Podcast
Questions and Answers
What is a potential risk associated with bottle feeding in cribs?
What is a potential risk associated with bottle feeding in cribs?
- Overheating the infant
- Increased risk of SIDS
- Increased incidence of sleep apnea
- Aspiration due to position (correct)
What is a major consequence of prolonged oxygen therapy and ventilation in premature infants?
What is a major consequence of prolonged oxygen therapy and ventilation in premature infants?
- Increased lung capacity
- Improved gas exchange
- Chronic Obstructive Pulmonary Disease (correct)
- Enhanced pulmonary compliance
What is a common medication used to manage apnea in infants?
What is a common medication used to manage apnea in infants?
- Morphine
- Ibuprofen
- Amoxicillin
- Caffeine (correct)
Which condition can indicate the presence of SIDS during an autopsy?
Which condition can indicate the presence of SIDS during an autopsy?
Which diagnostic finding suggests hypercapnia in a patient with Bronchopulmonary Dysplasia?
Which diagnostic finding suggests hypercapnia in a patient with Bronchopulmonary Dysplasia?
What describes an Apparent Life-Threatening Event (ALTE)?
What describes an Apparent Life-Threatening Event (ALTE)?
Which of the following is NOT a risk factor for Sudden Infant Death Syndrome (SIDS)?
Which of the following is NOT a risk factor for Sudden Infant Death Syndrome (SIDS)?
What position should infants be placed in during sleep to reduce the risk of SIDS?
What position should infants be placed in during sleep to reduce the risk of SIDS?
What is NOT a recommended safety practice for infant sleep?
What is NOT a recommended safety practice for infant sleep?
What characterizes the lungs of a patient suffering from Bronchopulmonary Dysplasia as seen in a chest X-ray?
What characterizes the lungs of a patient suffering from Bronchopulmonary Dysplasia as seen in a chest X-ray?
What characterizes asthma as a chronic respiratory disorder?
What characterizes asthma as a chronic respiratory disorder?
What color indicates a need for an inhaler or aerosol?
What color indicates a need for an inhaler or aerosol?
What is the highest mortality rate demographic for asthma?
What is the highest mortality rate demographic for asthma?
Which of the following is NOT a trigger for respiratory issues in children?
Which of the following is NOT a trigger for respiratory issues in children?
Which diagnostic test measures the amount of air during inspiration and expiration?
Which diagnostic test measures the amount of air during inspiration and expiration?
Which of the following is a sign of respiratory distress in asthma patients?
Which of the following is a sign of respiratory distress in asthma patients?
Cystic Fibrosis primarily affects which type of glands in the body?
Cystic Fibrosis primarily affects which type of glands in the body?
What medication class is Albuterol categorized under for asthma treatment?
What medication class is Albuterol categorized under for asthma treatment?
What is the most common inheritance pattern of Cystic Fibrosis?
What is the most common inheritance pattern of Cystic Fibrosis?
What condition can result from the malabsorption of nutrients in Cystic Fibrosis?
What condition can result from the malabsorption of nutrients in Cystic Fibrosis?
What is the purpose of inhaled corticosteroids in managing asthma?
What is the purpose of inhaled corticosteroids in managing asthma?
Which symptom indicates that a child may have difficulty passing the first stool at birth?
Which symptom indicates that a child may have difficulty passing the first stool at birth?
What is the function of pulse oximetry in asthma care?
What is the function of pulse oximetry in asthma care?
Which position is recommended for a patient in respiratory distress due to asthma?
Which position is recommended for a patient in respiratory distress due to asthma?
What is a common gastrointestinal manifestation of Cystic Fibrosis?
What is a common gastrointestinal manifestation of Cystic Fibrosis?
Which chromosome is responsible for the gene mutation associated with Cystic Fibrosis?
Which chromosome is responsible for the gene mutation associated with Cystic Fibrosis?
What is a primary cause of Respiratory Distress Syndrome in preterm neonates?
What is a primary cause of Respiratory Distress Syndrome in preterm neonates?
Which of the following is NOT a clinical manifestation of Respiratory Distress Syndrome?
Which of the following is NOT a clinical manifestation of Respiratory Distress Syndrome?
What treatment is primarily used to replace surfactant in infants with Respiratory Distress Syndrome?
What treatment is primarily used to replace surfactant in infants with Respiratory Distress Syndrome?
Which complication is associated with prolonged mechanical ventilation in children with RDS?
Which complication is associated with prolonged mechanical ventilation in children with RDS?
What clinical sign indicates that a child may be using accessory muscles for breathing?
What clinical sign indicates that a child may be using accessory muscles for breathing?
