Podcast
Questions and Answers
What is a benefit of using centrally acting non-opioid analgesics?
What is a benefit of using centrally acting non-opioid analgesics?
- Increased risk of respiratory depression
- Increased risk of abuse
- Reduced risk of physical dependence (correct)
- Increased risk of neurotoxic effects
What is a result of chronic opioid use?
What is a result of chronic opioid use?
- Increased release of analgesic mediators
- Release of proinflammatory cytokines and chemokines (correct)
- Decreased release of inflammatory mediators
- Release of anti-inflammatory cytokines
What is a mechanism of action of αlpha2 Adrenergic Agonists?
What is a mechanism of action of αlpha2 Adrenergic Agonists?
- Inhibit pain in ventral horns
- Stimulate norepinephrine release
- Inhibit α2 adrenergic receptors on sympathetic pre-ganglionic neurons
- Activate α2 adrenergic receptors on sympathetic pre-ganglionic neurons to inhibit NE released (correct)
What is an effect of neuraxial clonidine? (select 2)
What is an effect of neuraxial clonidine? (select 2)
What is a characteristic of clonidine?
What is a characteristic of clonidine?
What is the mechanism of action of ketamine in the dorsal horn?
What is the mechanism of action of ketamine in the dorsal horn?
What is the primary mechanism of action of midazolam in the spinal cord?
What is the primary mechanism of action of midazolam in the spinal cord?
What is the primary effect of ziconotide (snail poison) on the spinal cord?
What is the primary effect of ziconotide (snail poison) on the spinal cord?
What is the primary mechanism of action of baclofen in the spinal cord?
What is the primary mechanism of action of baclofen in the spinal cord?
What is the primary effect of dexmedetomidine on the spinal cord?
What is the primary effect of dexmedetomidine on the spinal cord?
What is the primary effect of tramadol?
What is the primary effect of tramadol?
What is the primary effect of ketorolac on the spinal cord?
What is the primary effect of ketorolac on the spinal cord?
Which of the following neuraxial analgesics is contraindicated in obstetric patients?
Which of the following neuraxial analgesics is contraindicated in obstetric patients?
What are common side effects of neuraxial a2 agonists?
What are common side effects of neuraxial a2 agonists?
What is the mechanism of action for baclofen?
What is the mechanism of action for baclofen?
What is the effect of COX1 inhibition on platelet function?
What is the effect of COX1 inhibition on platelet function?
What is the site of action for peripherally acting analgesics?
What is the site of action for peripherally acting analgesics?
What is the function of COX1 in the GI tract?
What is the function of COX1 in the GI tract?
What is the consequence of hypoalbuminemia on NSAID pharmacokinetics?
What is the consequence of hypoalbuminemia on NSAID pharmacokinetics?
What is the primary site of NSAID metabolism?
What is the primary site of NSAID metabolism?
What is the effect of COX2 selective inhibitors on platelet aggregation?
What is the effect of COX2 selective inhibitors on platelet aggregation?
What is the effect of high doses of NSAIDs on the risk of ulcers, perforation, and bleeding?
What is the effect of high doses of NSAIDs on the risk of ulcers, perforation, and bleeding?
What is the effect of NSAIDs on the excretion of sodium?
What is the effect of NSAIDs on the excretion of sodium?
What is the effect of COX1 inhibition on the production of prostaglandins?
What is the effect of COX1 inhibition on the production of prostaglandins?
What is the mechanism by which NSAIDs increase the risk of anaphylaxis?
What is the mechanism by which NSAIDs increase the risk of anaphylaxis?
Which of the following patients is at a higher risk of developing bronchoconstriction when taking NSAIDs?
Which of the following patients is at a higher risk of developing bronchoconstriction when taking NSAIDs?
What is the mechanism by which aspirin prevents the production of prostaglandins?
What is the mechanism by which aspirin prevents the production of prostaglandins?
What is the effect of NSAIDs on the platelet aggregation?
What is the effect of NSAIDs on the platelet aggregation?
What is the leading cause of acute liver failure in the US?
What is the leading cause of acute liver failure in the US?
Which COX enzyme is associated with renal function, gastric mucosal protection, and platelet function?
Which COX enzyme is associated with renal function, gastric mucosal protection, and platelet function?
