Podcast
Questions and Answers
What characterizes dystrophic calcification in tissues?
What characterizes dystrophic calcification in tissues?
- It is predominantly found in healthy tissues with strong blood supply.
- It occurs in the presence of elevated serum calcium levels.
- It arises in dead or dying tissues despite normal calcium metabolism. (correct)
- It is associated with significant functional impairment of affected organs.
Which of the following conditions is NOT a cause of hypercalcemia?
Which of the following conditions is NOT a cause of hypercalcemia?
- Advanced renal failure.
- Milk alkali syndrome.
- Primary hyperparathyroidism.
- Significant weight loss due to dieting. (correct)
Which statement about hypertrophy is true?
Which statement about hypertrophy is true?
- Hypertrophy leads to complete cell death within the tissue.
- Hypertrophy involves the shrinkage of cells and organs.
- It occurs exclusively in response to hormonal changes.
- It results in an increase in cell size due to protein synthesis. (correct)
What is a key characteristic of necrosis compared to apoptosis?
What is a key characteristic of necrosis compared to apoptosis?
What best describes atrophy in cells?
What best describes atrophy in cells?
Which of the following contributes to hypoxic cell injury?
Which of the following contributes to hypoxic cell injury?
Where does metastatic calcification typically occur?
Where does metastatic calcification typically occur?
Which cellular element is primarily affected by oxidative stress?
Which cellular element is primarily affected by oxidative stress?
Which injury factor is least likely to contribute to cell injury?
Which injury factor is least likely to contribute to cell injury?
In cell injury scenarios, which of the following systems is particularly sensitive to disruption?
In cell injury scenarios, which of the following systems is particularly sensitive to disruption?
What distinguishes ischæmia from hypoxia?
What distinguishes ischæmia from hypoxia?
What role does age play in cellular response to injury?
What role does age play in cellular response to injury?
What is the most significant consequence of impaired aerobic respiration in cells?
What is the most significant consequence of impaired aerobic respiration in cells?
Which of the following are examples of cell injury implicated by free radicals?
Which of the following are examples of cell injury implicated by free radicals?
What process primarily generates superoxide radicals inside cells?
What process primarily generates superoxide radicals inside cells?
Which of the following statements about chemical injury is true?
Which of the following statements about chemical injury is true?
How do free radicals primarily affect cellular membranes?
How do free radicals primarily affect cellular membranes?
What is a common consequence of intracellular free radical formation?
What is a common consequence of intracellular free radical formation?
What initial cellular process is affected by hypoxia leading to cell injury?
What initial cellular process is affected by hypoxia leading to cell injury?
Which enzyme is involved in generating superoxide radicals?
Which enzyme is involved in generating superoxide radicals?
Which enzyme's activity is stimulated due to decreased ATP and AMP during hypoxic conditions?
Which enzyme's activity is stimulated due to decreased ATP and AMP during hypoxic conditions?
What effect does carbon tetrachloride (CCl4) have on the liver regarding cell injury?
What effect does carbon tetrachloride (CCl4) have on the liver regarding cell injury?
What cellular change occurs when hypoxia leads to a reduction of the plasma membrane sodium pump?
What cellular change occurs when hypoxia leads to a reduction of the plasma membrane sodium pump?
Which component of the cell is MOST commonly affected by free radical reactions?
Which component of the cell is MOST commonly affected by free radical reactions?
Which of the following is NOT associated with irreversible injury in cells?
Which of the following is NOT associated with irreversible injury in cells?
What immediate cellular change is associated with reversible cell injury?
What immediate cellular change is associated with reversible cell injury?
What is a mechanism contributing to membrane injury during reperfusion of ischaemic tissues?
What is a mechanism contributing to membrane injury during reperfusion of ischaemic tissues?
What role does iron play in free radical formation?
What role does iron play in free radical formation?
Which of the following conditions is most likely to contribute to acute cellular swelling during hypoxia?
Which of the following conditions is most likely to contribute to acute cellular swelling during hypoxia?
What structural feature is often lost in cells experiencing prolonged hypoxia?
What structural feature is often lost in cells experiencing prolonged hypoxia?
Which process primarily leads to the degradation of cytoplasmic components during irreversible injury?
Which process primarily leads to the degradation of cytoplasmic components during irreversible injury?
What does the accumulation of lactic acid during hypoxia indicate?
What does the accumulation of lactic acid during hypoxia indicate?
What role does calcium play in the context of cellular injury and death?
What role does calcium play in the context of cellular injury and death?
What is the primary cause of cytoplasmic eosinophilia?
What is the primary cause of cytoplasmic eosinophilia?
Which necrosis type is characterized by the preservation of structural outlines of coagulated cells?
Which necrosis type is characterized by the preservation of structural outlines of coagulated cells?
Which type of necrosis is specifically associated with tuberculous infection?
Which type of necrosis is specifically associated with tuberculous infection?
What alterations are associated with mitochondrial changes in injury?
What alterations are associated with mitochondrial changes in injury?
What type of necrosis results primarily from hypoxic cell death in the central nervous system?
What type of necrosis results primarily from hypoxic cell death in the central nervous system?
Which of the following processes contributes to the morphologic appearance of necrosis?