What is the recommended environment for neonates suffering from Respiratory Distress Syndrome to maintain normal temperature?
What is the recommended environment for neonates suffering from Respiratory Distress Syndrome to maintain normal temperature?
Which of the following is a sign of hypoxia in a neonate?
Which of the following is a sign of hypoxia in a neonate?
What is a common respiratory rate indicating tachypnea in infants?
What is a common respiratory rate indicating tachypnea in infants?
What is the primary goal of treatment in cystic fibrosis?
What is the primary goal of treatment in cystic fibrosis?
Which test is diagnostic of cystic fibrosis when sweat chloride levels exceed 60 Meq/L?
Which test is diagnostic of cystic fibrosis when sweat chloride levels exceed 60 Meq/L?
What medication is used in aerosol treatments to facilitate expectoration of mucus?
What medication is used in aerosol treatments to facilitate expectoration of mucus?
How often should postural drainage be performed as part of pulmonary hygiene?
How often should postural drainage be performed as part of pulmonary hygiene?
What type of diet is recommended for individuals with cystic fibrosis?
What type of diet is recommended for individuals with cystic fibrosis?
Which of the following is NOT a medication class used in the treatment of cystic fibrosis?
Which of the following is NOT a medication class used in the treatment of cystic fibrosis?
What role do salt supplements play for children with cystic fibrosis?
What role do salt supplements play for children with cystic fibrosis?
Which therapy technique involves the use of aerosols before postural drainage?
Which therapy technique involves the use of aerosols before postural drainage?
What is the purpose of using pancreatic enzymes in cystic fibrosis treatment?
What is the purpose of using pancreatic enzymes in cystic fibrosis treatment?
What is one method to promote lung expansion in cystic fibrosis patients?
What is one method to promote lung expansion in cystic fibrosis patients?
A patient is prescribed theophylline for asthma management. Which of the following early signs of toxicity should the nurse monitor for?
A patient is prescribed theophylline for asthma management. Which of the following early signs of toxicity should the nurse monitor for?
A child with asthma uses a peak flow meter as part of their asthma management plan. A reading within which of the following ranges would indicate the need for an asthma medication intervention?
A child with asthma uses a peak flow meter as part of their asthma management plan. A reading within which of the following ranges would indicate the need for an asthma medication intervention?
A patient is prescribed a combination inhaler containing an inhaled corticosteroid (ICS) and a long-acting beta-agonist (LABA). Which of the following best describes when this combination treatment would most likely be used in the management of asthma patients?
A patient is prescribed a combination inhaler containing an inhaled corticosteroid (ICS) and a long-acting beta-agonist (LABA). Which of the following best describes when this combination treatment would most likely be used in the management of asthma patients?
A patient is using a metered-dose inhaler (MDI) with a spacer for asthma medication. Which of the following is the MOST appropriate instruction regarding the timing between puffs of medication?
A patient is using a metered-dose inhaler (MDI) with a spacer for asthma medication. Which of the following is the MOST appropriate instruction regarding the timing between puffs of medication?
A child with a history of asthma is being taught breathing exercises to help manage their condition. Which of the following exercises is most likely used to increase expiratory time and pressure?
A child with a history of asthma is being taught breathing exercises to help manage their condition. Which of the following exercises is most likely used to increase expiratory time and pressure?
Which of the following is the most likely finding that would be observed during an autopsy of an infant who has died of SIDS, that would also be relevant in other respiratory causes?
Which of the following is the most likely finding that would be observed during an autopsy of an infant who has died of SIDS, that would also be relevant in other respiratory causes?
A 1-month-old infant is brought to the ER after their parents found them unresponsive and with a bluish skin tone. The infant was limp, and appeared as if they were choking moments before becoming unresponsive. Which of these is MOST likely what is happening?
A 1-month-old infant is brought to the ER after their parents found them unresponsive and with a bluish skin tone. The infant was limp, and appeared as if they were choking moments before becoming unresponsive. Which of these is MOST likely what is happening?
A 2-month-old infant is being monitored for apnea using a 4-channel pneumogram. Which data point will be the PRIMARY focus of this test?
A 2-month-old infant is being monitored for apnea using a 4-channel pneumogram. Which data point will be the PRIMARY focus of this test?
Which practice is MOST effective at reducing the risk of Sudden Infant Death Syndrome (SIDS)?
Which practice is MOST effective at reducing the risk of Sudden Infant Death Syndrome (SIDS)?
During a home visit, the nurse is educating the parents of a 2-month-old infant about managing apnea that has been previously diagnosed. Besides medication, what should they be taught?
