Podcast
Questions and Answers
Which of the following best describes the definition of cervical spine injury?
Which of the following best describes the definition of cervical spine injury?
- Injury or pain limited to the bony structures of the neck.
- Injury or pain to any structure within the neck or head superior to T1. (correct)
- Injury or pain to any structure within the neck or head superior to T2.
- Pain only in the muscles of the neck.
What percentage of patients with cervical/neck pain are hospitalized?
What percentage of patients with cervical/neck pain are hospitalized?
- 4% (correct)
- 16.7%
- 22.2%
- 75%
Which of the following is NOT a typical component of the examination and evaluation of a patient with a suspected cervical spine injury?
Which of the following is NOT a typical component of the examination and evaluation of a patient with a suspected cervical spine injury?
- Neurovascular assessment.
- Palpation.
- Lower extremity reflex testing. (correct)
- Active movement assessment.
When taking a patient's history, what kind of information is relevant regarding their symptoms?
When taking a patient's history, what kind of information is relevant regarding their symptoms?
Which of the following is considered a 'red flag' in the assessment of cervical spine pain?
Which of the following is considered a 'red flag' in the assessment of cervical spine pain?
According to the Canadian C-Spine Rules, what is the approximate sensitivity for identifying a fracture?
According to the Canadian C-Spine Rules, what is the approximate sensitivity for identifying a fracture?
During structural inspection, what should the area being examined be?
During structural inspection, what should the area being examined be?
Which of the following best describes the typical range of motion (ROM) during cervical side bending?
Which of the following best describes the typical range of motion (ROM) during cervical side bending?
During cervical rotation, where does the majority of the movement occur?
During cervical rotation, where does the majority of the movement occur?
What is a typical characteristic of normal cervical motion?
What is a typical characteristic of normal cervical motion?
What is the purpose of the Upper Quarter Assessment?
What is the purpose of the Upper Quarter Assessment?
Which of the following is an example of structural differentiation for the shoulder?
Which of the following is an example of structural differentiation for the shoulder?
During palpation, which of the following structures are assessed?
During palpation, which of the following structures are assessed?
In the context of PIVM grading, what does a grade of '0' indicate?
In the context of PIVM grading, what does a grade of '0' indicate?
During the Craniocervical Flexion Test (CCFT), what is the baseline pressure to which the blood pressure cuff is inflated?
During the Craniocervical Flexion Test (CCFT), what is the baseline pressure to which the blood pressure cuff is inflated?
What is the most common spinal level that is affected by a Cervical Herniated disc?
What is the most common spinal level that is affected by a Cervical Herniated disc?
Which of the following is a typical symptom associated with cervical spondylosis?
Which of the following is a typical symptom associated with cervical spondylosis?
Which of the following is a true statement regarding the Flexion-Rotation Test?
Which of the following is a true statement regarding the Flexion-Rotation Test?
Which of the following structures is NOT likely involved in the development of cervicogenic pain?
Which of the following structures is NOT likely involved in the development of cervicogenic pain?
According to the content, what type of alternative therapeutic approach was found to be more effective in relieving chronic nonspecific neck pain than a home-based manual for self-care?
According to the content, what type of alternative therapeutic approach was found to be more effective in relieving chronic nonspecific neck pain than a home-based manual for self-care?
Flashcards
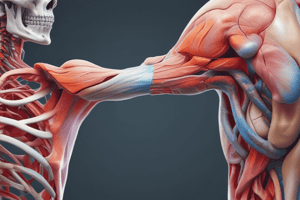
Cervical Spine Injury
Cervical Spine Injury
Injury or pain to any structure (muscle, bone, or soft tissue) within the neck or head superior to T1.
Cervical Red Flags
Cervical Red Flags
Severe pain unaffected by medication or position, may also include bowel/bladder dysfunction.
Active Motion Evaluation
Active Motion Evaluation
Visually observe for impairments and facet capsular patterns to detect instabilities.
