Podcast
Questions and Answers
What is the defining characteristic of irreversible cell injury?
What is the defining characteristic of irreversible cell injury?
- The cell undergoes reversible changes.
- The cell can recover with intervention.
- The cell increases its metabolic activity.
- The cell reaches a point where it cannot recover and dies. (correct)
Which of the following is characterized by programmed single cell death?
Which of the following is characterized by programmed single cell death?
- Apoptosis (correct)
- Metaplasia
- Oncosis
- Necrosis
Which of the following best describes necrosis?
Which of the following best describes necrosis?
- Reversible cellular injury
- Cellular adaptation to stress
- A programmed process of single-cell death
- Death of a group of cells within the living body (correct)
What is the primary initiator of necrosis at the cellular level?
What is the primary initiator of necrosis at the cellular level?
What is the role of mitochondria in the pathogenesis of necrosis?
What is the role of mitochondria in the pathogenesis of necrosis?
How does decreased ATP impact cellular function during necrosis?
How does decreased ATP impact cellular function during necrosis?
What role do calcium ions play in the pathogenesis of necrosis?
What role do calcium ions play in the pathogenesis of necrosis?
Reactive oxygen species (ROS) contribute to necrosis by primarily doing what?
Reactive oxygen species (ROS) contribute to necrosis by primarily doing what?
What is a typical microscopic finding in necrotic cells?
What is a typical microscopic finding in necrotic cells?
What is pyknosis a sign of?
What is pyknosis a sign of?
What occurs during karyorrhexis?
What occurs during karyorrhexis?
Which of the following best describes karyolysis?
Which of the following best describes karyolysis?
Which type of necrosis is characterized by the preservation of cell outlines and is commonly seen in infarcts?
Which type of necrosis is characterized by the preservation of cell outlines and is commonly seen in infarcts?
What is the primary process underlying coagulative necrosis?
What is the primary process underlying coagulative necrosis?
What type of necrosis is characterized by complete enzymatic digestion of dead cells, resulting in a liquid mass?
What type of necrosis is characterized by complete enzymatic digestion of dead cells, resulting in a liquid mass?
Brain infarcts typically undergo which type of necrosis?
Brain infarcts typically undergo which type of necrosis?
Which type of necrosis is often associated with tuberculosis?
Which type of necrosis is often associated with tuberculosis?
What is the characteristic appearance of tissue undergoing caseation necrosis?
What is the characteristic appearance of tissue undergoing caseation necrosis?
In what condition is enzymatic fat necrosis most commonly observed?
In what condition is enzymatic fat necrosis most commonly observed?
Which feature distinguishes fibrinoid necrosis from other types of necrosis?
Which feature distinguishes fibrinoid necrosis from other types of necrosis?
Histologically, fibrinoid necrosis is characterized by what?
Histologically, fibrinoid necrosis is characterized by what?
What determines the fate of necrotic tissue?
What determines the fate of necrotic tissue?
How does a small area of necrosis typically resolve?
How does a small area of necrosis typically resolve?
What typically happens to a large area of necrotic tissue?
What typically happens to a large area of necrotic tissue?
What is the fundamental process in apoptosis?
What is the fundamental process in apoptosis?
Which processes are related to physiological apoptosis?
Which processes are related to physiological apoptosis?
Which of the following is a cause of pathologic apoptosis?
Which of the following is a cause of pathologic apoptosis?
Which of the following genes inhibits apoptosis?
Which of the following genes inhibits apoptosis?
What is the role of caspases in apoptosis?
What is the role of caspases in apoptosis?
What is the main morphological hallmark of apoptosis?
What is the main morphological hallmark of apoptosis?
What is the fate of apoptotic bodies?
What is the fate of apoptotic bodies?
What is a key feature that distinguishes apoptosis from necrosis?
What is a key feature that distinguishes apoptosis from necrosis?
Which cellular process involves genetic activation?
Which cellular process involves genetic activation?
Which process is always pathological?
Which process is always pathological?
In the context of cellular injury, describe the sequence of events that leads from a normal cell to necrosis or apoptosis, considering the roles of stress, adaptation, and the severity of injury.
In the context of cellular injury, describe the sequence of events that leads from a normal cell to necrosis or apoptosis, considering the roles of stress, adaptation, and the severity of injury.
Which of the necrosis types would most likely be associated with a well-developed infarct of the brain related to a stroke?
Which of the necrosis types would most likely be associated with a well-developed infarct of the brain related to a stroke?
Imagine a scenario: A researcher is studying a tissue sample under a microscope and observes cells with shrunken nuclei, fragmented DNA, and intact cell membranes. Which of the following processes is most likely occurring in these cells?