During a home visit, the nurse is educating the parents of a 2-month-old infant about managing apnea that has been previously diagnosed. Besides medication, what should they be taught?
What is the recommended action when a child's asthma action plan is in the "yellow" zone?
What is the recommended action when a child's asthma action plan is in the "yellow" zone?
Why is it recommended to wait one minute between puffs when administering a metered-dose inhaler with a spacer?
Why is it recommended to wait one minute between puffs when administering a metered-dose inhaler with a spacer?
Which of the following is the primary reason why cold liquids should be avoided by individuals experiencing respiratory distress or bronchospasm?
Which of the following is the primary reason why cold liquids should be avoided by individuals experiencing respiratory distress or bronchospasm?
Which of the following does not represent a common clinical manifestation of Cystic Fibrosis?
Which of the following does not represent a common clinical manifestation of Cystic Fibrosis?
A patient with cystic fibrosis displays clubbing of the nails. Which underlying cause is primarily responsible for this?
A patient with cystic fibrosis displays clubbing of the nails. Which underlying cause is primarily responsible for this?
What is the primary underlying cause of steatorrhea in patients with Cystic Fibrosis?
What is the primary underlying cause of steatorrhea in patients with Cystic Fibrosis?
Which genetic factor is responsible for the development of Cystic Fibrosis?
Which genetic factor is responsible for the development of Cystic Fibrosis?
Which of the following best describes the effect of mucus in males with cystic fibrosis on reproductive function?
Which of the following best describes the effect of mucus in males with cystic fibrosis on reproductive function?
What is a primary physiological effect of Bronchopulmonary Dysplasia (BPD) on the respiratory system?
What is a primary physiological effect of Bronchopulmonary Dysplasia (BPD) on the respiratory system?
Which of the following is characteristic of the typical presentation of Sudden Infant Death Syndrome (SIDS)?
Which of the following is characteristic of the typical presentation of Sudden Infant Death Syndrome (SIDS)?
What is the primary concern regarding oxygen therapy in the context of Bronchopulmonary Dysplasia (BPD)?
What is the primary concern regarding oxygen therapy in the context of Bronchopulmonary Dysplasia (BPD)?
Which of these findings would be most commonly expected in the blood gas analysis of a patient with BPD?
Which of these findings would be most commonly expected in the blood gas analysis of a patient with BPD?
To reduce the risk of Sudden Infant Death Syndrome (SIDS), which of the following practices is most crucial?
To reduce the risk of Sudden Infant Death Syndrome (SIDS), which of the following practices is most crucial?
Which of the following best explains why a patient with asthma might have decreased forced expiratory volume?
Which of the following best explains why a patient with asthma might have decreased forced expiratory volume?
A child with asthma presents with a persistent, non-productive cough, especially at night. This symptom is described as:
A child with asthma presents with a persistent, non-productive cough, especially at night. This symptom is described as:
During an asthma exacerbation, which of the following would be the earliest auscultatory finding?
During an asthma exacerbation, which of the following would be the earliest auscultatory finding?
If a child with asthma is showing signs of severe respiratory distress, what is the most important initial intervention?
If a child with asthma is showing signs of severe respiratory distress, what is the most important initial intervention?
An asthma patient's pulse oximetry reading is 92%. How would you interpret this reading?
An asthma patient's pulse oximetry reading is 92%. How would you interpret this reading?
Which of the following options correctly orders the actions of a SABA, such as albuterol, during an asthma attack?
Which of the following options correctly orders the actions of a SABA, such as albuterol, during an asthma attack?
Why are cold mist vaporizers or tents contraindicated for patients with asthma?
Why are cold mist vaporizers or tents contraindicated for patients with asthma?
In the management of asthma, what is the primary function of inhaled corticosteroids?
In the management of asthma, what is the primary function of inhaled corticosteroids?
Which of the following findings from a chest X-ray is most indicative of Cystic Fibrosis?
Which of the following findings from a chest X-ray is most indicative of Cystic Fibrosis?
What is the primary action of recombinant human deoxyribonuclease (DNase) in the management of Cystic Fibrosis?
What is the primary action of recombinant human deoxyribonuclease (DNase) in the management of Cystic Fibrosis?
When should aerosol treatments be administered in relation to meals to avoid emesis?
When should aerosol treatments be administered in relation to meals to avoid emesis?
Which dietary modification is most appropriate for an infant with Cystic Fibrosis?
Which dietary modification is most appropriate for an infant with Cystic Fibrosis?
What is the rationale for providing salt supplements to individuals with Cystic Fibrosis, especially in warm weather?