Shoulder Ruling-Out Tests
Shoulder Ruling-Out Tests
Signup and view all the flashcards
Cervical Palpation
Cervical Palpation
Signup and view all the flashcards
Craniocervical Flexion Test (CCFT)
Craniocervical Flexion Test (CCFT)
Signup and view all the flashcards
Cervicogenic Pain
Cervicogenic Pain
Signup and view all the flashcards
Sharp Purser Test
Sharp Purser Test
Signup and view all the flashcards
Alar Ligament Stability Test
Alar Ligament Stability Test
Signup and view all the flashcards
Forward Head Posture
Forward Head Posture
Signup and view all the flashcards
Forward Head/Thoracic Spine
Forward Head/Thoracic Spine
Signup and view all the flashcards
Cervical Stenosis
Cervical Stenosis
Signup and view all the flashcards
Cervical Radiculopathy
Cervical Radiculopathy
Signup and view all the flashcards
Cervicogenic Pain
Cervicogenic Pain
Signup and view all the flashcards
Whiplash Signs and Symptoms
Whiplash Signs and Symptoms
Signup and view all the flashcards
Study Notes
- Cervical spine injury includes injury or pain to any structure within the neck or head superior to T1.
- Most visits for cervical/neck pain are to physician offices (75%), while only 4% of patients are hospitalized.
- Point prevalence of cervical/neck pain ranges from 5.9% to 22.2% in adults aged 15-75.
- One-year prevalence of cervical/neck pain varies from 16.7% to 75.1%, depending on the study.
- Examination and evaluation includes initial observation, history and interview, structural inspection, active movement, neurovascular assessment, palpation, upper quarter assessment, summary of findings, and intervention/Rx plan.
History & Interview
- Includes onset and mechanism of injury.
- Includes symptom descriptions (constant/varies, static/motion, radiating).
- Includes usual activities and positions, noting what makes it better or worse.
- Additional questions for HA, blurred vision, ringing in the ears, difficulty walking, and whether the condition is getting worse or better are helpful.
Red Flags
- Severe unremitting pain should raise concerns.
- Pain unaffected by medication or position is a red flag.
- Severe night pain, or severe pain with no history of injury are concerning.
- Change in function of bowels and bladder are red flags.
- Chest pains or elevated temperature (especially if prolonged) require attention.
Fracture?
- Use Canadian C-Spine Rules to identify if the patient has symptoms of a fracture
- Sensitivity = 99
- LR- = 0.01
Structural Inspection
- The area should be exposed to get an accurate assessment.
- Observe true posture, both sitting and standing.
- Note symmetry.
Active Motion
- Detect and observe any impairments to movement.
- Differentiate facet capsular pattern from myofascial pattern.
- Detect any instabilities.
- During Forward Bending, the facets are at 45 degrees, and translate up & forwards and the spinal canal lengthens for about 35 degrees
- During Backward Bending, facets translate down & back and the spinal canal narrows and shortens for about 70 degrees
- Side bending occurs at approximately 20 to 45 degrees, and the facet closes on the ipsilateral side and opens on the contralateral side, watch for substituting
- Rotation occurs at approximately 70 to 90 degrees, majorly at the atlanto-axial joint on the M/C (rotation and SB occur to the same side) and S/C (rotation and SB occur to the opposite side)
- Normal motion is smooth, "Full" ROM and pain free.
- Adequate relaxation of the antagonists is also important.
Characteristics of Abnormal Motion
- Limited range should raise concerns.
- Includes unwillingness to move and pain during or at end range, and any compensatory or "trick" movements.
Neurovascular Assessment
- Includes reflexes and nerve tension signs (Spurlings, distraction, ULTT, Lhermitte's sign, etc).
- Vascular test (Vertebral artery), muscle weakness, and skin sensation should be checked.
Upper Quarter Assessment
- Assesses the effects of the extremities on the spine, and vice versa, to determine treatment needs.
Structural Differentiation
- Ruling out the shoulder can be accomplised via Neers Impingement, Hawkins Kennedy Test and Shoulder Overpressure tests
- Ruling out the thoracic spine can be accomplised via PA's of the Thoracic Spine, assessing pain with breathing and Overpressure
Palpation
- Soft tissue differences, structure, and temperature should be assessed.