Imagine a scenario: A researcher is studying a tissue sample under a microscope and observes cells with shrunken nuclei, fragmented DNA, and intact cell membranes. Which of the following processes is most likely occurring in these cells?
A researcher is investigating a novel therapeutic agent designed to prevent neuronal cell death after a traumatic brain injury. Which of the following mechanisms of action would be most promising for this agent?
A researcher is investigating a novel therapeutic agent designed to prevent neuronal cell death after a traumatic brain injury. Which of the following mechanisms of action would be most promising for this agent?
Consider a scenario where a drug overdose leads to widespread hepatocellular (liver cell) damage, resulting in the release of intracellular contents and a significant inflammatory response. Simultaneously, in the thymus (an immune organ), T-cells that recognize self-antigens are being eliminated without provoking inflammation. Which cell death processes are occurring in each scenario respectively, and what is the key differentiating factor?
Consider a scenario where a drug overdose leads to widespread hepatocellular (liver cell) damage, resulting in the release of intracellular contents and a significant inflammatory response. Simultaneously, in the thymus (an immune organ), T-cells that recognize self-antigens are being eliminated without provoking inflammation. Which cell death processes are occurring in each scenario respectively, and what is the key differentiating factor?
Flashcards
Irreversible Injury
Irreversible Injury
The injury progresses to the point that the cell cannot recover; the cell dies.
Necrosis Definition
Necrosis Definition
Death of a group of cells within the living body. Causes include severe injury or injury of long duration that damages the nucleus and causes cell death.
Apoptosis Definition
Apoptosis Definition
Programmed single cell death.
Mitochondria Damage
Mitochondria Damage
Signup and view all the flashcards
Increased Calcium Ions
Increased Calcium Ions
Signup and view all the flashcards
Necrotic Cells and Inflammation
Necrotic Cells and Inflammation
Signup and view all the flashcards
Cell Membrane Changes in Necrosis
Cell Membrane Changes in Necrosis
Signup and view all the flashcards
Cytoplasm Changes in Necrosis
Cytoplasm Changes in Necrosis
Signup and view all the flashcards
Pyknosis
Pyknosis
Signup and view all the flashcards
Karyorrhexis
Karyorrhexis
Signup and view all the flashcards
Karyolysis
Karyolysis
Signup and view all the flashcards
Coagulative Necrosis
Coagulative Necrosis
Signup and view all the flashcards
Liquefactive Necrosis
Liquefactive Necrosis
Signup and view all the flashcards
Caseation Necrosis
Caseation Necrosis
Signup and view all the flashcards
Fat Necrosis
Fat Necrosis
Signup and view all the flashcards
Fibrinoid Necrosis
Fibrinoid Necrosis
Signup and view all the flashcards
Fate of Necrosis
Fate of Necrosis
Signup and view all the flashcards
Apoptosis Definition
Apoptosis Definition
Signup and view all the flashcards
Physiologic Apoptosis
Physiologic Apoptosis
Signup and view all the flashcards
Pathologic Apoptosis
Pathologic Apoptosis
Signup and view all the flashcards
Apoptosis Pathogenesis
Apoptosis Pathogenesis
Signup and view all the flashcards
Morphology of Apoptosis
Morphology of Apoptosis
Signup and view all the flashcards
Cellular Membranes in Apoptosis
Cellular Membranes in Apoptosis
Signup and view all the flashcards
Small area of necrosis
Small area of necrosis
Signup and view all the flashcards
Large area of necrosis
Large area of necrosis
Signup and view all the flashcards
Study Notes
- Irreversible cell injury leads to cell death, categorized into two main types: necrosis and apoptosis.
Necrosis
- Necrosis means death of a group of cells within a living body.
- Severe injuries or prolonged injuries can damage the nucleus, leading to cell death.
Pathogenesis of Necrosis
- Initial mitochondrial damage decreases ATP, disrupting energy-dependent functions, including the sodium-potassium pump, leading to cell swelling.
- Anaerobic glycolysis also occurs, decreasing pH.
- Increased calcium ions activate enzymes like phospholipases, proteases, endonucleases, and ATPases, damaging proteins, membranes, and DNA.
- Increase in reactive oxygen species (ROS) damage membranes and other cellular components.
Pathology of Necrosis
- Necrotic cells release chemicals that irritate adjacent living tissue, causing an inflammatory reaction.
- Microscopically (M/E), cell membrane disappears, cytoplasm swells and coagulates, appearing homogenous, and deeply eosinophilic, along with nuclear changes: pyknosis, karyorrhexis, & karyolysis.