What is the rationale for providing salt supplements to individuals with Cystic Fibrosis, especially in warm weather?
Why is a 72-hour fecal fat study often performed for patients who have Cystic Fibrosis?
Why is a 72-hour fecal fat study often performed for patients who have Cystic Fibrosis?
Which of the following best describes the administration sequence of aerosol medications and chest physiotherapy in Cystic Fibrosis?
Which of the following best describes the administration sequence of aerosol medications and chest physiotherapy in Cystic Fibrosis?
What information is conveyed by a sweat chloride test greater than 60 Meq/L?
What information is conveyed by a sweat chloride test greater than 60 Meq/L?
Which of the following is a key element in the patient education for a child with Cystic Fibrosis and their family, regarding signs and symptoms?
Which of the following is a key element in the patient education for a child with Cystic Fibrosis and their family, regarding signs and symptoms?
What is the role of fat-soluble vitamin supplementation (A, D, E, and K) in the treatment of Cystic Fibrosis?
What is the role of fat-soluble vitamin supplementation (A, D, E, and K) in the treatment of Cystic Fibrosis?
A patient with asthma is prescribed montelukast. For what purpose is this medication primarily used?
A patient with asthma is prescribed montelukast. For what purpose is this medication primarily used?
A patient with asthma is prescribed theophylline. Which of the following serum levels would indicate toxicity?
A patient with asthma is prescribed theophylline. Which of the following serum levels would indicate toxicity?
A patient's peak flow meter reading is in the yellow zone. According to the provided information, what does this indicate?
A patient's peak flow meter reading is in the yellow zone. According to the provided information, what does this indicate?
What is the primary reason premature infants are more susceptible to apnea?
What is the primary reason premature infants are more susceptible to apnea?
A patient is prescribed ipratropium bromide as part of their asthma management. What is the mechanism of action of this medication?
A patient is prescribed ipratropium bromide as part of their asthma management. What is the mechanism of action of this medication?
An infant experiencing an Apparent Life-Threatening Event (ALTE) typically presents with which sequence of symptoms?
An infant experiencing an Apparent Life-Threatening Event (ALTE) typically presents with which sequence of symptoms?
A child with asthma is using a metered-dose inhaler and spacer. Which of the following techniques demonstrates proper administration?
A child with asthma is using a metered-dose inhaler and spacer. Which of the following techniques demonstrates proper administration?
Which statement BEST describes the primary function of a home apnea monitor for infants?
Which statement BEST describes the primary function of a home apnea monitor for infants?
Which of the following is a significant recommendation for preventing Sudden Infant Death Syndrome (SIDS) related to the infant's sleeping environment?
Which of the following is a significant recommendation for preventing Sudden Infant Death Syndrome (SIDS) related to the infant's sleeping environment?
A four-channel pneumogram is performed on an infant. What primary information does this test provide which is critical for diagnosing apnea?
A four-channel pneumogram is performed on an infant. What primary information does this test provide which is critical for diagnosing apnea?
A premature infant receiving prolonged oxygen therapy and ventilation is at increased risk for which condition?
A premature infant receiving prolonged oxygen therapy and ventilation is at increased risk for which condition?
Which finding would indicate impaired gas exchange in an infant with Bronchopulmonary Dysplasia?
Which finding would indicate impaired gas exchange in an infant with Bronchopulmonary Dysplasia?
A 3-month-old infant is found unresponsive in their crib. Which of the following is associated with an increased risk of Sudden Infant Death Syndrome (SIDS)?
A 3-month-old infant is found unresponsive in their crib. Which of the following is associated with an increased risk of Sudden Infant Death Syndrome (SIDS)?
An infant with Bronchopulmonary Dysplasia exhibits which of the following clinical manifestations?
An infant with Bronchopulmonary Dysplasia exhibits which of the following clinical manifestations?
Which of the following is a primary goal in the treatment of infants with Bronchopulmonary Dysplasia?
Which of the following is a primary goal in the treatment of infants with Bronchopulmonary Dysplasia?
A child with a history of asthma presents with a sudden onset of difficulty breathing. What immediate assessment finding would be MOST concerning to a nurse?
A child with a history of asthma presents with a sudden onset of difficulty breathing. What immediate assessment finding would be MOST concerning to a nurse?
What does a decreased forced expiratory volume (FEV1) indicate in a child with asthma, during pulmonary function testing (PFTs)?
What does a decreased forced expiratory volume (FEV1) indicate in a child with asthma, during pulmonary function testing (PFTs)?
A child with asthma is prescribed Cromolyn Sodium. What is the PRIMARY purpose of this medication in their treatment plan?