Which enzyme is associated with pain, inflammation, and fever mediation?
Which enzyme is associated with pain, inflammation, and fever mediation?
What is COX in relation to arachidonic acid?
What is COX in relation to arachidonic acid?
What is the mechanism of action of NSAIDs on prostaglandin biosynthesis?
What is the mechanism of action of NSAIDs on prostaglandin biosynthesis?
Moderate to severe liver and renal disease impair NSAID metabolism and elimination
Moderate to severe liver and renal disease impair NSAID metabolism and elimination
What is a benefit of selective COX-2 inhibitors?
What is a benefit of selective COX-2 inhibitors?
What is the mechanism by which NSAIDs are associated with increased risk of cardiovascular events? (select 2)
What is the mechanism by which NSAIDs are associated with increased risk of cardiovascular events? (select 2)
What is the least risky NSAID to administer to a patient with cardiovascular disease?
What is the least risky NSAID to administer to a patient with cardiovascular disease?
How do NSAIDs affect GFR?
How do NSAIDs affect GFR?
COX-2 inhibitors inhibit the vasodilatory properties of _____
COX-2 inhibitors inhibit the vasodilatory properties of _____
What are some complications of NSAID use?
What are some complications of NSAID use?
What effect does acetaminophen have on neurotransmission at the spinal cord level?
What effect does acetaminophen have on neurotransmission at the spinal cord level?
What is true about the effect of aspirin on platelet aggregation?
What is true about the effect of aspirin on platelet aggregation?
Aspirin overdose results in ____
Aspirin overdose results in ____
What is the mechanism of action of corticosteroids?
What is the mechanism of action of corticosteroids?
Which of the following steroids has the greatest anti-inflammatory potency? (select 2)
Which of the following steroids has the greatest anti-inflammatory potency? (select 2)
Less potent corticosteroids (e.g. methylprenisolone, prednisone) tend to have shorter durations of action
Less potent corticosteroids (e.g. methylprenisolone, prednisone) tend to have shorter durations of action
What are many of the untoward effects of steroids associated with?
What are many of the untoward effects of steroids associated with?
What is the primary corticosteroid against which the pharmacologic properties of various synthetic corticosteroids are judged?
What is the primary corticosteroid against which the pharmacologic properties of various synthetic corticosteroids are judged?
What is the effect of mineralocorticoids on the body?
What is the effect of mineralocorticoids on the body?
What is the primary function of glucocorticoids, such as cortisol (hydrocortisone)?
What is the primary function of glucocorticoids, such as cortisol (hydrocortisone)?
What is the primary function of mineralocorticoids, such as aldosterone, in the body?
What is the primary function of mineralocorticoids, such as aldosterone, in the body?
What do steroids do in relation to anesthesia?
What do steroids do in relation to anesthesia?
What is the mechanism of action of IV lidocaine, oral mexiletine, and tocainide?
What is the mechanism of action of IV lidocaine, oral mexiletine, and tocainide?
What is the mechanism of action of capsaicin?
What is the mechanism of action of capsaicin?
Ketamine can be used as a local anesthetic due to its ____ channel blocking ability
Ketamine can be used as a local anesthetic due to its ____ channel blocking ability
What is the mechanism by which opioids injected locally produce potent analgesic effects?
What is the mechanism by which opioids injected locally produce potent analgesic effects?
Where do peripheral analgesics primarily act to block transmission of pain impulses to higher cortical structures?
Where do peripheral analgesics primarily act to block transmission of pain impulses to higher cortical structures?
