Podcast
Questions and Answers
Which of the following properties of the ground substance in connective tissue contributes most to its function as a barrier against the penetration of invaders?
Which of the following properties of the ground substance in connective tissue contributes most to its function as a barrier against the penetration of invaders?
- Its high concentration of glycoproteins.
- Its abundance of collagen fibers.
- Its crystalline structure.
- Its viscous nature. (correct)
What aspect of collagen structure primarily determines its high tensile strength and resistance to tearing forces?
What aspect of collagen structure primarily determines its high tensile strength and resistance to tearing forces?
- The random arrangement of collagen fibers allowing multidirectional flexibility.
- The high concentration of elastin, providing elasticity alongside strength.
- The presence of glycosaminoglycans (GAGs) within the collagen matrix.
- The hierarchical organization from individual molecules to fibrils, fibers, and bundles. (correct)
How do multiadhesive glycoproteins contribute to the overall stability and function of the extracellular matrix (ECM)?
How do multiadhesive glycoproteins contribute to the overall stability and function of the extracellular matrix (ECM)?
- By regulating the hydration levels within the ground substance.
- By providing binding sites for cell surface receptors and other matrix macromolecules. (correct)
- By initiating the synthesis of collagen and elastin fibers.
- By cross-linking collagen fibers to each other.
What is the primary functional difference between fibroblasts and myofibroblasts in connective tissue?
What is the primary functional difference between fibroblasts and myofibroblasts in connective tissue?
How does the structural arrangement of collagen fibers in dense regular connective tissue contribute to its specific function?
How does the structural arrangement of collagen fibers in dense regular connective tissue contribute to its specific function?
What distinguishes resident connective tissue cells from wandering connective tissue cells?
What distinguishes resident connective tissue cells from wandering connective tissue cells?
Which characteristic of reticular fibers is crucial for their role in supporting hemopoietic tissues and lymphoid organs?
Which characteristic of reticular fibers is crucial for their role in supporting hemopoietic tissues and lymphoid organs?
What role do glycosaminoglycans (GAGs) play in maintaining the structural integrity and functionality of the ECM?
What role do glycosaminoglycans (GAGs) play in maintaining the structural integrity and functionality of the ECM?
What mechanism allows leukocytes to enter connective tissue from blood vessels during an inflammatory response?
What mechanism allows leukocytes to enter connective tissue from blood vessels during an inflammatory response?
What is the primary clinical significance of understanding collagen synthesis in the context of diseases like Ehlers-Danlos syndrome and Osteogenesis Imperfecta?
What is the primary clinical significance of understanding collagen synthesis in the context of diseases like Ehlers-Danlos syndrome and Osteogenesis Imperfecta?
How does the unique structure of elastin contribute to the overall function of elastic fibers?
How does the unique structure of elastin contribute to the overall function of elastic fibers?
In the context of wound healing, what is the primary role of myofibroblasts, and how does their function contribute to tissue regeneration?
In the context of wound healing, what is the primary role of myofibroblasts, and how does their function contribute to tissue regeneration?
Which molecular component of the basal lamina is crucial for anchoring it to the underlying reticular lamina, and what type of collagen is it composed of?
Which molecular component of the basal lamina is crucial for anchoring it to the underlying reticular lamina, and what type of collagen is it composed of?
In the assembly of collagen molecules, what is the primary functional significance of disulfide bonds formed in the endoplasmic reticulum (ER)?
In the assembly of collagen molecules, what is the primary functional significance of disulfide bonds formed in the endoplasmic reticulum (ER)?
What best describes the process by which the subunits for fibrillar collagens join to become large fibrils, and how are these structures viewed under a microscope?
What best describes the process by which the subunits for fibrillar collagens join to become large fibrils, and how are these structures viewed under a microscope?
In what way do the functions of mast cells and plasma cells differentiate in connective tissue?
In what way do the functions of mast cells and plasma cells differentiate in connective tissue?
What is the clinical relevance of the high degree of hydration maintained by GAGs in the ground substance of connective tissue?
What is the clinical relevance of the high degree of hydration maintained by GAGs in the ground substance of connective tissue?
What is the primary distinction between dense irregular and dense regular connective tissues?
What is the primary distinction between dense irregular and dense regular connective tissues?
How does the disruption of the typical microfibril arrangement in elastic fibers impact tissue function, and which protein is primarily involved in this arrangement?