A child with asthma is prescribed Cromolyn Sodium. What is the PRIMARY purpose of this medication in their treatment plan?
A nurse is providing education to the parents of a child newly diagnosed with asthma. Which statement indicates a NEED for further teaching?
A nurse is providing education to the parents of a child newly diagnosed with asthma. Which statement indicates a NEED for further teaching?
Which of the following findings would indicate the administration of humidified oxygen is necessary in a child with asthma?
Which of the following findings would indicate the administration of humidified oxygen is necessary in a child with asthma?
Which of these is a physiological effect when a child with asthma experiences bronchoconstriction?
Which of these is a physiological effect when a child with asthma experiences bronchoconstriction?
A child with asthma is experiencing an acute exacerbation and has been given a SABA. What outcome demonstrates the medication's effectiveness?
A child with asthma is experiencing an acute exacerbation and has been given a SABA. What outcome demonstrates the medication's effectiveness?
A patient with asthma is being monitored. Which finding would be MOST consistent with a compromised airway due to bronchoconstriction?
A patient with asthma is being monitored. Which finding would be MOST consistent with a compromised airway due to bronchoconstriction?
A child's asthma action plan indicates a 'yellow' zone. What does this signify?
A child's asthma action plan indicates a 'yellow' zone. What does this signify?
What is the rationale for advising individuals with respiratory issues like asthma or cystic fibrosis to avoid cold liquids?
What is the rationale for advising individuals with respiratory issues like asthma or cystic fibrosis to avoid cold liquids?
Which of the following is a consequence of altered electrolyte balance in Cystic Fibrosis?
Which of the following is a consequence of altered electrolyte balance in Cystic Fibrosis?
Which statement best explains why individuals with Cystic Fibrosis demonstrate steatorrhea?
Which statement best explains why individuals with Cystic Fibrosis demonstrate steatorrhea?
What is the primary reason for the use of a spacer with a metered-dose inhaler (MDI)?
What is the primary reason for the use of a spacer with a metered-dose inhaler (MDI)?
A 6-month old infant is experiencing difficulty passing their first stool. This finding may be indicative of:
A 6-month old infant is experiencing difficulty passing their first stool. This finding may be indicative of:
What is a common reproductive complication in males with cystic fibrosis?
What is a common reproductive complication in males with cystic fibrosis?
A patient with Cystic Fibrosis has chronic hypoxia; which of the following signs and symptoms is most likely to manifest?
A patient with Cystic Fibrosis has chronic hypoxia; which of the following signs and symptoms is most likely to manifest?
What is the primary reason for administering recombinant human deoxyribonuclease (DNase) to a patient with cystic fibrosis?
What is the primary reason for administering recombinant human deoxyribonuclease (DNase) to a patient with cystic fibrosis?
Why are fat-soluble vitamins often a necessary supplement for individuals with cystic fibrosis?
Why are fat-soluble vitamins often a necessary supplement for individuals with cystic fibrosis?
A 72-hour fecal fat study is performed on a child with suspected cystic fibrosis. What is the primary purpose of this diagnostic test?
A 72-hour fecal fat study is performed on a child with suspected cystic fibrosis. What is the primary purpose of this diagnostic test?
What is the most important reason for using bronchodilators in the treatment regimen for cystic fibrosis?
What is the most important reason for using bronchodilators in the treatment regimen for cystic fibrosis?
A patient with cystic fibrosis is undergoing postural drainage and percussion. At what point should aerosolized medications be administered in relation to this therapy?
A patient with cystic fibrosis is undergoing postural drainage and percussion. At what point should aerosolized medications be administered in relation to this therapy?
Why is it recommended to administer pancreatic enzymes with every meal and snack for patients with cystic fibrosis?
Why is it recommended to administer pancreatic enzymes with every meal and snack for patients with cystic fibrosis?
During periods of warmer weather, why might individuals with cystic fibrosis be advised to take salt supplements?
During periods of warmer weather, why might individuals with cystic fibrosis be advised to take salt supplements?
What is the primary role of mucolytic medications in managing cystic fibrosis?
What is the primary role of mucolytic medications in managing cystic fibrosis?
Which of the following should be emphasized in patient education in the context of cystic fibrosis?
Which of the following should be emphasized in patient education in the context of cystic fibrosis?
Why are aerosols typically administered before meals in patients with respiratory conditions such as cystic fibrosis?
Why are aerosols typically administered before meals in patients with respiratory conditions such as cystic fibrosis?
Flashcards
Traffic Light System for Asthma
Traffic Light System for Asthma
Green means good; yellow indicates caution; red signals the need for medication or inhaler.
