Podcast
Questions and Answers
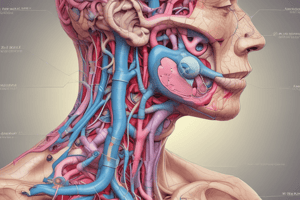
What are the main components of the pancreas?
What are the main components of the pancreas?
Exocrine and endocrine functions
The exocrine pancreas is composed of two types of cells. What are these cells?
The exocrine pancreas is composed of two types of cells. What are these cells?
Pancreatic acinar cells and duct cells
What is the function of the duct cells?
What is the function of the duct cells?
They serve as a “roadway” to duodenum
What is the function of the exocrine pancreas?
What is the function of the exocrine pancreas?
The endocrine pancreas is composed of __________
The endocrine pancreas is composed of __________
What are the cell types found in the islets of langerhans in the endocrine pancreas?
What are the cell types found in the islets of langerhans in the endocrine pancreas?
Each cell produces a distinct hormone.
Each cell produces a distinct hormone.
What hormones from the pancreas are involved in glucose metabolism?
What hormones from the pancreas are involved in glucose metabolism?
Beta cells secrete insulin in response to hypoglycemia
Beta cells secrete insulin in response to hypoglycemia
Describe the process of insulin synthesis and secretion
Describe the process of insulin synthesis and secretion
How many chains make up insulin and which ones are they?
How many chains make up insulin and which ones are they?
Amino acid sequences forming the insulin protein are different between species. For example, dogs can’t use insulin from pigs
Amino acid sequences forming the insulin protein are different between species. For example, dogs can’t use insulin from pigs
Species specific differences in insulin structure
Species specific differences in insulin structure
In carnivores, which substance primarily stimulates insulin secretion?
In carnivores, which substance primarily stimulates insulin secretion?
Which of the following is a stimulant for insulin release specifically in humans?
Which of the following is a stimulant for insulin release specifically in humans?
What is the primary factor influencing insulin secretion in omnivores?
What is the primary factor influencing insulin secretion in omnivores?
Which statement is true regarding insulin secretion in ruminants?
Which statement is true regarding insulin secretion in ruminants?
Which of the following variables does NOT influence insulin release?
Which of the following variables does NOT influence insulin release?
What hormones stimulate insulin secretion?
What hormones stimulate insulin secretion?
Nutrition is a stimulator factor for insulin secretion. What are these nutrients?
Nutrition is a stimulator factor for insulin secretion. What are these nutrients?
Which of the following hormones is NOT an inhibitor of insulin secretion?
Which of the following hormones is NOT an inhibitor of insulin secretion?
List all the hormones that inhibit insulin secretion (ones important in class)
List all the hormones that inhibit insulin secretion (ones important in class)
Name and describe the phases of insulin secretion
Name and describe the phases of insulin secretion
GLUT2 transporters aer found on both beta and alpha cells
GLUT2 transporters aer found on both beta and alpha cells
Highlight the process in which glucose enters the beta cell to release insulin
Highlight the process in which glucose enters the beta cell to release insulin
What would happen with the addition of sulfonylureas affect insulin release?
What would happen with the addition of sulfonylureas affect insulin release?
What is the membrane receptor that insulin binds to on target tissues and how many molecules need to bind in order to activate it?
What is the membrane receptor that insulin binds to on target tissues and how many molecules need to bind in order to activate it?
Describe the physiological effects of insulin
Describe the physiological effects of insulin
What are the most important insulin sensitive tissues?
What are the most important insulin sensitive tissues?
What is the primary mechanism by which insulin facilitates glucose entry into the cells?
What is the primary mechanism by which insulin facilitates glucose entry into the cells?
Which of the following statements about GLUT-4 is true?
Which of the following statements about GLUT-4 is true?
What type of stimulation is referred to as non-insulin mediated action in relation to GLUT-4?
What type of stimulation is referred to as non-insulin mediated action in relation to GLUT-4?
Which glucose transporter is specifically characterized as insulin-sensitive?
Which glucose transporter is specifically characterized as insulin-sensitive?
Which of the following is NOT a role of GLUT-4 in glucose metabolism?
Which of the following is NOT a role of GLUT-4 in glucose metabolism?
Insulin is inactivated mainly by what two organs?
Insulin is inactivated mainly by what two organs?