How does the disruption of the typical microfibril arrangement in elastic fibers impact tissue function, and which protein is primarily involved in this arrangement?
What is the developmental origin of connective tissue cells, and from which embryonic tissue do they primarily arise?
What is the developmental origin of connective tissue cells, and from which embryonic tissue do they primarily arise?
What is the role of fibronectin in the adhesion and migration of cells within the extracellular matrix (ECM)?
What is the role of fibronectin in the adhesion and migration of cells within the extracellular matrix (ECM)?
Following an injury, why is regulated inflammation crucial in the initial phases of tissue repair, and how do mast cells contribute to this process?
Following an injury, why is regulated inflammation crucial in the initial phases of tissue repair, and how do mast cells contribute to this process?
Which of the following best describes the structural organization of the basal lamina and its interactions with adjacent tissues?
Which of the following best describes the structural organization of the basal lamina and its interactions with adjacent tissues?
What is the significance of identifying the altered ratios of collagen types I and III, and during which biological process is it most relevant?
What is the significance of identifying the altered ratios of collagen types I and III, and during which biological process is it most relevant?
What property defines a tissue as 'loose connective tissue'?
What property defines a tissue as 'loose connective tissue'?
What distinctive characteristic of mucoid connective tissue sets it apart from other types of embryonic connective tissue?
What distinctive characteristic of mucoid connective tissue sets it apart from other types of embryonic connective tissue?
How does the structural arrangement of reticular fibers support their function in hemopoietic tissues and lymphoid organs?
How does the structural arrangement of reticular fibers support their function in hemopoietic tissues and lymphoid organs?
How is the role of histamine released from mast cells best described, and what downstream effects result because of it?
How is the role of histamine released from mast cells best described, and what downstream effects result because of it?
Which cells make and help preserve blood-forming cells and produce many secretory products in lymphoid organs?
Which cells make and help preserve blood-forming cells and produce many secretory products in lymphoid organs?
What are the key structural and functional components that compose the basement membrane?
What are the key structural and functional components that compose the basement membrane?
ECM components of the basal lamina includes glycoproteins which self-assemble as a network below the cell poles, how do cells adhere with these networks?
ECM components of the basal lamina includes glycoproteins which self-assemble as a network below the cell poles, how do cells adhere with these networks?
How does ground substance contribute to its function as a 'lubricant' and describe a potential clinical implication if this function is aberrant?
How does ground substance contribute to its function as a 'lubricant' and describe a potential clinical implication if this function is aberrant?
What best describes the unique roles that collagen and elastin contribute to the functional properties of tissues?
What best describes the unique roles that collagen and elastin contribute to the functional properties of tissues?
What is 'mucoid connective tissue', where is it typically found and can it be found in adults?
What is 'mucoid connective tissue', where is it typically found and can it be found in adults?
Type III collagen forms a 3D network structure in specialized reticular connective tissue, what cell type is closely associated with these type III collagen networks?
Type III collagen forms a 3D network structure in specialized reticular connective tissue, what cell type is closely associated with these type III collagen networks?
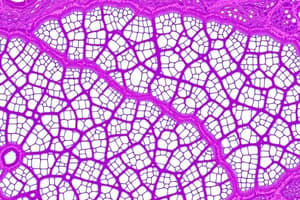
Under a microscope, what features best differentiates loose connective tissue from dense connective tissue.
Under a microscope, what features best differentiates loose connective tissue from dense connective tissue.
Given that ground substance acts a barrier that reduces diffusion of large molecules, what role does interstitial fluid perform to supplement the ground substance?
Given that ground substance acts a barrier that reduces diffusion of large molecules, what role does interstitial fluid perform to supplement the ground substance?
Flashcards
Connective Tissue Function
Connective Tissue Function
Tissue that encloses, connects, supports, cushions, and transports within the body.
Extracellular Matrix (ECM)
Extracellular Matrix (ECM)
A matrix is the major non-cellular constituent of connective tissue. It consists of protein fibers and ground substance
3 components of connective tissue
3 components of connective tissue
Cells, fibers, and ground substance.