- Assess passive intervertebral motion (PIVMs) of the clavicle and scapula (levator scapulae, supraspinatus, articular pillars & facets, transverse processes).
- Palpate for the first rib.
PIVM Grading System
- 0 Ankylosis
- 1 Considerably Restricted
- 2 Slightly Restricted
- 3 Normal
- 4 Slightly Increased
- 5 Considerably Increased
- 6 Unstable
PIVM Technique
- Position the patient relaxed, well-supported, region in neutral, informed, securely on the table
- The operator should be relaxed & comfortable, table at appropriate heights, patient close to therapist and firm contact
Central Posterior Anterior Mobilization (CPS's) protocol:
- Baseline
- Move to first point of pain
- Move past first point of pain to end range
- Assess if concordant
- Repeat on opposite side
Unilateral Posterior Anterior protocol:
- Baseline
- Move to first point of pain
- Move past first point of pain to end range
- Assess if concordant
- Repeat on opposite side
Craniocervical Flexion Test (CCFT)
- Inflate blood pressure cuff to 20 mmHg (baseline).
- Perform chin tuck to 22 mmHg, hold for 10 sec, rest for 10 sec.
- Next at 24 mmHg, then 26 mmHg and finally 28 mmHg, holding each for 10 secs, with 10 secs of rest time, if overcompensating or unable to hold position, STOP before 30 mmHg
Jull Test for Endurance
- Should perform a chin retraction and lift head 1 inch off mat, and the test should be stopped if overcompensating or unable to hold position
- Record the time and the results should be; 38.9 seconds for men and 29.4 seconds for women
Cervical Endurance HEP
- Towel-assisted chin tuck
- Standing chin tuck with resistance band
- Quadruped chin tuck with/without resistance bands
Lateral Lift Test
- Lie patient on side
- Instruct the patient to lift neck to midline position and time the neck
- Repeat on opposite side and then compare ratio of side to side
Posterior Neck Endurance Test
- Hold for as long as you can while maintaining chin retraction
- Timed test
- Load can be added to the head to increase the difficulty
Scapular Endurance Test
- Hold as long as you can
- Keep the shoulders and elbows at 90 degrees
- ER while holding the ruler
Additional Muscle Performance Testing Considerations
- Shoulders
- Mid trapezius
- Lower trapezius
- External rotators
LAB-Observation
- Overall impression
- Body type
- Skin, muscle, etc
- Muscle tone
- Posture
- Symmetry
Lab-AROM considerations
- Verbal commands
- Ease of performance
- Recruitment of vertebra
- Trick movements
Lap-Palpation/Neuro (sitting vs supine)
- While the patient is Sitting include PROM and C7-T1
- While the patient is Supine include sternoclav/AC joint, 1st rib, TP and Articular pillars
- Assess Reflexes, Sensation, Strength and ULTTS (both sitting and Supine)
Lap-Palpation/Neuro for PIVM
- Supine: include Lateral glides
- Prone: check if bilateral or unilateral
Temporomandibular Joint
- The TMJ can cause neck dysfunction and contribute to neck pain
TMJ Movement
- Depression (gravity muscles) - lateral pterygoid
- Elevation (antigravity muscles) - masseter, temporalis & medial pterygoid
- Protrusion - lateral & medial pterygoid
- Retraction - posterior fibers of temporalis
- Side to side or lateral movements - lateral & medial pterygoid (left lateral pterygoid with right medial pterygoid turn the chin to left side & vice versa)
Movement Dysfunction
- Movement dysfuction can be displayed either; Disc displacement with reduction, or Disc displacement without reduction
Anterior Disc Displacement with Reduction
- Mouth closed-anterior and medial to condyle
- Opening - condyle moves over posterior band of disc and then returns to normal condyle disc relationship
- Closing - condyle slips posteriorly, rests on retrodiscal tissue, disc returns to anterior and medial displaced position
- Symptoms include joint tenderness, clicking - during opening and a closing click can also be elicited
Disc Displacement Without Reduction
- Condyle does not translate anteriorly to its full extent
- No clicking (lack of translation of condyle over posterior aspect of the disc)
- Symptoms such as history of clicking and popping in TMJ (past now now) and Limited mandibular ROM
- Signs include No TMJ sounds, limited mouth opening, deviation of mandible to affected side and decreased lateral excursions to contralateral side
TMJ Dysfunction
- Popping
- Locking
- Pain (especially on the neck, teeth or ear)
- Headaches
- Altered movement
Wilkes Classification
- Early stage: stage 1 (mild disc displacement with normal disc morphology and reduction relative to condyle with mouth opening
- Stage 2: Mild to moderate disc displacement and deformity, but there is reduction with opening
- Stage 3: Disc displacement, deformity and non reduction of disc with opening, but has shown to best respond to surgery