In adipose tissue, insulin inhibits lipolysis and promotes adipose deposition
In adipose tissue, insulin inhibits lipolysis and promotes adipose deposition
What hormones counteract the effects of insulin?
What hormones counteract the effects of insulin?
Which of the following counter regulatory hormones are acute phase?
Which of the following counter regulatory hormones are acute phase?
What is one effect of cortisol during the chronic phase of hypoglycemia?
What is one effect of cortisol during the chronic phase of hypoglycemia?
In addition to glucagon, which other hormone aids in gluconeogenesis during acute hypoglycemia?
In addition to glucagon, which other hormone aids in gluconeogenesis during acute hypoglycemia?
Which counter regulatory hormone is primarily responsible for increasing muscular lipolysis during hypoglycemia?
Which counter regulatory hormone is primarily responsible for increasing muscular lipolysis during hypoglycemia?
Glucagon is a polypeptide hormone produced in alpha cells of pancreatic islets
Glucagon is a polypeptide hormone produced in alpha cells of pancreatic islets
What stimulates the synthesis of glucagon?
What stimulates the synthesis of glucagon?
Describe glucagon synthesis
Describe glucagon synthesis
What is the purpose of glucagon within the body?
What is the purpose of glucagon within the body?
Glucagon synthesis is promoted by voltage-dependent K+ channels
Glucagon synthesis is promoted by voltage-dependent K+ channels
What is the primary effect of glucagon on the liver?
What is the primary effect of glucagon on the liver?
Which amino acids are specifically known to stimulate both insulin and glucagon release?
Which amino acids are specifically known to stimulate both insulin and glucagon release?
What is one of the key actions of glucagon on adipocytes?
What is one of the key actions of glucagon on adipocytes?
In obligate carnivores, what effect does glucagon have in response to increased amino acid levels?
In obligate carnivores, what effect does glucagon have in response to increased amino acid levels?
What is the primary role of pancreatic somatostatin in the gastrointestinal tract?
What is the primary role of pancreatic somatostatin in the gastrointestinal tract?
Which cells in the pancreas are responsible for producing pancreatic polypeptide?
Which cells in the pancreas are responsible for producing pancreatic polypeptide?
What effect does somatostatin have on pancreatic polypeptide secretion?
What effect does somatostatin have on pancreatic polypeptide secretion?
Which of the following is a known effect of pancreatic polypeptide on the gastrointestinal tract?
Which of the following is a known effect of pancreatic polypeptide on the gastrointestinal tract?
Which of these statements about the actions of somatostatin is correct?
Which of these statements about the actions of somatostatin is correct?
What is the primary difference between absolute and relative insulin deficiency in diabetes mellitus?
What is the primary difference between absolute and relative insulin deficiency in diabetes mellitus?
List two primary clinical signs associated with hyperglycemia in diabetes mellitus.
List two primary clinical signs associated with hyperglycemia in diabetes mellitus.
Explain how insulin deficiency affects glucagon production.
Explain how insulin deficiency affects glucagon production.
What role does hormone-sensitive lipase play in diabetes mellitus?
What role does hormone-sensitive lipase play in diabetes mellitus?
Describe the metabolic effect of insulin deficiency on muscle tissue.
Describe the metabolic effect of insulin deficiency on muscle tissue.
How does glucagon promote gluconeogenesis, particularly in times of insulin deficiency?
How does glucagon promote gluconeogenesis, particularly in times of insulin deficiency?
Identify one potential effect of excess free fatty acids (FFA) in diabetic patients.
Identify one potential effect of excess free fatty acids (FFA) in diabetic patients.
What is the significance of paradoxical hyperglucagonemia in diabetes mellitus?
What is the significance of paradoxical hyperglucagonemia in diabetes mellitus?
What is the primary underlying cause of Type I diabetes in dogs?
What is the primary underlying cause of Type I diabetes in dogs?
What factor contributes most significantly to the development of cataracts in diabetic patients?
What factor contributes most significantly to the development of cataracts in diabetic patients?
Which of the following statements accurately describes the nature of Type II diabetes in cats?
Which of the following statements accurately describes the nature of Type II diabetes in cats?
Which condition is most likely to impair insulin secretion and cause beta cell dysfunction in cats with obesity?
Which condition is most likely to impair insulin secretion and cause beta cell dysfunction in cats with obesity?
What role does amylin play in the context of diabetes in cats?
What role does amylin play in the context of diabetes in cats?
