
Signup and view all the flashcards
Mean Arterial Pressure (MAP)
Mean Arterial Pressure (MAP)
Signup and view all the flashcards
Total Peripheral Resistance (TPR)
Total Peripheral Resistance (TPR)
Signup and view all the flashcards
Factors influencing MAP
Factors influencing MAP
Signup and view all the flashcards
Function of the Vascular System
Function of the Vascular System
Signup and view all the flashcards
Blood flow regulation
Blood flow regulation
Signup and view all the flashcards
Short-Term Blood Pressure Regulation by Kidneys
Short-Term Blood Pressure Regulation by Kidneys
Signup and view all the flashcards
Long-Term Blood Pressure Regulation by Kidneys
Long-Term Blood Pressure Regulation by Kidneys
Signup and view all the flashcards
Mean Arterial Pressure
Mean Arterial Pressure
Signup and view all the flashcards
Renal Regulation of Blood Pressure
Renal Regulation of Blood Pressure
Signup and view all the flashcards
Pulse Pressure
Pulse Pressure
Signup and view all the flashcards
Renin
Renin
Signup and view all the flashcards
Angiotensinogen
Angiotensinogen
Signup and view all the flashcards
Angiotensin I
Angiotensin I
Signup and view all the flashcards
Angiotensin II
Angiotensin II
Signup and view all the flashcards
Aldosterone
Aldosterone
Signup and view all the flashcards
What enzyme converts angiotensin I to angiotensin II?
What enzyme converts angiotensin I to angiotensin II?
Signup and view all the flashcards
What is the effect of Angiotensin II on blood vessels?
What is the effect of Angiotensin II on blood vessels?
Signup and view all the flashcards
What hormones does Angiotensin II stimulate the release of?
What hormones does Angiotensin II stimulate the release of?
Signup and view all the flashcards
What is the effect of aldosterone on blood volume and pressure?
What is the effect of aldosterone on blood volume and pressure?
Signup and view all the flashcards
What is the effect of ADH (antidiuretic hormone) on blood volume and pressure?
What is the effect of ADH (antidiuretic hormone) on blood volume and pressure?
Signup and view all the flashcards
Study Notes
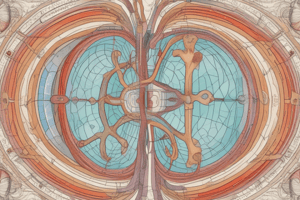
Control of Arterial Pressure II
- Objectives: Understand blood pressure regulation, components of the baroreceptor reflex, and the role of kidneys in regulation.
- Blood Pressure Definition: Pressure exerted by blood on vessel walls while flowing.
- Blood Pressure Formula: BP = CO × TPR (Cardiac output x Total peripheral resistance).
- Resistance Factors: Resistance is directly proportional to length and viscosity, inversely proportional to radius.
- Blood Pressure Measurement: Force applied to artery walls.
- Clinical Blood Pressure Units: Systolic over Diastolic (e.g., 120/80 mmHg).
- Normal Blood Pressure Ranges: Non-diabetic adults: Systolic 100-140, Diastolic 60-90 mmHg; Diabetic adults: Systolic 100-130, Diastolic 60-85 mmHg.
- Mean Arterial Pressure (MAP): 90-100 mmHg.
- Diabetic Patients: Slightly lower blood pressure, diabetes is a major coronary artery disease risk factor.
- Postural Hypotension: Low blood pressure during transitions from sitting/lying to standing.
- Autonomic Nervous System in BP Regulation: The sympathetic nervous system constricts blood vessels (vasoconstriction), hormones such as epinephrine, norepinephrine, and angiotensin II also cause vasoconstriction.
- Viscosity and Angiogenesis in Hypertension: Increased viscosity (e.g., in polycythemia/hyperproteinemia) and angiogenesis increase resistance.
- Poiseuille's Law: Smaller radius results in higher resistance.
- Short-Term Blood Pressure Control: Regulates mean arterial pressure constantly. This includes baroreceptors, chemoreceptors, CNS ischemic response, abdominal compression reflex, and Cushing reaction.
- Baroreceptors: Pressure-sensitive receptors in carotid and aortic arteries; respond to pressure changes (MAP); involved in maintaining MAP during posture changes.
- Chemoreceptors: Located in carotid & aortic bodies, respond to changes in blood chemistry (pH, O2, CO2).
- CNS Ischemic Response: Activation of sympathetic vasoconstrictor system when blood flow to brain decreases (MAP <60mmHg).
- Long-Term Blood Pressure Regulation: Kidneys play a crucial role (RAAS).
- Renin-Angiotensin-Aldosterone System (RAAS) :Renin converts angiotensinogen to angiotensin I; then to angiotensin II (strongest vasoconstrictor); stimulates aldosterone & ADH release.
- Cardiac Output: Dependent on heart rate (HR) and stroke volume (SV).
- Stroke Volume: Volume of blood pumped in one ventricular contraction, influenced by EDV (end-diastolic volume).
Baroreceptor Reflex
- Receptor: Located in the carotid sinus and aortic arch.
- Afferent Pathway: Nerve impulses to the cardiovascular center in the medulla oblongata.
- Integrating Center: The cardiovascular center in the medulla oblongata processes the information.
- Efferent Pathway: Sends signals to the heart and blood vessels via the sympathetic and parasympathetic nervous systems.
- Effector Organ: The heart, blood vessels.
- Mechanism of Action : When blood pressure decreases, baroreceptors fire less frequently, and sympathetic activity increases, causing vasoconstriction and increasing heart rate to elevate blood pressure. If blood pressure is high, baroreceptor activity increases, and sympathetic activity decreases, promoting vasodilation and decreasing heart rate to reduce blood pressure.
Types of Baroreceptors
- Type A (carotid sinus): High sensitivity, high firing rate.
- Type C (aortic): Lower sensitivity, lower firing rate, higher threshold.
Chemoreceptor Reflex
- Stimulus: Responds to changes in blood chemistry (O2, CO2, H+).
- Mechanism: Chemoreceptors signal the cardiovascular center when blood flow (due to lowered MAP) is reduced; stimulating sympathetic activity, which causes vasoconstriction in attempt to elevate blood pressure.
- Response: Increased respiratory activity (breathing) to reduce CO2 and H+ levels, increase in vasoconstriction to maintain blood pressure.
CNS Ischemic Response
- Stimulus: Reduced blood flow to the brain (low MAP).
- Mechanism: Leads to increased sympathetic activity & vasoconstriction, especially in kidney arterioles.
- Response: Prevents further decrease in blood pressure to the brain.
Importance of Blood Pressure Regulation
- Supply of Nutrients & Gases: Ensures adequate delivery of essential substances to cells.
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.