- Later stage: stage 4 (severe displacement, deformity, shortening or rarely elongation and non reduction of disc)
- Stage 5: Perforation of disc attachments, severe derangement of joint (Regressive remodeling/osteoarthritis)
TMJ Treatment
- Education is critical
- Joint mobilization and massage
- Modalities such as US and Iontophoresis
- Night splints
- Surgery may be needed
Most Common Problems
- Cervical disc disorder such as herniated disc
- Cervical degenerative disorders such as spondylosis/spondylolysis and Stenosis (myelopathy and radiculopathy)
- Headaches (Cervicogenic headache)
- Cervical neck injuries (Whiplash associated disorder)
Cervical Herniated Disc
- Usually C6-7
- May see sensory, muscle, and reflex changes
- Generally sharp pain with extension
- Usually young
- Often with hold their head in opposite SB, rotation and flexion
- "Flattened" neck posture
Causes-Herniated Disc
- Herniated discs may occur when excessive force is exerted on a cervical intervertebral disc such as a car accident or a traumatic fall
- A herniated disc is classified into one of three categories:
- Soft herniation of nucleus material
- Mixed soft-calcified herniation of disc material and calcified structures
- Calcified disc herniation
- A soft herniated disc (category 1) is more commonly in occurrence in younger populations
- Categories 2 and 3 are very common during degenerative processes to the neck
Referral Pain from C Spine
- Cervical disc lesions can cause pain in the T Spine
- Refer symptoms to T spine and especially to medial borders of scapula ("Cloward areas" = discogenic pain), especially very common after whiplash injuries
Treatments for the C spine
- Treatments can include selected manual techniques, traction and positional based active and passive exercises
Cervical Spondylosis
- Ubiquitous over the age of 40 years
- Levels most affected include C5-C6 and C6-C7, while the level least affected is C2-C3
- Is related to instability, as disc degeneration is an ubiquitous condition with mild to no reported symptoms and Disc degeneration concurrent with zygapophyseal and uncovertebral degeneration
Clinical Instability
- Clinical cervical is one element of cervical pain, and may contribute to cervicogenic headaches, chronic whiplash dysfunction, rheumatoid arthritis, osteoarthritis and segmental degeneration, situations involving trauma, genetic predisposition, disc degeneration and surgery
Symptoms
- Stiffness
- Diffuse pain
- Headaches (occasionally)
- Frequent need of manipulation
- Rarely complain of neurological signs
- Usually younger
- Women > men
- Usually associated with some trauma or long term postural disorder
Leads to Degeneration
- The degenerative process can lead to reduced disc height and bulging of the posterior aspect of the disc into the spinal canal
- Surrounding bones and ligaments of the spinal joints thicken and enlarge, collectively pushing into the spinal canal or nerve roots
- Stenotic changes may cause radiculopathy in isolation but will often coincide with a disc herniation or degradation
Treatment
- Can include:
- Active movement, mobilization/manipulation, general conditioning exercises and stretching
Cervical Stenosis
- Stenosis stands for narrowing
- This dysfunction can lead to myelopathy or radiculopathy (can be lateral or central or both)
- Can be caused from herniated disc, degeneration, or other factors associated with range loss
Cervical Myelopathy
- Cervical spondylotic myelopathy is the most common cause of spinal cord dysfunction in older people
- Signs and symptoms: characteristic symptoms (leg stiffness, hand weakness) includes characteristic signs such as hyperreflexia, atrophy of hands
- Diagnosed via MRI or CT (showing spinal stenosis and cord compression as a result of osteophytic overgrowth, disc herniation, ligamentum hypertrophy)
Cervical Radiculopathy
- Cervical radiculopathy is a pathological consequence in the cervical region associated with degenerative changes, a herniated disc, or other less common phenomena
- Cervical radiculopathy has a reported prevalence of 3.3 cases per 1,000 people and predominantly occurs in the fourth or fifth decades of life
- Symptoms associated with this disorder include pain that radiates from the neck to the extremities or body, with the symptoms generally represented by pain, numbness and/or weakness
Upper Limb Tension Test (Median Nerve Bias) has been shown in studies
- Sensitivity = 97
- LR-= 0.14
- Helps rule out the presence of cervical radiculopathy when performed early in the examination
Spurling's Test
- Specificity = 92
- LR+ = 4.87
- Rules in presence of cervical radiculopathy
Cervical Radiculopathy occurs when there is...