Which of the following processes contributes to the morphologic appearance of necrosis?
What is karyorrhexis referring to in nuclear changes during necrosis?
What is karyorrhexis referring to in nuclear changes during necrosis?
Which cellular changes are indicative of necrosis?
Which cellular changes are indicative of necrosis?
What is the term for the process of cell digestion derived from dead cells?
What is the term for the process of cell digestion derived from dead cells?
Which of the following best describes gangrenous necrosis?
Which of the following best describes gangrenous necrosis?
Flashcards are hidden until you start studying
Study Notes
Cell Injury
- Cells maintain a narrow range of physiological activities, but can adapt to stress
- When adaptive capacity is exceeded, cell injury occurs
- Two main cell death patterns:
- Necrosis: Occurs due to noxious conditions, characterized by swelling, protein denaturation, and organellar breakdown
- Apoptosis: Programmed cell death occurring in normal or physiologic conditions
Causes of Cell Injury
- Hypoxia: Reduced oxygen supply to cells, impacting aerobic respiration (distinct from ischemia, which also causes hypoxic injury)
- Physical Agents: Trauma, extreme temperatures, radiation, electric shock, pressure changes
- Chemicals and Drugs: Alter membrane permeability, osmotic balance, or enzyme integrity
- Microbiologic Agents: Viruses, bacteria, parasites
- Immunologic Reactions: Immune system responses can cause cell injury (e.g., anaphylaxis)
- Genetic Defects: Inherited genetic disorders (e.g., Down Syndrome, sickle cell anemia)
- Nutritional Imbalances: Protein-calorie deficiency, vitamin deficiencies, diets high in animal fat can contribute to cell injury
Mechanisms of Cell Injury
- Cell response to injury depends on type, duration, and severity
- Four key intracellular systems vulnerable to injury:
- Cell membrane integrity
- Aerobic respiration
- Protein synthesis
- The genetic apparatus
- Calcium Imbalance:
- Cytosolic calcium normally kept low by ATP-dependent transporters
- Ischemia or toxins increase calcium influx and release from mitochondria
- Activated enzymes (phospholipases, proteases, ATPases, endonucleases) damage cell structures
- Free Radicals:
- Important mediators of cell death
- Unstable chemical species with unpaired electrons
- Generated during normal metabolism, radiation, chemical exposure
- Damage cell components (lipid peroxidation of membranes, DNA damage, protein cross-linking)
Ischemic and Hypoxic Injury
- Reversible Injury:
- Initial effect of hypoxia is reduced ATP production
- Results in sodium and water influx, potassium efflux, cell swelling
- Increased anaerobic glycolysis, glycogen depletion, lactic acid buildup
- Reduced protein synthesis, cytoskeletal damage
- Irreversible Injury:
- Severe mitochondrial damage, calcium accumulation
- Extensive plasma membrane damage, lysosomal swelling
- Reperfusion can worsen injury (calcium-mediated)
- Loss of proteins, coenzymes, RNA
- Lysosomal enzymes degrade cell components
Mechanisms of Irreversible Injury
- Progressive loss of membrane phospholipids
- Cytoskeletal abnormalities (protease activation, calcium increase)
- Toxic oxygen radicals generated during reperfusion
- Lipid breakdown products with detergent effects
Chemical Injury
- Two main mechanisms:
- Direct combination with cellular components (e.g., mercury binding to sulfhydryl groups)
- Conversion to reactive metabolites (e.g., CCl4 converted to CCl3. in the liver, causing lipid peroxidation)
Patterns of Acute Cell Injury
- Reversible Cell Injury:
- Light microscopic changes: cell swelling, cytoplasmic eosinophilia, fatty change
- Ultrastructural changes: membrane blebbing, mitochondrial swelling, ER dilatation, nuclear changes
- Necrosis:
- Morphologic changes after cell death in living tissue
- Enzymatic digestion of cell and protein denaturation
- Cytoplasmic changes: eosinophilia, vacuolation, calcification
- Nuclear changes: karyolysis, pyknosis, karyorrhexis
Types of Necrosis
- Coagulative Necrosis: Preservation of structural outlines (common in myocardial infarction)
- Liquefactive Necrosis: Enzymatic digestion, liquefied tissue (bacterial infections, CNS hypoxia)
- Gangrenous Necrosis: Ischemic coagulative necrosis with superimposed infection
- Caseous Necrosis: Cheese-like appearance, characteristic of tuberculosis
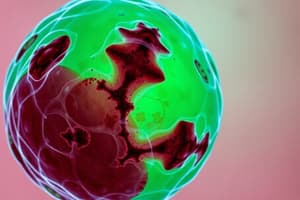
Calcification
- Dystrophic Calcification: Deposition in dead or dying tissue (atherosclerosis, aging)
- Metastatic Calcification: Deposition in normal tissue due to hypercalcemia (hyperparathyroidism, tumor-related, vitamin D toxicity, renal failure)
Cellular Adaptations of Growth and Differentiation
- Atrophy: Reduction in cell size due to decreased work load, blood supply, innervation, nutrition, hormonal stimulation, or aging
- Hypertrophy: Increase in cell size due to increased synthesis of proteins and organelles (increased workload)
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.