Role of capillaries
Role of capillaries
Signup and view all the flashcards
Resident vs. Wandering Cells
Resident vs. Wandering Cells
Signup and view all the flashcards
Fibroblasts
Fibroblasts
Signup and view all the flashcards
Myofibroblasts
Myofibroblasts
Signup and view all the flashcards
Adipocytes
Adipocytes
Signup and view all the flashcards
Leukocytes
Leukocytes
Signup and view all the flashcards
Macrophages
Macrophages
Signup and view all the flashcards
Mast Cells
Mast Cells
Signup and view all the flashcards
Plasma Cells
Plasma Cells
Signup and view all the flashcards
Three main types of fibers found in connective tissue.
Three main types of fibers found in connective tissue.
Signup and view all the flashcards
Collagen
Collagen
Signup and view all the flashcards
Fibrillar collagens
Fibrillar collagens
Signup and view all the flashcards
Collagen type I
Collagen type I
Signup and view all the flashcards
Sheet-forming collagens
Sheet-forming collagens
Signup and view all the flashcards
Linking/anchoring collagens
Linking/anchoring collagens
Signup and view all the flashcards
Reticular Fibers
Reticular Fibers
Signup and view all the flashcards
Elastic Fibers
Elastic Fibers
Signup and view all the flashcards
Elastic Fiber Composition
Elastic Fiber Composition
Signup and view all the flashcards
Elastic Fiber Properties
Elastic Fiber Properties
Signup and view all the flashcards
Ground Substance
Ground Substance
Signup and view all the flashcards
Ground substance principle classes
Ground substance principle classes
Signup and view all the flashcards
GAGs (Glycosaminoglycans)
GAGs (Glycosaminoglycans)
Signup and view all the flashcards
Proteoglycans
Proteoglycans
Signup and view all the flashcards
Multiadhesive Glycoproteins
Multiadhesive Glycoproteins
Signup and view all the flashcards
Interstitial Fluid
Interstitial Fluid
Signup and view all the flashcards
Basement Membrane
Basement Membrane
Signup and view all the flashcards
Entactin/nidogen
Entactin/nidogen
Signup and view all the flashcards
Mesenchyme
Mesenchyme
Signup and view all the flashcards
Types of Connective Tissue
Types of Connective Tissue
Signup and view all the flashcards
Loose (Areolar) Connective Tissue
Loose (Areolar) Connective Tissue
Signup and view all the flashcards
Dense Irregular Connective Tissue
Dense Irregular Connective Tissue
Signup and view all the flashcards
Dense Regular CT
Dense Regular CT
Signup and view all the flashcards
Reticular Tissue
Reticular Tissue
Signup and view all the flashcards
Mucoid Connective Tissue
Mucoid Connective Tissue
Signup and view all the flashcards
Study Notes
Connective Tissue Overview
- Connective tissue is present in a range of tissue types including epithelium, muscle, and nerve tissue, the bulk of which are cells.
- A major component is the extracellular matrix (ECM).
- The ECM consists of protein fibers (collagen and elastic)
- The ECM also contains ground substance.
Connective Tissue Proper Distribution and Function
- Found throughout the body.
- Connects epithelia to underlying body structures.
- Links muscles to bones.
- Holds joints together.
- Plays roles in defense, repair, storage, and nutrition.
- Provides a medium for oxygen and nutrient diffusion to cells from capillaries.
- Allows carbon dioxide and waste to diffuse back in to circulation.
- Allows organs to resist stretching and tearing forces.
Resident and Wandering Connective Tissue Cells
- Connective tissue cells are either resident or wandering.
- Cells of the resident cell population are stable and exhibit little movement.
- Resident cell types: fibroblasts, myofibroblasts, macrophages, adipocytes, mast cells, and adult stem cells.
- Wandering cells are primarily cells that have migrated into the tissue from the blood in response to stimuli.
- Wandering cell types: lymphocytes, plasma cells (differentiated B cells), neutrophils, eosinophils, basophils, and monocytes.
Fibroblasts: Main Cells of Connective Tissue Proper
- Represent the main cell population within connective tissue proper.
- These are large, flat, elongated (spindle-shaped) with processes extending from the cell body ends.
- The cell nucleus is flat and oval.
- They produce and maintain most of the tissue's extracellular components.
- Fibroblasts rarely divide in adults.
- Cell cycling and mitotic activity can resume when stimulated by growth factors, and when additional fibroblasts are needed.
Collagen and ECM Production by Fibroblasts
- Fibroblasts secrete collagen (most abundant protein), elastin, GAGs, proteoglycans, and multiadhesive glycoproteins.