Study Notes
Centrally Acting Non-opioid Analgesics
- Widespread dependence, misuse, and abuse of opioids have driven the exploration of alternative analgesia modalities
- Opioids have limited efficacy for managing non-cancer chronic pain
- Non-narcotic medications relieve pain by mechanisms unrelated to opioid receptors, and do not cause respiratory depression, physical dependence, or abuse
Neuroaxial Use of Centrally Acting Non-Opioid Analgesics
- Higher CSF concentrations are achieved by bypassing the blood-brain barrier
- Agents act through different mechanisms than opioids
- May allow elimination or reduction in opioid use
- Caution: Neurotoxic effects of some compounds are unknown
α2 Adrenergic Agonists
- Clonidine and Dexmedetomidine are examples
- Mechanism of Action:
- Activate α2 adrenergic receptors on sympathetic pre-ganglionic neurons, reducing norepinephrine release
- Stimulation of α2 adrenergic receptors decreases norepinephrine in the brain, causing decreased wakefulness, decreased blood pressure in smooth vessels, and inhibition of pain in the dorsal horn
- Result: leading to analgesia, hypotension, bradycardia, and sedation
Neuraxial Clonidine
- Clonidine is a selective partial α2 receptor agonist
- Inhibits nociceptive impulses at post-junctional α2 receptors in the dorsal horn
- Prolongs local anesthetic analgesia and reduces postoperative opioid requirements
- Prolongs sensory and motor block of local anesthetics
- Acts synergistically with neuraxial opioids
- Black box warning in obstetric patients
- Anti-hyperalgesic properties
Dexmedetomidine
- Selective α2 receptor agonist
- Higher receptor affinity and selectivity for α2 receptors than clonidine
- Fewer hemodynamic systemic effects
- Intrathecal dose: 3 ug
- No neurotoxicity reported for intrathecal or epidural administration
- Major side effects: bradycardia and hypotension
Epidural Dexmedetomidine
- Prolongs neuraxial sensory and motor blockade
- Decreases intraoperative anesthetic requirements
- Improves postoperative analgesia
- Decreases heart rate and blood pressure in cesarean sections
- Black box warning for hypotension and bradycardia in cesarean sections
Neuraxial Neostigmine
- Neostigmine inhibits acetylcholinesterase, preventing the metabolism of acetylcholine
- Analgesic effects due to stimulation of muscarinic cholinergic receptors
- Prolongs analgesia with minimal side effects with intrathecal (10-100 ug) or epidural (100-200 ug) use
- High incidence of nausea (50-100%)
- Does not affect motor blockade
Ketamine
- Non-competitive antagonism of NMDA (glutamate) receptors in the dorsal horn
- Mechanism of Action:
- Counts the release of glutamate, aspartate, and neurokinin
- These neurotransmitters are linked to central sensitization, windup, and other elements of neuroplasticity
- Ketamine counters these effects
Neuraxial Ketamine
- Intrathecal use is limited due to the risk of neurotoxicity
- Epidural dose: 10-30 mg produces excellent postoperative analgesia
- Synergist with opioids
- Use of preservative-free solutions is mandatory
- Side effects: headache, sedation, transient burning pain with injection, and hints at possibility of neurotoxicity
Neuraxial Midazolam
- Intrathecal midazolam increases the affinity of GABA for the GABAA receptor
- The transmembrane conductance of chloride results in hyperpolarization of the neuron, reducing action potential propagation
- High density of GABAA receptors in the dorsal horn of the spinal cord
- Intrathecal (1-2 mg) or epidural midazolam has an analgesic effect and may be beneficial for treating perioperative and chronic pain
- Epidural midazolam reduces postoperative nausea and vomiting
Tramadol
- Binds to mu receptors
- Inhibits serotonin and norepinephrine uptake
Droperidol
- Reduces postoperative nausea and vomiting
- Do not use this neuraxially
Conopeptides: Snail Poisons
- Ziconotide
- Selectively blocks dorsal horn voltage-gated calcium channels
- Inhibits norepinephrine release, decreasing mean and diastolic pressures
- Approved for treatment of neuropathic pain
- Has a narrow therapeutic window and provokes neuropsychiatric side effects
- Side effects: dizziness, confusion, ataxia, abnormal gait, memory impairment, and suicidal ideation
Baclofen
- GABA-B receptor agonist, suppressing neuronal transmission in the cerebral cortex, basal ganglia, thalamus, cerebellum, and spinal cord
- Actions at laminae II & III:
- Increase potassium conductance, resulting in hyperpolarization
- Inhibit calcium conductance
- Resulting in hyperpolarization and inhibition of glutamate and substance P release
- Intrathecal baclofen is effective in treating pain with multiple sclerosis, complex regional pain syndrome type I, and low back pain
Ketorolac
- Cyclo-oxygenase inhibitor
- COX1 and COX2 facilitate production of prostaglandins leading to hyperalgesia and allodynia after injury
- Intrathecal ketorolac appears to have little analgesia benefit
Magnesium Sulfate
- Acts on NMDA receptors by regulating calcium influx into cells
- Magnesium is the natural antagonist to calcium
- Has some analgesic effect when administered intrathecally or in the epidural space
- Animal studies have reported neurotoxicity, and human safety is not proven
COX Enzymes and NSAIDs
- COX1 is inhibited by aspirin and NSAIDs, while COX2 specific inhibitors have no effect on COX1.