- Pyknosis means the nucleus shrinks, becomes dense, and deeply basophilic.
- Karyorrhexis means the nucleus becomes fragmented
- Karyolysis means nuclear fragments fade and disappear.
Types of Necrosis
- There are five types of necrosis: coagulative, liquefactive, caseation, fat, and fibrinoid necrosis.
Tissue Changes: Denaturation of Proteins
- Cell outlines are retained, but cellular details are lost, resulting in firm, swollen, pale tissue, characteristic of coagulative necrosis.
Tissue Changes: Enzymatic Digestion
- Lysosomal enzymes from nearby leukocytes cause loss of architectural and structural details, resulting in soft tissue filled with turbid fluid, characteristic of liquefactive necrosis.
Coagulative Necrosis
- Protein denaturation predominates to cause cell damage, while cellular detail is lost, the outline is preserved.
- The necrotic area is dry, firm, opaque, and pale yellow.
- General architecture is preserved, dead cells retain their outline without nuclear or cytoplasmic details, and blood vessels as well as stroma persist longer.
- It's commonly associated with acute ischemia in the heart, kidney, and spleen
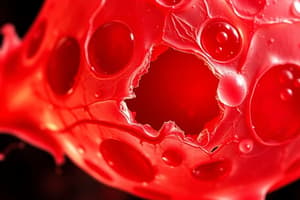
Liquefactive Necrosis
- Enzymatic digestion predominates causing cell damage.
- Necrotic tissue liquefies by enzymes, becoming soft and filled with turbid fluid, with complete loss of architectural and cellular details
- Examples include pyogenic abscesses, where proteolytic enzymes come from neutrophils (pus cells), and brain infarction, which contain high lipid and large fluid contents in nervous tissue.
Caseation Necrosis
- Necrosis appears as a friable, soft, grayish-yellow material resembling cheese.
- Granulomas are formed of homogenous granular eosinophilic material.
- Examples include tuberculosis (TB), syphilis, and fungal infections in any organ.
Fat Necrosis
- Traumatic fat necrosis is when cells rupture because of trauma to adipose tissue in the breast and subcutaneous fat.
- Ruptured cells then release fatty acids combine with calcium
- Enzymatic fat necrosis, which commonly occurs in acute pancreatitis, causes lipase to escape from ruptured pancreatic ducts, digesting surrounding fat
Fibrinoid Necrosis
- It involves histological changes to arteries during vasculitis and hypertension cases.
- Glassy, eosinophilic fibrin-like material is deposited in the damaged necrotic vessel wall
Fate of Necrosis
- The fate of the cells depends on the size of the affected necrotic area: a small area will heal by regeneration or granulation tissue and fibrosis (repair), but a large area will result in being surrounded by a fibrous capsule, where the unabsorbed content dries, and shows dystrophic calcification
Apoptosis
- Apoptosis is a programmed single-cell death where enzymes degrade the cell’s nuclear DNA and cytoplasmic proteins.
Causes of Apoptosis
- Physiologic apoptosis occurs during embryogenesis and hormone-dependent events, such as endometrial breakdown during the menstrual cycle.
- Pathologic apoptosis is often caused by DNA damage and pathologic atrophy.
Pathogenesis of Apoptosis
- A physiological or pathological stimuli initiates the apoptotic process.
- Proapoptotic genes like PAX activate, while anti-apoptotic genes like bcl-2 deactivate.
- Proteases, specifically the caspase family, are activated.
- There are distinct morphological changes that occur
Morphology of Apoptosis
- Electron microscopy (E/M) shows cell shrinkage, chromatin condensation and fragmentation, formation of cytoplasmic blebs and apoptotic bodies, and their phagocytosis by macrophages.
- Light microscopy (L/M) reveals that apoptosis involves single cells or small groups of cells.
- Apoptotic bodies appear rounded or oval with dense eosinophilic cytoplasm and nuclear fragments with no inflammation in the surrounding tissue
Necrosis vs. Apoptosis
- Necrosis involves groups of cells or tissues, but apoptosis involves single cells.
- There is no gene activation involved in necrosis, but there is genetic activation involved in apoptosis.
- ATP decreases in necrosis, but is normal in apoptosis.
- In necrosis, there is swelling of cells, but apoptotic bodies form due to apoptosis.
- Cellular membranes rupture during necrosis, but they remain intact during apoptosis until later on, when apoptotic bodies separate.
- Inflammation occurs around necrosis, but not with apoptosis.
- Necrosis is always pathological, but apoptosis can sometimes be physiological.
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.