-
- Spurling's
- ROM <60 deg
-
- Distraction
-
- ULTT
- 2 of 4 positive is a LR+ of 0.80
- 3 of 4 positive is a LR+ of 6.1
- 4 of 4 positive is a LR+ of 30.3
- Sens = 24, spec = 99
Benefit of Cervical Traction
- Intermittent better than continuous (for pain reduction)
- Only one quality study
- Actually demonstrated more benefit for mechanical neck pain
Manual Traction Progression
- Distraction (light force, patient response)
- Rotation away
- Rotation back
- Release distraction
- *Continue process slowly working toward rotation to the same side as the pain
Identification of Cervicogenic Pain
- Head pain that spreads below the occiput is likely to originate from the atlantoaxial joint and can be distinguished from other types of headaches
- Structures may include muscle, facet joint, capsule, ligament, nerves, dura mater, spinal cord or vertebral artery
Location of Symptoms
- In C6 - frontal
- C1 - orbital
- C1-2 temporal
- Tension occipital areas
- C2-3 parietal
- Pain is usually unilateral (can be bilateral) and does not change sides like a migraine
Precipitating Events
- Pain has been described as an ache with a deep boring quality and may be accompanied by dizziness, light-headedness, nausea, visual disturbances and tinnitus
- Cervical headache is commonly continuous and can occur daily or two to three times during a week with fluctuating intensity
- Pain is often present upon waking that increase throughout the day and is commonly precipitated by neck movement or a sustained neck posture
Differentiation
- Cervical headaches are not confined to bouts or attacks (fluctuate according to circumstance)
- Most have 2 or more headaches a week and 58% will awake with their headache
- Emotional tension is a precipitating factor
- Cervical tender points can significantly influence the headache
Range of Motion Loss includes...
- Rotation defecit (26 degrees)
- Side flexion deficit (6 degrees)
- Flexion/extension deficit (23 degrees)
Differentiation protocol
- For the C2-3 segment: Palpate the C2 facet and mobilize straight down toward the patient's throat
- For the C1-2 segment: Rotate the head 30 degrees to the same side then perform the same mobilization, this time aiming at the patient's mouth and when rotated, the Alar ligament stabilizes the C2-3 segment, allowing more movement in the C1-2
C1-C2 PA Mobilization
- Sensitivity = 62
- Specificity = 87
- LR+ = 4.9
- LR- = 0.43
Flexion-Rotation Test
- Sensitivity = 86%
- Specificity = 100
- LR+ = 18+
- Rules in and out the presence of a cervicogenic headache with an origin at C1-2
Treatment protocol
- Treatments will include focused strengthening exercises and mobilizations/manipulation as well as massage/stretching
Incidence of Whiplash Associated Disorder
- Common with 120,000 cases per year, split into 10,000 per month, 2,307 per week, 328 per day, 13 per hour
Etiology
- May involve tearing of the anterior or posterior muscles, rupture or tear of Alar ligament and rupture or tear of Transverse ligament, including hypermobility of the upper or mid cervical segments
Signs and Symptoms
- Pain and aching to the neck and back, referred pain, to the shoulders, sensory disturbance (such as pins and needles) to the arms and legs, and headaches
- Symptoms can appear directly after the injury, but often are not felt until days afterwards
HyperSensitive
- Patients with chronic WAD displayed lower reflex thresholds than healthy subjects
- These findings provide objective electrophysiological evidence for generalized spinal cord hyper-excitability
Prognosis
- Expect symptoms to persist at least 6 months Common to see postural changes
- Origin of lengthy prognosis from Alar and Transverse ligament instability from Transverse ligament or Anterior local muscle group tears
Sharp Purser Test
- Neck in semi flexion (active)
- Palm of one hand on forehead
- Index finger on spinous process of C2
- Posterior force through forehead
- Positive posterior slide indicates AA instability
Alar Ligament Stability Test