Which of the following statements about the relationship between obesity and diabetes in cats is true?
Which of the following statements about the relationship between obesity and diabetes in cats is true?
What is the significance of aldose reductase in diabetic cataract formation?
What is the significance of aldose reductase in diabetic cataract formation?
Which of the following factors is least associated with the etiopathogenesis of Type II diabetes in cats?
Which of the following factors is least associated with the etiopathogenesis of Type II diabetes in cats?
What is one of the common causes of insulin resistance in cats?
What is one of the common causes of insulin resistance in cats?
Describe the condition under which clinical remission can occur in type 2 diabetes mellitus in cats.
Describe the condition under which clinical remission can occur in type 2 diabetes mellitus in cats.
What is a common chronic complication of diabetes in cats and its primary cause?
What is a common chronic complication of diabetes in cats and its primary cause?
What role does glucotoxicity play in the context of beta cell dysfunction in cats with diabetes?
What role does glucotoxicity play in the context of beta cell dysfunction in cats with diabetes?
What are the clinical signs of diabetic neuropathy in cats, and how can they vary?
What are the clinical signs of diabetic neuropathy in cats, and how can they vary?
DKA is not a severe complication of Diabetes mellitus
DKA is not a severe complication of Diabetes mellitus
Which counterregulatory hormone is the most influential ketogenenic hormone?
Which counterregulatory hormone is the most influential ketogenenic hormone?
What electrolytes are affected by DKA?
What electrolytes are affected by DKA?
What physiological change occurs as a result of acidosis due to excessive ketone accumulation?
What physiological change occurs as a result of acidosis due to excessive ketone accumulation?
Which factors contribute to the kidney's failure to compensate during Diabetic Ketoacidosis (DKA)?
Which factors contribute to the kidney's failure to compensate during Diabetic Ketoacidosis (DKA)?
What is the most likely consequence of overwhelming the body's buffering system during acidosis?
What is the most likely consequence of overwhelming the body's buffering system during acidosis?
Which molecule's accumulation is primarily responsible for the acidosis associated with diabetes?
Which molecule's accumulation is primarily responsible for the acidosis associated with diabetes?
What primary effect does untreated acidosis have on the body's acid-base balance?
What primary effect does untreated acidosis have on the body's acid-base balance?
What type of pancreatic tumor is characterized by the excessive production of insulin regardless of blood glucose levels?
What type of pancreatic tumor is characterized by the excessive production of insulin regardless of blood glucose levels?
Which clinical sign is most commonly associated with glucagonoma?
Which clinical sign is most commonly associated with glucagonoma?
In which species is insulinoma rarely observed?
In which species is insulinoma rarely observed?
Which cell type is responsible for synthesizing and secreting glucagon?
Which cell type is responsible for synthesizing and secreting glucagon?
What is a significant characteristic of the insulinoma tumors in terms of their insulin production?
What is a significant characteristic of the insulinoma tumors in terms of their insulin production?
Flashcards
Insulin Release Factors
Insulin Release Factors
Insulin release is regulated by several factors including nutrition, nerves, hormones, and local signaling molecules.
Omnivore Insulin Secretion
Omnivore Insulin Secretion
In omnivores, glucose is the primary stimulus for insulin secretion.
Carnivore Insulin Secretion
Carnivore Insulin Secretion
In carnivores, amino acids are the primary stimulus for insulin secretion.
Human Insulin Stimulation
Human Insulin Stimulation
Signup and view all the flashcards
Ruminant Insulin Stimulation
Ruminant Insulin Stimulation
Signup and view all the flashcards
GLUT-4
GLUT-4
Signup and view all the flashcards
Insulin's role in glucose transport
Insulin's role in glucose transport
Signup and view all the flashcards
Exercise and GLUT-4
Exercise and GLUT-4
Signup and view all the flashcards
Non-insulin mediated GLUT-4 stimulation
Non-insulin mediated GLUT-4 stimulation
Signup and view all the flashcards
Why is GLUT-4 important?
Why is GLUT-4 important?
Signup and view all the flashcards
Counter-Regulatory Hormones
Counter-Regulatory Hormones
Signup and view all the flashcards
Acute Hypoglycemia Response
Acute Hypoglycemia Response
Signup and view all the flashcards
Chronic Hypoglycemia Response
Chronic Hypoglycemia Response
Signup and view all the flashcards
How do these hormones affect the liver?