- Most secreted ECM components undergo further modification outside the cell before matrix assembly.
Myofibroblasts and Wound Healing
- Fibroblasts are involved in wound healing, and known as myofibroblasts.
- Myofibroblasts have a well-developed contractile function.
- Myofibroblasts are enriched with a form of actin also found in smooth muscle cells.
Fibroblast Activity Levels
- Two activity levels can be observed histologically.
- Cells with synthetic activity are morphologically distinct from the quiescent ones.
- Quiescent fibroblasts may be scattered within the matrix that they've synthesized.
- Active cells are sometimes called "fibroblasts".
- Quiescent cells are sometimes called "fibrocytes".
Active vs Quiescent Fibroblasts
- Active fibroblasts have more abundant and irregularly branched cytoplasm.
- The active fibroblast nucleus is large, ovoid, euchromatic, and has a prominent nucleolus.
- Active fibroblasts have abundant rough endoplasmic reticulum (RER) and a well-developed Golgi.
- Quiescent fibroblasts are smaller than active ones and spindle-shaped
- Quiescent fibroblasts have fewer processes and less RER, and have darker, more heterochromatic nucleus.
Adipocytes: Fat Storage
- Adipocytes, or fat cells, are found in the connective tissue of many organs.
- Large, mesenchymally-derived cells are specialized for cytoplasmic storage of lipid as neutral fats.
- Fat deposits also cushion and insulate the skin and other organs.
- Adipocytes have major metabolic and medical significance.
Leukocytes and Diapedesis
- Besides macrophages and plasma cells, connective tissue contains leukocytes from cells circulating in the blood.
- Leukocytes, or white blood cells, create a population of wandering cells in the connective tissue.
- Leukocytes leave the blood by migrating between endothelial cells lining venules, in a process called diapedesis.
- Diapedesis increases greatly during inflammation, a vascular and cellular defensive response to injury or foreign substances.
Macrophages: Phagocytic Cells
- Macrophages derive from monocytes.
- Macrophages are characterized by phagocytic ability and turnover of protein fibers.
- Macrophages are responsible for removing dead cells, tissue debris, and other particulate material.
- Varying morphologic features exist according to their state of functional activity and the tissue they inhabit.
Macrophage Characteristics
- A typical macrophage has a 10-30 μm diameter and an oval or kidney-shaped nucleus.
- Macrophages are present in connective tissue of organs; pathologists often refer to macrophages as "histiocytes."
- In TEM, possess a characteristic irregular surface with pleats, protrusions, and indentations.
- These surfaces denote active pinocytotic and phagocytic activities.
- Macrophages have a well-developed Golgi apparatus and many lysosomes.
Macrophage Development
- Macrophages derive from bone marrow precursor cells that divide, producing monocytes that circulate in the blood.
- Monocytes cross the epithelial wall of venules and penetrate connective tissue.
- In connective tissue, monocytes differentiate, mature, and acquire morphologic features of phagocytic cells.
- Monocytes and macrophages are the same cell at different maturation stages.
Mononuclear Phagocyte System
- Macrophage-like cells have different names in different organs.
- Kupffer cells are present in the liver.
- Microglial cells are present in the central nervous system.
- Langerhans cells are present in the skin.
- Osteoclasts are present in bone tissue.
- All the macrophage-like cells are derived from monocytes.
- All macrophage-like cells are long-living and survive for months in tissues.
- They are important for debris removal, uptake, processing, and presentation of antigens for lymphocyte activation, a function of the immune system.
Mast Cells: Immune Regulators
- Mast cells are a type of white blood cell.
- Consist of oval, irregularly shaped connective tissue cells, which measure 7-20 μm.
- The cytoplasm is filled with basophilic secretory granules.
- Nuclei are centrally situated and obscured by secretory granules.
- Granules are heterogeneous in structure and measure 0.3-2.0 μm.
- Granules are poorly preserved by common fixatives, so that mast cells are difficult to identify.
- Mast cells regulate of the immune system.
Mast Cell Development and Function
- Mast cells originate from progenitor cells in bone marrow.
- Progenitor cells circulate in the blood, crossing the venule and capillary walls.
- Progenitor cells penetrate connective tissues and differentiate.
- They release chemical mediators stored in mast cells and promote allergic reactions / immediate hypersensitivity reactions.