- Three potential steps
- Stabilize the C2 spinous process by grabbing it firmly, laterally
- Slide flex the head with opposite arm (feel for movement at C2)
- Rotate the head with opposite arm (feel for movement at C2)
Treatment considerations
- Modalities
- General strengthening exercises
- General manual therapy procedures
Mobilization Has Best Evidence for Acute Whiplash
- Light mobilizations demonstrate the most evidence in treatment of acute whiplash
- Limited evidence for manipulations
- Transient evidence for modalities
Mechanism (Origin of Pain)
- Maintaining a postural preference, the patient puts normal tissue under abnormal mechanical stress by hanging their spinal joints at end range in certain positions (some tissues are getting unduly stretched while others are unduly shortened)
- Repeated undue stretching probably leads to many of the dysfunctions and derangements people over thirty experience
Common Postural Conditions
- Upper crossed syndrome can result in cervical headache which is commonly precipitated or aggravated by sustained neck posturing or neck movements
- Forward head posture is associated with TMD, chronic headaches, weakness of the anterior neck flexors and weakness of the lower trapezius
- FHP changes the balance between the flexors and extensors of the neck, and mediated the relationship between thoracic kyphosis and cervical ROM, specifically general cervical rotation and flexion
- Addressing FHP can improve cervical impairments as the FHP results also suggest that addressing thoracic kyphosis impairments may constitute and “upstream” approach
Treatment considerations
- General conditioning exercises and stretching
- Selected manual techniques
- Positional based active and passive exercises
Neck Classification
- Pain control - stabilize and palliative
- Mobility - mobilization or manipulation
- Exercise and conditioning (non-mobilization)
- Headache - mobilization and postural treatment
- Centralization - traction group
Thoracic Manipulation
- Thoracic Manipulation is typically needed, as thoracic manipulation has a better response than e-stim, infrared, mobilization to the thoracic spine and exercises, but is not better than treatment directed specifically to the neck
Home Exercise or Spinal Manipulation
- Studies find There is no difference at 8 weeks to 6 months in pain or disability between spine manipulation or home exercise and advice
- Both were better than medication only at all time points
Posterior Glides in Sitting protocol
- Stabilize at the spinous process the level below you are interested in facilitating
- Using the head as the lever, push upward and posterior
- Block at the spinous process
Side Flexion in Sitting Protocol
- Stand behind the patient
- Loop their arm over your bent knee
- Block at C7 or T1, with your thumb
- Side flex the head away from your knee, toward the blocked side
- Side flex the body of the patient away from the movement direction of the neck
Thoracic Extension in Sitting Protocol
- Ask the patient to lock their arms
- Block the thoracic region at the targeted level
- Use your knee to assist in stabilization
- Ask the patient to move “with you" during the glides
Anterior Cervical Stabilization
- Chin retraction to create a skin fold below the mandible
- Clinician removes hand support under head
- Patient holds position maintaining skin fold under mandible
- The exercise involves endurance
Posterior Strengthening Exercise
- Can target posterior cervical spine multifidi
- Stabilize T2 with belt
Upper Extremity Strengthening Considerations
- Low to moderate quality evidence to show that upper extremity stretching and strengthening does not have enough utility to be used exclusively
Yoga, Aerobics
- Yoga was more effective in relieving chronic nonspecific neck pain than a home-based manual for self care
- The data for Aerobics is not available.
- Other alternative approaches, are also not available.
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.