- COX1 maintains normal renal function, provides mucosal protection of the GI tract, and produces thromboxane A2 following platelet activation.
- COX2 mediates pain, inflammation, and fever, and may also modulate nociception centrally.
NSAIDs Side Effects
- NSAIDs are associated with ulcers, perforation, and bleeding, particularly at high doses, in older adults, and with certain comorbidities.
- COX2 specific inhibitors carry less risk of GI side effects.
- NSAIDs are also associated with increased risk of adverse cardiovascular events due to an imbalance between COX2 mediated thromboxane production and antiaggregatory prostaglandin I2 production in endothelial cells.
- Risks may be substantially lower with naproxen.
Other NSAIDs Risks
- NSAIDs may decrease excretion of sodium, increase risk of interstitial nephritis, alter filtration rate and tubular transport, and induce reversible impairment of GFR.
- Risk factors for renal impairment include diabetes, hypertension, atherosclerosis, hypovolemia, salt depletion, and hypoalbuminemia.
- In the liver, aspirin/NSAID use is associated with a decreased risk of hepatocellular carcinoma and death due to chronic liver disease.
Peripheral Analgesics
- Peripheral analgesics have their site of action within damaged tissues, acting at the sensory level to block transmission of pain impulses to higher cortical structures.
- Activators of primary sensory neurons include prostanoids, bradykinin, adenosine triphosphate, histamine, serotonin, and others.
- Nociceptors have their cell bodies in the DRG and synapse with second-order neurons in the dorsal horn.
Anti-Inflammatory Drugs
- NSAIDs block the biosynthesis of prostaglandins from arachidonic acid by binding to the COX enzyme active site.
- COX1 and COX2 are both inhibited, with COX2 inhibition modulating nociception centrally.
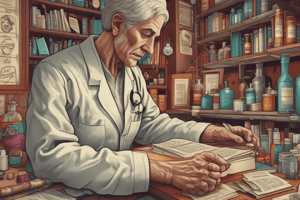
Kinetics and Pharmacology of NSAIDs
- NSAIDs are rapidly absorbed from the GI tract, 90% bound to albumin, and metabolized in the liver and eliminated in urine and bile.
- Hypoalbuminemia increases the fraction of unbound drug and risk of adverse events.
- Impaired renal function prolongs NSAID half-life, and moderate to severe liver disease impairs NSAID metabolism, increasing the potential for toxicity.
Platelet Function and Pulmonary Effects
- Platelet COX1 catalyzes thromboxane A2 production.
- NSAIDs inhibit prostaglandin synthesis, increasing the risk of anaphylaxis, particularly in patients with allergic rhinitis, nasal polyposis, and/or history of asthma.
Hypersensitivity and Allergic Reactions
- NSAIDs can cause bronchoconstriction, rhinitis, urticaria, idiosyncratic adverse events, skin rash, photosensitivity, aseptic meningitis, tinnitus, and hearing loss.
- Drug-drug interactions can occur, including additive inhibition of platelet aggregation, decreased lithium clearance, decreased digoxin clearance, and displacement of phenytoin and valproic acid from their binding sites.
Acetaminophen
- Acetaminophen has antipyretic and analgesic effects, but little anti-inflammatory effects.
- Central analgesic effect is mediated through activation of descending serotonergic pathways.
- At the spinal cord level, acetaminophen antagonizes neurotransmission by NMDA, substance P, and nitric oxide pathways.
- IV formulation (Ofirmev) is currently available, but acetaminophen is the leading cause of acute liver failure in the U.S.
Aspirin
- Aspirin blocks the action of COX enzymes and prevents the production of prostaglandins.
- Aspirin inactivation is irreversible and inhibits platelet aggregation.
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.
Related Documents
Description
Explore alternative analgesia modalities to opioids for managing non-cancer chronic pain. Non-narcotic medications relieve pain without opioid receptors, reducing respiratory depression, physical dependence, and abuse.