Meter Dose Inhaler
Meter Dose Inhaler
An inhaler connected to a spacer to optimize medication delivery.
Asthma Triggers in Children
Asthma Triggers in Children
Factors like cold weather, allergies, smoke, and dust that can provoke asthma.
Cystic Fibrosis (CF)
Cystic Fibrosis (CF)
Signup and view all the flashcards
Chromosome Involved in CF
Chromosome Involved in CF
Signup and view all the flashcards
Clinical Manifestations of CF
Clinical Manifestations of CF
Signup and view all the flashcards
Steatorrhea
Steatorrhea
Signup and view all the flashcards
Infertility in CF
Infertility in CF
Signup and view all the flashcards
Asthma
Asthma
Signup and view all the flashcards
High mortality rates in asthma
High mortality rates in asthma
Signup and view all the flashcards
Diagnosis of Asthma
Diagnosis of Asthma
Signup and view all the flashcards
Pulmonary Function Tests (PFTs)
Pulmonary Function Tests (PFTs)
Signup and view all the flashcards
Signs of Respiratory Distress
Signs of Respiratory Distress
Signup and view all the flashcards
SABAs
SABAs
Signup and view all the flashcards
Inhaled Corticosteroids
Inhaled Corticosteroids
Signup and view all the flashcards
Positioning for Asthma
Positioning for Asthma
Signup and view all the flashcards
Manual postural drainage
Manual postural drainage
Signup and view all the flashcards
Respiratory Distress Syndrome (RDS)
Respiratory Distress Syndrome (RDS)
Signup and view all the flashcards
Hyaline Membrane Disease
Hyaline Membrane Disease
Signup and view all the flashcards
Clinical manifestations of RDS
Clinical manifestations of RDS
Signup and view all the flashcards
Exogenous Surfactant (Exosurf)
Exogenous Surfactant (Exosurf)
Signup and view all the flashcards
Mechanical ventilation
Mechanical ventilation
Signup and view all the flashcards
Bronchopulmonary Dysplasia (BPD)
Bronchopulmonary Dysplasia (BPD)
Signup and view all the flashcards
Growth and Development retardation
Growth and Development retardation
Signup and view all the flashcards
Cystic Fibrosis Diagnosis
Cystic Fibrosis Diagnosis
Signup and view all the flashcards
Sweat Chloride Test
Sweat Chloride Test
Signup and view all the flashcards
72-hour fecal fat study
72-hour fecal fat study
Signup and view all the flashcards
Goals of CF Treatment
Goals of CF Treatment
Signup and view all the flashcards
Recombinant DNase
Recombinant DNase
Signup and view all the flashcards
Pancreatic Enzymes
Pancreatic Enzymes
Signup and view all the flashcards
Aerosol Treatments Purpose
Aerosol Treatments Purpose
Signup and view all the flashcards
Mucolytics and Bronchodilators
Mucolytics and Bronchodilators
Signup and view all the flashcards
Postural Drainage
Postural Drainage
Signup and view all the flashcards
Patient Education in CF
Patient Education in CF
Signup and view all the flashcards
SIDS Risk Factors
SIDS Risk Factors
Signup and view all the flashcards
Apnea Definition
Apnea Definition
Signup and view all the flashcards
ALTE Symptoms
ALTE Symptoms
Signup and view all the flashcards
Caffeine for Apnea
Caffeine for Apnea
Signup and view all the flashcards
Home Monitoring for Apnea
Home Monitoring for Apnea
Signup and view all the flashcards
Diagnosis of BPD
Diagnosis of BPD
Signup and view all the flashcards
Treatments for BPD
Treatments for BPD
Signup and view all the flashcards
Sudden Infant Death Syndrome (SIDS)
Sudden Infant Death Syndrome (SIDS)
Signup and view all the flashcards
Risk factors for SIDS
Risk factors for SIDS
Signup and view all the flashcards
Chronic Inflammation in Asthma
Chronic Inflammation in Asthma
Signup and view all the flashcards
Bronchoconstriction
Bronchoconstriction
Signup and view all the flashcards
Bronchial Hyperresponsiveness
Bronchial Hyperresponsiveness
Signup and view all the flashcards
Respiratory Distress Signs
Respiratory Distress Signs
Signup and view all the flashcards
Peak Expiratory Flow Rate
Peak Expiratory Flow Rate
Signup and view all the flashcards
Short-Acting Beta-Agonists (SABAs)
Short-Acting Beta-Agonists (SABAs)
Signup and view all the flashcards
High Fowler's Position
High Fowler's Position
Signup and view all the flashcards
Signs of BPD in Diagnosis
Signs of BPD in Diagnosis