- Immediate hypersensitivity reactions happen within minutes of antigen appearance in an individual previously sensitized to the same or similar antigen.
- Mast cells function in localized release of bioactive substances with roles in the local inflammatory response, innate immunity, and tissue repair.
Molecules Secreted by Mast Cells
- Heparin is a sulfated GAG that acts locally as an anticoagulant.
- Histamine promotes increased vascular permeability and smooth muscle contraction.
- Serine proteases activate various mediators of inflammation.
- Eosinophil and neutrophil chemotactic factors attract leukocytes.
- Cytokines are the polypeptides that direct leukocytes and other cells in the immune system.
- Phospholipid precursors convert to prostaglandins, leukotrienes, and other lipid mediators of the inflammatory response.
Plasma Cells: Antibody Production
- Plasma cells are B-lymphocyte-derived, antibody-producing cells.
- They have large, ovoid basophilic cytoplasm, a result of richness in RER.
- The Golgi apparatus and centrioles occupy a pale region near the nucleus in routine histologic preparations.
- Nucleus is spherical but eccentrically placed.
- Plasma cells are present in most connective tissues.
- Plasma cells have an average lifespan of 10-20 days
Fiber Composition
- Fibrous components of connective tissue consist of elongated structures.
- Fibrous components of connective tissue are formed from proteins that polymerize after secretion from fibroblasts.
- 3 main types of fibers: collagen, reticular, and elastic.
- Collagen and reticular fibers originate from proteins of the collagen family.
- Elastic fibers consist mainly of elastin protein.
- These fibers distribute unequally among the different types of connective tissue
Collagen
- Collagens constitute a protein family able to form a variety of extracellular structures.
- Collagen fibers, sheets and networks are strong and resistant to normal shearing and tearing forces.
- It is the most abundant protein in the human body (30% of its dry weight).
- Major components of fibroblasts as collagens secrete from several other cell types.
- Collagen turnover and renewal in connective tissue is a slow, ongoing process.
Categories of Collagen
- Can be grouped according to their structures which are formed by their subunits.
- Fibrillar collagens: collagen types I, II, and III have subunits that aggregate to form large fibrils are visible in the electron or light microscope.
- Collagen type I: the most abundant and widely distributed collagen.
- Forms large, eosinophilic bundles and is known as collagen fibers.
- Collagen type I densely fills connective tissue, forming structures including tendons, organ capsules, and dermis.
- Sheet-forming collagens, including type IV collagen.
- Sheet-forming collagens have subunits created by epithelial cells.
- They are the major structural proteins of external laminae and the basal lamina in epithelia.
- Linking/anchoring collagens are short collagens linking fibrillar collagens to components of the ECM.
- Type VII collagen binds type IV collagen.
- Type VII collagen anchors the basal lamina to the underlying reticular lamina in basement membranes.
Collagen Synthesis
- Occurs in fibroblasts and several other cell types.
- The initial procollagen α chains are created first.
- Three α chains selected, aligned, and stabilized by disulfide bonds in the ER.
- Folded as a triple helix.
- The triple helix undergoes exocytosis and is cleaved to procollagen molecule.
- The procollagen molecule is the basic subunit from which the fibers or sheets are assembled.
- Subunits may be homotrimeric (all 3 chains identical) or heterotrimeric (2-3 chains having different sequences).
- Different combinations of procollagen α chains produce the various collagen types with different structures and functions.
- Collagen biosynthesis is complex and has many steps, meaning there are many points at which the process can be interrupted / changed by defective enzymes / disease processes.
Reticular Fibers
- Found in the delicate connective tissue of organs.
- Consist mainly of collagen type III and form an extensive network (reticulum) of thin, heavily glycosylated fibers.
- Seldom visible in hematoxylin and eosin (H&E) preparations.
- Stained black by impregnation with silver salts.
- Periodic acid-Schiff (PAS) positive.
- Reticular fibers contain up to 10% carbohydrate, as opposed to 1% in most other collagen fibers.
- Reticular fibers (produced by fibroblasts) occur in the reticular lamina of basement membranes.
- Surrounded adipocytes, smooth muscle and nerve fibers, and small blood vessels.
- Delicate reticular networks support the stroma for parenchymal secretory cells and rich microvasculature of the liver and endocrine glands.
- Abundant reticular fibers characterize the stroma of hemopoietic tissue (bone marrow) and some lymphoid organs (spleen / lymph nodes).
