Podcast
Questions and Answers
What is the primary role of vascular endothelial growth factor (VEGF) in tractional retinal treatment?
What is the primary role of vascular endothelial growth factor (VEGF) in tractional retinal treatment?
- Promotes neo-vascularization and contributes to atherosclerosis. (correct)
- Inhibits inflammation in retinal blood vessels.
- Helps in the absorption of excess cholesterol from the blood.
- Encourages the formation of a protective layer over the retina.
What condition may result from the alteration of AGE tissue due to high cholesterol levels?
What condition may result from the alteration of AGE tissue due to high cholesterol levels?
- Reduction of oxidative stress in retinal tissues.
- Tractional retinal detachment and potential hemorrhage. (correct)
- Increased blood flow to the retina.
- Complete retinal regeneration.
Why is the formation of a fibrovascular tuft considered a poor prognostic indicator in retinal health?
Why is the formation of a fibrovascular tuft considered a poor prognostic indicator in retinal health?
- It suggests insufficient cholesterol in the blood.
- It creates unnecessary traction on the retina. (correct)
- It leads to the formation of new protective blood vessels.
- It indicates excessive physical activity by the patient.
What lifestyle change is recommended to avoid complications associated with tractional retinal detachment?
What lifestyle change is recommended to avoid complications associated with tractional retinal detachment?
What is a characteristic feature of dysplastic nevus syndrome?
What is a characteristic feature of dysplastic nevus syndrome?
Which of the following is a leading cause of blindness in diabetics, particularly in underdeveloped countries?
Which of the following is a leading cause of blindness in diabetics, particularly in underdeveloped countries?
Which condition indicates a poor prognosis for metastasis?
Which condition indicates a poor prognosis for metastasis?
What does the Collar Button sign indicate?
What does the Collar Button sign indicate?
What diagnostic test is primarily used to assess fluid under the retina?
What diagnostic test is primarily used to assess fluid under the retina?
Which symptom typically results from ocular melanomas?
Which symptom typically results from ocular melanomas?
What is the primary cause of CNVM formation mentioned in the content?
What is the primary cause of CNVM formation mentioned in the content?
Which of the following complications is NOT associated with CNVM?
Which of the following complications is NOT associated with CNVM?
What results from an imbalance of promotors and inhibitors in CNVM formation?
What results from an imbalance of promotors and inhibitors in CNVM formation?
Which of the following factors may contribute to decreased blood flow, facilitating the development of CNVM?
Which of the following factors may contribute to decreased blood flow, facilitating the development of CNVM?
What condition is related to the thickening and calcification of Bruch's membrane?
What condition is related to the thickening and calcification of Bruch's membrane?
What is a potential outcome of serous fluid accumulation in retinal conditions?
What is a potential outcome of serous fluid accumulation in retinal conditions?
Which treatment approach is mentioned as a response to conditions involving CNVM?
Which treatment approach is mentioned as a response to conditions involving CNVM?
What type of hemorrhage is specifically associated with subretinal conditions?
What type of hemorrhage is specifically associated with subretinal conditions?
What is a key characteristic of papilledema?
What is a key characteristic of papilledema?
What is an indicator of increased intracranial pressure (ICP)?
What is an indicator of increased intracranial pressure (ICP)?
Which condition is primarily characterized by inflammation of the optic nerve?
Which condition is primarily characterized by inflammation of the optic nerve?
What could indicate a blockage of cerebrospinal fluid (CSF) flow?
What could indicate a blockage of cerebrospinal fluid (CSF) flow?
What symptom can occur with unilateral disc edema?
What symptom can occur with unilateral disc edema?
Which of the following is a feature of ischemic optic neuropathy?
Which of the following is a feature of ischemic optic neuropathy?
What might choroidal folds indicate?
What might choroidal folds indicate?
Papilledema is not caused by which of the following?
Papilledema is not caused by which of the following?
What is a common symptom of increased intracranial pressure associated with papilledema?
What is a common symptom of increased intracranial pressure associated with papilledema?
What condition is characterized by papilledema without obvious cause?
What condition is characterized by papilledema without obvious cause?
Which diagnostic test is recommended for evaluating acute papilledema?
Which diagnostic test is recommended for evaluating acute papilledema?
What is a significant sign of optic nerve issues that could lead to the presence of papilledema?
What is a significant sign of optic nerve issues that could lead to the presence of papilledema?
Which of the following describes a symptom that could indicate elevated intracranial pressure?
Which of the following describes a symptom that could indicate elevated intracranial pressure?
What is associated with 'axoplasmic stasis' in the context of increased intracranial pressure?
What is associated with 'axoplasmic stasis' in the context of increased intracranial pressure?
What imaging study is indicated for patients with suspected Grade 4 Hypertension related to papilledema?
What imaging study is indicated for patients with suspected Grade 4 Hypertension related to papilledema?
Which symptom is least likely to indicate increased intracranial pressure?
Which symptom is least likely to indicate increased intracranial pressure?
