Podcast
Questions and Answers
Which of the following correctly describes cellular adaptations?
Which of the following correctly describes cellular adaptations?
- Adaptations are irreversible changes that lead to cell death.
- Adaptations involve alterations that allow the cell to survive under stress. (correct)
- Adaptations are permanent structural changes with no functional benefits.
- Adaptations only occur in pathological conditions.
Which of the following is NOT a cause of cell injury?
Which of the following is NOT a cause of cell injury?
- Increased exercise (correct)
- Genetic abnormalities
- Oxygen deprivation
- Chemical agents and drugs
What is the primary effect of ischemia on cells?
What is the primary effect of ischemia on cells?
- It provides excess oxygen to the cells.
- It leads to a loss of blood supply and therefore oxygen. (correct)
- It reduces cellular waste products immediately.
- It enhances cellular metabolic activity.
Which factor can lead to hypoxia?
Which factor can lead to hypoxia?
Which of the following substances could act as a chemical agent leading to cell injury?
Which of the following substances could act as a chemical agent leading to cell injury?
Which of the following describes the role of immunologic reactions in cell injury?
Which of the following describes the role of immunologic reactions in cell injury?
What is a common result of nutritional imbalances in cellular health?
What is a common result of nutritional imbalances in cellular health?
What is the impact of aging on cellular health?
What is the impact of aging on cellular health?
What appearance does pus typically have due to acute inflammation?
What appearance does pus typically have due to acute inflammation?
What is the characteristic appearance of the necrotic focus in caseous necrosis?
What is the characteristic appearance of the necrotic focus in caseous necrosis?
In what type of infection is caseous necrosis most commonly encountered?
In what type of infection is caseous necrosis most commonly encountered?
What happens to the normal tissue architecture in the event of a renal abscess?
What happens to the normal tissue architecture in the event of a renal abscess?
Which type of necrosis results from acute ischemia or severe bacterial infection?
Which type of necrosis results from acute ischemia or severe bacterial infection?
What is the gross appearance of tissue in caseous necrosis often described as?
What is the gross appearance of tissue in caseous necrosis often described as?
What happens to the tissue as a result of gangrene that leads to a foul smell?
What happens to the tissue as a result of gangrene that leads to a foul smell?
Gangrene is a modified form of which type of necrosis?
Gangrene is a modified form of which type of necrosis?
What defines hyperplasia?
What defines hyperplasia?
Under which conditions does hyperplasia typically cease after tissue restoration?
Under which conditions does hyperplasia typically cease after tissue restoration?
What type of hyperplasia is exemplified by the proliferation of glandular epithelium in the female breast at puberty?
What type of hyperplasia is exemplified by the proliferation of glandular epithelium in the female breast at puberty?
Which of the following best describes endometrial hyperplasia?
Which of the following best describes endometrial hyperplasia?
What distinguishes pathologic hyperplasia from physiologic hyperplasia?
What distinguishes pathologic hyperplasia from physiologic hyperplasia?
What initiates compensatory hyperplasia in the liver?
What initiates compensatory hyperplasia in the liver?
Which factor is primarily responsible for turning off cell proliferation after liver restoration?
Which factor is primarily responsible for turning off cell proliferation after liver restoration?
How long can hyperplasia persist after the removal of the stimulus?
How long can hyperplasia persist after the removal of the stimulus?
What is the role of the bax gene in apoptosis?
What is the role of the bax gene in apoptosis?
Which physiologic condition does NOT involve evident apoptosis?
Which physiologic condition does NOT involve evident apoptosis?
Which of the following is an apoptosis-inhibiting gene?
Which of the following is an apoptosis-inhibiting gene?
What is a potential effect of excessive accumulation of misfolded proteins in cells?
What is a potential effect of excessive accumulation of misfolded proteins in cells?
Which situation involves cell death induced by cytotoxic T lymphocytes?
Which situation involves cell death induced by cytotoxic T lymphocytes?
Which of the following is considered a pathologic condition with evident apoptosis?
Which of the following is considered a pathologic condition with evident apoptosis?
What trigger can lead to apoptotic cell death due to DNA damage?