Signup and view all the flashcards
BPD Treatment Strategies
BPD Treatment Strategies
Signup and view all the flashcards
Pilocarpine
Pilocarpine
Signup and view all the flashcards
Aerosol treatments
Aerosol treatments
Signup and view all the flashcards
Mucolytics
Mucolytics
Signup and view all the flashcards
Bronchodilators
Bronchodilators
Signup and view all the flashcards
Pulmonary hygiene
Pulmonary hygiene
Signup and view all the flashcards
Fat Soluble Vitamins
Fat Soluble Vitamins
Signup and view all the flashcards
Genetic Counseling
Genetic Counseling
Signup and view all the flashcards
Antileukotrienes
Antileukotrienes
Signup and view all the flashcards
Theophylline Side Effects
Theophylline Side Effects
Signup and view all the flashcards
Peak Flow Meter Colors
Peak Flow Meter Colors
Signup and view all the flashcards
Asthma Management Steps
Asthma Management Steps
Signup and view all the flashcards
Severe Red in Asthma
Severe Red in Asthma
Signup and view all the flashcards
Cystic Fibrosis Inheritance
Cystic Fibrosis Inheritance
Signup and view all the flashcards
Exocrine Glands in CF
Exocrine Glands in CF
Signup and view all the flashcards
Pulmonary Complications in CF
Pulmonary Complications in CF
Signup and view all the flashcards
Cystic Fibrosis Symptoms
Cystic Fibrosis Symptoms
Signup and view all the flashcards
Nutritional Impact of CF
Nutritional Impact of CF
Signup and view all the flashcards
Clubbing of Nails in CF
Clubbing of Nails in CF
Signup and view all the flashcards
Meconium Ileus
Meconium Ileus
Signup and view all the flashcards
Albuterol
Albuterol
Signup and view all the flashcards
Peak Expiratory Flow Rate (PEFR)
Peak Expiratory Flow Rate (PEFR)
Signup and view all the flashcards
SABAs vs LABAs
SABAs vs LABAs
Signup and view all the flashcards
Positioning in High Fowler’s
Positioning in High Fowler’s
Signup and view all the flashcards
Pulse Oximetry
Pulse Oximetry
Signup and view all the flashcards
Theophylline
Theophylline
Signup and view all the flashcards
SABA Protocol
SABA Protocol
Signup and view all the flashcards
Peak Flow Meter
Peak Flow Meter
Signup and view all the flashcards
Cystic Fibrosis Clinical Manifestations
Cystic Fibrosis Clinical Manifestations
Signup and view all the flashcards
Mucus in CF
Mucus in CF
Signup and view all the flashcards
Sweat Electrolytes in CF
Sweat Electrolytes in CF
Signup and view all the flashcards
Nutritional Deficiencies in CF
Nutritional Deficiencies in CF
Signup and view all the flashcards
Steatorrhea in CF
Steatorrhea in CF
Signup and view all the flashcards
Meconium Ileus in CF
Meconium Ileus in CF
Signup and view all the flashcards
Crib Safety for Infants
Crib Safety for Infants
Signup and view all the flashcards
Treatment for Apnea
Treatment for Apnea
Signup and view all the flashcards
Study Notes
Chronic Respiratory Disorders
- Asthma is the most common pediatric chronic illness, also known as hyperreactive airway disease. Mortality rates are highest among inner-city African American and Hispanic youth.
- Asthma is characterized by chronic inflammation, bronchoconstriction, and bronchial hyperresponsiveness.
- Asthma triggers include smoke, strong emotions, colds, exercise, cockroaches, pollen, mold & mildew, food allergies, dust, furry pets, changes in the weather (cold weather), and strong smells.
- During an asthma attack, smooth airway muscles tighten, and air gets trapped in the alveoli. The airway walls become inflamed and thickened.
- Diagnosing asthma involves a client history, physical exam, chest X-rays (to rule out other diseases like pneumonia or lower respiratory tract infections), and pulmonary function tests (PFTs). PFTs measure the amount of air inhaled and exhaled, including forced expiratory volume, peak expiratory flow rate, diminished forced vital capacity, and diminished inspiratory capacity.
- Treatment for asthma includes frequent respiratory assessments, humidified oxygen if necessary, avoiding cold mist vaporizers or tents (as they can cause bronchospasm), administering pulse oximetry (to check O2 levels- 95% or normal), positioning the patient in high Fowler's position, and using various medications.