Elastic Fibers
- Elastic fibers are thin compared to type I collagen fibers.
- Form sparse networks in highly bent or stretched organs.
- Have physical properties similar to rubber.
- Allow tissues to stretch / distend and return to original shape.
- In the walls of large blood vessels, especially arteries, elastin occurs as fenestrated sheets called elastic lamellae.
- Elastic fibers and lamellae stain poorly with H&E and are more darkly stained by orcein and aldehyde fuchsin.
- Elastic fibers and lamellae are a composite of fibrillin microfibrils embedded in a larger mass of cross-linked elastin.
- Both components secrete from fibroblasts (and smooth muscle cells in vascular walls) and produce elastic fibers in a stepwise manner.
- Initially, microfibrils consist of fibrillin which forms protein fibrillin.
- Microfibrils scaffold elastin, on which elastin is deposited.
- Elastin accumulates between microfibrils, embedding most of these with the mass eventually comprising most of the elastic fiber.
- The properties of elastic fibers and lamellae result from the structure of elastin subunits, and unique cross-links holding them together.
- Elastin molecules are rich in glycine, proline and lysine, giving protein a random-coil conformation.
- Elastin resists digestion by most proteases and is hydrolyzed by pancreatic elastase.
Ground Substance
- The ECM ground substance is a highly hydrated, transparent mixture of macromolecules.
- Macromolecules are made of glycosaminoglycans (GAGs), proteoglycans & multiadhesive glycoproteins (laminin and fibronectin).
- Ground substance fills spaces between cells and fibers in connective tissue.
- Acts as both a lubricant and barrier to the penetration of invaders.
- The hydrated nature of connective tissue provides a medium for nutrient exchange and metabolic waste between cells / the blood supply.
- Glycoproteins stabilize the ECM by binding to matrix components / integrins in cell membranes.
Glycosaminoglycans (GAGs)
- GAGs (mucopolysaccharides) are long polysaccharides consisting of repeating disaccharide units.
- Hyaluronic acid (hyaluronan or HA) is the largest and most important GAG.
- GAGs bind large amounts of water, allowing polyanions to swell and occupy large tissue spaces.
- 4 major GAGs found in proteoglycans dermatan sulfate, chondroitin sulfates, keratan sulfate, heparan sulfate
- All have different disaccharide units and tissue distributions
Proteoglycans
- Proteoglycans consist of a protein core covalently attached to sulfated GAGs in varied numbers/combinations.
- Like glycoproteins, synthesized on RER.
- Mature in the Golgi, where GAG side chains are added and secreted from cells by exocytosis.
- Contain a greater mass of polysaccharide chains than polypeptide.
- The major cartilage constituent aggrecan is a proteoglycan.
- ECM regions contain various proteoglycan core proteins, each one carrying GAGs of different lengths/compositions.
Proteoglycan Types
- Decorin is a small proteoglycan with few GAG side chains that binds fibrils of type I collagen.
- Cell surface proteoglycans (syndecan) have transmembrane core proteins and serve as additional cell attachments to ECM.
- Aggrecan is a large proteoglycan with a core protein carrying chondroitin sulfate and keratan sulfate chains.
Multiadhesive Glycoproteins and Substrates
- Multiadhesive glycoproteins provide multiple binding sites for cell surface receptors (integrins) and matrix macromolecules.
- The adhesive glycoproteins are large branched molecules and important in adhesion of cells to their substrate.
- Laminin provides adhesion for epithelial and other cells, with integrin, type IV collagen, and proteoglycan binding sites.
- Basal and external laminae are rich in laminin.
- Laminin is essential for structure assembly / maintenance.
- Fibronectin (synthesized by fibroblasts), has binding sites for collagens and forms insoluble fibrillar networks.
- Provides specific binding sites for integrins and is important for cell adhesion and migration.
- In addition to the hydrated ground substance, connective tissue has some free interstitial fluid, with ion composition like that of blood plasma.
- It’s plasma protein content is low in molecular weight that pass through the thin walls of capillaries.
Basement Membrane Constituents
- The basement membrane has 2 sublayers the basal lamina and the reticular lamina.
- The basal lamina (100 nm thick) consists of fine protein filaments embedded in an amorphous matrix produced by the epithelial cells.