Flashcards are hidden until you start studying
Study Notes
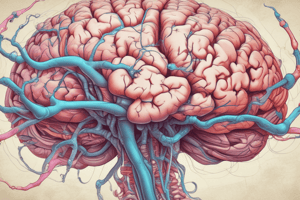
Choroidal Neovascularization (CNV)
- CNV is a new blood vessel formation in the choroid that grows up towards the RPE, and/or sensory retina.
- This is a common cause of vision loss in people with age-related macular degeneration (AMD).
- CNV can lead to subretinal hemorrhage, sub-RPE hemorrhage, or serous retinal detachment.
- Risk Factors:
- Age-related (aka, "aging pigment")
- Classic Risk Factors:
- Abnormal moles (nevi): Including dysplastic nevus syndrome (atypical moles)
- Genetic predisposition: Monosomy 3 (increased risk of metastasis to liver & aggressive tumor behavior) & trisomy 8 (increased risk of aggressive tumor behavior)
- Signs and Symptoms:
- Fundus autofluorescence (FAF): Lipofuscin pigment will glow.
- Low-dose intravenous radioactive phosphorus uptake test (p32 test)
- Ultrasounds: Tumors show acoustic hollowness (low to medium internal reflectivity).
- OCT: Fluid buildup under the retina (serous RD)
- Symptoms: Metamorphopsia (distorted vision), photopsias (flashes), visual field loss, decreased visual acuity (Snellen chart)
- Treatment:
- Anti-VEGF therapy: Injections aim to reduce the growth of abnormal blood vessels
- Observation: Visualized via fluorescein angiography. Hyperfluorescence in the angiogram indicates the presence of CNV.
- Avoid strenuous physical activity: Can lead to rupture of abnormal vessels.
Tractional Retinal Detachment (TRD)
- This is a type of retinal detachment caused by the growth of new blood vessels in the eye.
- The new blood vessels form a fibrous membrane (scaffolding) that pulls on the retina, causing it to detach.
- Common in diabetic patients, especially in developing countries.
- Causes:
- High blood sugar levels: Promote Protein Kinase C pathway activity and upregulate Vascular Endothelial Growth Factor (VEGF), which promotes angiogenesis (new blood vessel formation).
- Atherosclerosis: Thickening and narrowing of blood vessels due to genetics, UV exposure, and lifestyle factors (smoking, stress)
- Imbalance of Promoters/Inhibitors: Hypoxia and VEGF outweigh inhibitors, leading to ocular angiogenesis.
- Bruch's Membrane Thickening: Thickening and calcification of Bruch's membrane causes it to become brittle and break.
Papilledema
- Definition: Swelling and protrusion of the optic disc (where the optic nerve connects to the eye).
- Cause: Increased intracranial pressure (ICP)
- Pseudotumor cerebri (idiopathic intracranial hypertension - IIH): Common cause, especially in young women of childbearing age.
- Other causes: Brain tumor, space-occupying lesion, venous thrombosis, severe hypertension, and vitamin A toxicity.
- Mechanism:
- Blockage of CSF flow: Not overproduction of CSF
- Increased venous pressure: Increased pressure in the veins surrounding the optic disc
- This leads to axoplasmic stasis, a blockage of axoplasmic flow
- Signs and Symptoms:
- Typically bilateral: May appear unilateral if one eye has severe optic atrophy.
- Exam findings:
- Indistinct disc margins
- Venous engorgement
- Flame-shaped hemorrhages
- Anterior extension of the optic nerve head (ONH)
- Retinal (Paton) folds
- Choroidal folds
- Absence of physiological cup
- Macular star (hard exudates) along Henle's fibers
- Dilated veins
- Good visual acuity and pupil reactions (unless long standing --negative RAPD)
- Full visual fields (with an enlarged blind spot).
- Symptoms:
- Headaches (especially upon waking)
- Nausea/vomiting
- Lethargy
- 6th nerve palsy (CNS lesions & increased ICP)
- Transient obscuration (vision blackouts)
- Pulsatile tinnitus
- Loss of spontaneous venous pulsation
- Treatment:
- Emergency referral to a neurologist: Requires a CBC, SED rate, and brain imaging (MRI/CT scan)
- Focus on lowering CSF pressure:
- Immediate referral to an internist: If grade 4 hypertension (seen in young patients with kidney problems).
- MRI/MRV of brain and orbits: Complete within 24 hours to rule out venous sinus thrombosis, aneurysm or other intracranial issues.
Unilateral Papilledema
- Causes: Congenital variation in the subarachnoid space (no swelling will be apparent), atrophied optic disks, previous optic nerve issues.
- Potential causes of unilateral papilledema:
- Congenital Variation: Subarachnoid space terminating retrolaminarly.
- Atrophied Disks: May show reduced signs of edema.
- Past Optic Nerve Issues: Trauma or unilateral ischemic optic neuropathy.
- Important note: Unilateral papilledema may present as asymmetric.
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.