- Medications include SABAs (Albuterol, Proventil, Ventolin) for acute exacerbations, inhaled corticosteroids (Beclomethasone, Flonase, Budesonide), systemic corticosteroids (Prednisone, Prednisolone), inhaled NSAIDS (Cromolyn Sodium), antileukotrienes (Zafirlukast, Montelukast), anticholinergics (ipratropium bromide), systemic beta-2 agonists (Epinephrine, Theophylline, Breathine), and LABA (Advair).
- A combination of ICS + LABA is also used for maintenance.
Cystic Fibrosis
- Cystic fibrosis (CF) is the most common inherited autosomal recessive disorder. Both parents must carry the trait.
- CF affects exocrine glands that produce mucus, leading to alterations in sweat electrolytes (especially chloride) and mucus production.
- CF damages the pulmonary system (respiratory infection due to trapped mucus), GI tract (prevents nutrient absorption), intestinal tract, pancreas (blocks lipase and amylase, insulin needed for replacement), liver (impaired function), and the reproductive system. Symptoms include difficulty absorbing nutrients (causing weight loss), inability for the pancreas to produce enzymes, and possible infertility.
- CF increases the risk of pulmonary bacteria colonization.
- CF is more common in Caucasian children and less common in Asians or African Americans.
- Life expectancy has improved to 40-70 years.
- Diagnosis is made through a sweat chloride test (greater than 60 mEq/L), 72-hour fecal fat study (steatorrhea), and chest X-rays (showing patchy atelectasis and generalized obstructive emphysema).
Respiratory Distress Syndrome
- Respiratory distress syndrome (RDS) is caused by lung immaturity, specifically an immature pulmonary surfactant system, in preterm neonates.
- This condition leads to an insufficient amount of surfactant, which keeps alveoli open.
- Clinical manifestations include prematurity, tachypnea (greater than 60 breaths per minute), nasal flaring, expiratory grunting, diminished breath sounds, hypoxia, and respiratory acidosis.
- RDS treatment involves exogenous surfactant via endotracheal tube, mechanical ventilation with supplemental oxygen, maintaining a neutral thermal environment, correcting fluid and electrolyte imbalances, and chest physiotherapy.
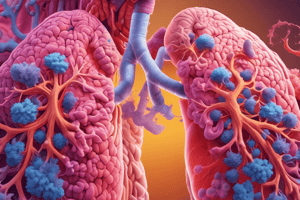
Bronchopulmonary Dysplasia (BPD)
- BPD is a chronic obstructive pulmonary disease found in premature infants after prolonged oxygen therapy and ventilation.
- High levels of oxygen and ventilation can damage the bronchial epithelium and alveoli.
- This leads to scarring, fibrosis, atelectasis (collapsed alveoli), poor gas exchange, and chronic low levels of oxygenation.
- BPD results in reduced lung compliance and altered respiratory function.
- Diagnosis might show lung changes with air trapping on X-rays (like emphysema) and abnormal blood gases (hypercapnia, respiratory acidosis).
- Treatment for BPD includes artificial airway, mechanical ventilation, suctioning prn, chest physiotherapy, medications (bronchodilators, corticosteroids, diuretics, and antibiotics) and patient education on CPR, home monitoring, and infection control.
Sudden Infant Death Syndrome (SIDS)
- SIDS is the unexplained death of an infant under one year old, where a post-mortem examination does not reveal a cause of death.
- It occurs most often in infants aged 3 months (90% before 6 months), with a higher frequency during winter months.
- The infant usually dies during sleep, and there are no disturbing signs or struggles.
- Risk factors include prematurity, low birth weight, male gender, and asphyxia in multiple births, as well as SIDS in siblings.
- Risk reduction strategies include placing babies to sleep on their backs, using cribs meeting safety standards, avoiding water mattresses and soft surfaces, avoiding secondary smoke, avoiding bottle feeding in cribs, avoiding overheating, avoiding co-sleeping, and monitoring for signs.
Apnea
- Apnea is an unintentional cessation of spontaneous breathing for more than 20 seconds.
- Apnea is more common in premature infants due to immature central respiratory centers.
- Common medications to manage apnea include caffeine and theophylline.
- Apparent Life-Threatening Events (ALTE) are usually central apnea events lasting longer than 20 seconds, with color changes (pale then cyanotic), marked muscle limpness, choking, or gagging.
- Diagnosis involves monitoring using 4-channel pneumograms over 24 hours, looking for periods of apnea.
- Treatment involves CPR / CPR classes, home monitoring (for up to one year) if needed, medications like theophylline and caffeine, support groups, and understanding when to call 911.
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.