- The reticular lamina consists of reticular fibers from cells of the underlying connective tissue.
- Basement membrane functions by supporting the epithelium and acting as a selectively permeable filter.
- ECM components of basal laminae is laminin self-assemble in a lacelike network below the basal poles of cells (anchored by trans-membrane integrins).
- The laminin and type IV collagen networks held by the adhesive glycoprotein entactin/nidogen, and the proteoglycan perlecan.
- Type IV collagen is a sheet-forming collagen that consists of monomers containing 3 polypeptide chains, self-assembling to form feltlike layers.
- Type VII collagen, linking/anchoring collagen, binds to type IV collagen and anchors the basal lamina to the underlying reticular lamina in basement.
Connective Tissue
- Meshwork contains type III collagen
- collagen anchored to 2 basal laminae by anchoring fibrils composed of type VII collagen.
- Meshwork produced by cells of the connective tissue.
Connective Tissue Origin
- Originates from embryonic mesenchyme, a tissue developing from the middle layer of the embryo, or mesoderm.
- Mesenchyme has a viscous ground substance with few collagen fibers.
- Mesenchymal cells are undifferentiated and have large nuclei, nucleoli and fine chromatin.
- Mesenchymal cells are “spindle-shaped,” with cytoplasmic extensions.
- The cells produce all types of connective tissue proper, specialized connective tissue, bone, and cartilage.
- The embryonic mesenchyme consists of stem cells for other tissues such as blood.
Types of Connective Tissue
- Different combinations and densities of cells, fibers, and extracellular macromolecules produce variations in histological structure.
- Types used denote a major component or a structural tissue characteristic.
Connective Tissue Proper Classification
- Connective tissue proper has 2 classes: loose and dense.
- Loose and dense refers to the amount of collagen present in the tissue.
- Loose connective tissue (areolar tissue) is common and supports epithelial tissue.
- Loose connective tissue comprises lamina propria ( thick layer) under epithelial lining and fills spaces between muscle and nerve fibers.
- Usually well-vascularized thin layers of loose connective tissue surround small blood vessels.
Loose Connective Tissue Fibers, Cells, and Function
- Loose connective tissue mostly contains equal parts cells, fibers, and ground substance.
- Most numerous cells are fibroblasts, along with types of connective tissue cells in the body and blood vessels.
- Collagen fibers predominate, but also elastic and reticular fibers.
- Loose connective tissue has a flexible consistency and is not stress resistant.
Dense Connective Tissue Function and Composition
- Dense connective tissue is adapted for resistance and protection.
- Shares components with loose connective tissue, but has fewer cells.
- Dense connective predominates collagen fibers instead of ground substance and is much more resistant to stress than loose connective tissue.
- Has 2 subtypes: regular and irregular
Irregular Density Connective Tissue
- In dense irregular connective tissue bundles of collagen appear randomly interwoven, with no definite orientation.
- The collagen fibers form a 3D network, providing resistance to stress from all directions.
- Dense irregular connective tissue is closely associated with loose connective tissue
Regular Density Connective Tissue
- Type 1 collagen bundles are arranged according to pattern.
- Fibers and fibroblasts are aligned in parallel to resist stress from the same direction.
- Tendons and ligaments are types of connective tissue ( strong straps and chords that connects components of the system).
- Dense has packed collagen, and appears white in the fresh state and almost inextensible.
- Parallel, closely packed bundles of collagen are separated by very little ground substance.
Reticular Tissue Characteristics
- Type III collagen fibers create a delicate 3D network that supports various types of cells.
- Fibrous network produced by modified fibroblasts called reticular cells.
- The network remains associated with and partially covering the fibers.
- Loose reticular fibers provide specialized framework for microenvironments of hematopoietic tissue and lymphoid organs.
- Resulting system creates a meshwork for lymphocyte and lymph passage.
- Macrophages and other cells of the mononuclear phagocyte system are dispersed into these reticular tissues.
Mucoid Tissue
- Mucoid tissue is an embryonic connective tissue.
- Mucoid tissue is found mainly in the umbilical cord and fetal organs.
- A chief component is its abundant ground substance composed mostly of hyaluronic acid.
- mucoid tissue is jellylike with sparse collagen fibers, and embedded scattered fibroblasts
- referred to as Wharton’s jelly.
- Also in the pulp cavities of young teeth, provides a postnatal stem cell source.
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.