How do these hormones affect the liver?
Signup and view all the flashcards
How do these hormones affect adipose tissue?
How do these hormones affect adipose tissue?
Signup and view all the flashcards
Glucagon's Primary Target
Glucagon's Primary Target
Signup and view all the flashcards
Glucagon's Role in Energy
Glucagon's Role in Energy
Signup and view all the flashcards
Glucagon and Amino Acids
Glucagon and Amino Acids
Signup and view all the flashcards
Hormone-Sensitive Lipase (HSL)
Hormone-Sensitive Lipase (HSL)
Signup and view all the flashcards
Glucagon's Importance
Glucagon's Importance
Signup and view all the flashcards
Somatostatin's Role
Somatostatin's Role
Signup and view all the flashcards
Somatostatin's Target
Somatostatin's Target
Signup and view all the flashcards
Pancreatic Polypeptide Production
Pancreatic Polypeptide Production
Signup and view all the flashcards
Pancreatic Polypeptide's Function
Pancreatic Polypeptide's Function
Signup and view all the flashcards
Somatostatin's Influence on Pancreatic Polypeptide
Somatostatin's Influence on Pancreatic Polypeptide
Signup and view all the flashcards
Diabetes Mellitus
Diabetes Mellitus
Signup and view all the flashcards
Type 1 Diabetes
Type 1 Diabetes
Signup and view all the flashcards
Type 2 Diabetes
Type 2 Diabetes
Signup and view all the flashcards
Hyperglycemia
Hyperglycemia
Signup and view all the flashcards
Polyuria, Polydipsia, Polyphagia
Polyuria, Polydipsia, Polyphagia
Signup and view all the flashcards
Paradoxical Hyperglucagonemia
Paradoxical Hyperglucagonemia
Signup and view all the flashcards
FFA Release in Diabetes
FFA Release in Diabetes
Signup and view all the flashcards
Muscle Catabolism in Diabetes
Muscle Catabolism in Diabetes
Signup and view all the flashcards
What causes cataracts in Type I diabetes?
What causes cataracts in Type I diabetes?
Signup and view all the flashcards
Islet Amyloidosis
Islet Amyloidosis
Signup and view all the flashcards
What is amylin?
What is amylin?
Signup and view all the flashcards
Why do obese cats not always develop diabetes?
Why do obese cats not always develop diabetes?
Signup and view all the flashcards
How does amylin form amyloid?
How does amylin form amyloid?
Signup and view all the flashcards
Why is amyloid toxic to beta cells?
Why is amyloid toxic to beta cells?
Signup and view all the flashcards
Hypoinsulinemia
Hypoinsulinemia
Signup and view all the flashcards
Common insulin resistance causes in cats
Common insulin resistance causes in cats
Signup and view all the flashcards
Clinical remission in feline diabetes
Clinical remission in feline diabetes
Signup and view all the flashcards
What's irreversible in feline diabetes?
What's irreversible in feline diabetes?
Signup and view all the flashcards
Diabetic neuropathy in cats
Diabetic neuropathy in cats
Signup and view all the flashcards
How does hyperglycemia damage nerves?
How does hyperglycemia damage nerves?
Signup and view all the flashcards
Ketones and Acidosis
Ketones and Acidosis
Signup and view all the flashcards
Beta Hydroxybutyrate and Acetoacetate
Beta Hydroxybutyrate and Acetoacetate
Signup and view all the flashcards
DKA and Kidney Failure
DKA and Kidney Failure
Signup and view all the flashcards
What Causes Acidosis in DKA?
What Causes Acidosis in DKA?
Signup and view all the flashcards
How Does DKA Affect Kidney Function?
How Does DKA Affect Kidney Function?
Signup and view all the flashcards
Acidosis in DKA
Acidosis in DKA
Signup and view all the flashcards
Kidney Failure in DKA
Kidney Failure in DKA
Signup and view all the flashcards
Insulinoma
Insulinoma
Signup and view all the flashcards
Glucagonoma
Glucagonoma
Signup and view all the flashcards
Beta Cells in Insulinoma
Beta Cells in Insulinoma
Signup and view all the flashcards
Alpha Cells in Glucagonoma
Alpha Cells in Glucagonoma
Signup and view all the flashcards
Insulinoma: Who Gets It?
Insulinoma: Who Gets It?
Signup and view all the flashcards