What trigger can lead to apoptotic cell death due to DNA damage?
What is the primary function of the death-inducing signaling complex in apoptosis?
What is the primary function of the death-inducing signaling complex in apoptosis?
What is the primary difference between dystrophic calcification and metastatic calcification?
What is the primary difference between dystrophic calcification and metastatic calcification?
Which condition is not typically associated with dystrophic calcification?
Which condition is not typically associated with dystrophic calcification?
What characterizes metastatic calcification in tissues?
What characterizes metastatic calcification in tissues?
Which of the following is a consequence of renal failure related to metastatic calcification?
Which of the following is a consequence of renal failure related to metastatic calcification?
Which of the following is a typical example of dystrophic calcification?
Which of the following is a typical example of dystrophic calcification?
Which condition is likely to cause accelerated bone turnover associated with metastatic calcification?
Which condition is likely to cause accelerated bone turnover associated with metastatic calcification?
What is the role of vitamin D in metastatic calcification?
What is the role of vitamin D in metastatic calcification?
Which of the following is not a cause of metastatic calcification?
Which of the following is not a cause of metastatic calcification?
Flashcards are hidden until you start studying
Study Notes
Overview of Cellular Responses to Stress and Noxious Stimuli
- Adaptations in cells are reversible changes to structural and functional states due to physiological or pathological stimuli, enabling survival and continued function.
Causes of Cell Injury
- Oxygen deprivation includes hypoxia due to ischemia (loss of blood supply) and anemia (decreased hemoglobin).
- Physical agents causing injury include mechanical trauma, temperature extremes (burns/freezing), and radiation or electrical shock.
- Chemical agents encompass poisons (e.g., arsenic, cyanide), hypertonic solutions (glucose/salts), environmental pollutants, alcohol, and narcotic drugs.
- Infectious agents include viruses, bacteria, fungi, and parasites.
- Immunologic reactions involve the immune system causing cell injury, such as in autoimmune diseases and anaphylactic reactions.
- Genetic abnormalities can lead to pathologies, evident in conditions like Down syndrome or sickle cell anemia.
- Nutritional imbalances include protein-calorie deficiencies, vitamin insufficiencies, and excessive lipids leading to atherosclerosis.
- Aging results in cellular senescence, impacting replication and repair capabilities.
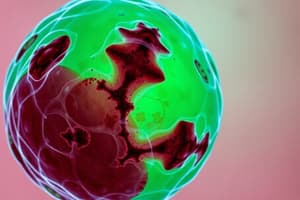
Types of Cell Death
- Necrosis is uncontrolled cell death due to factors like hypoxia, physical agents, or toxic substances.
- Liquefactive necrosis occurs in the brain, forming cavities due to tissue liquefaction.
- Caseous necrosis characterizes tuberculosis infections, presenting as cheesy, necrotic tissue.
- Gangrenous necrosis involves large-scale tissue death due to ischemia or infection, often leading to putrefaction and foul odors.
Apoptosis
- Apoptosis is programmed cell death, crucial for normal development and maintenance of tissue homeostasis.
- Genes involved include pro-apoptotic genes (e.g., bax) that stimulate apoptosis and anti-apoptotic genes (e.g., bcl) that inhibit it.
Physiologic and Pathologic Conditions of Apoptosis
- Physiologic apoptosis occurs during embryogenesis, hormone-driven tissue involution, and elimination of unnecessary immune cells.
- Pathologic apoptosis can be triggered by cytotoxic T lymphocytes, DNA damage, accumulation of misfolded proteins, and viral infections leading to cell loss.
Hypertrophy and Hyperplasia
- Hypertrophy is an increase in cell size due to increased functional demand or stimuli.
- Hyperplasia involves an increase in cell number, contributing to tissue or organ enlargement.
- Physiologic hyperplasia includes hormonal (e.g., breast tissue during pregnancy) and compensatory types (e.g., liver regeneration post-resection).
- Pathologic hyperplasia denotes excessive proliferation, like endometrial hyperplasia due to estrogen imbalance.
Calcification Types
- Dystrophic calcification involves calcium deposits in dead or dying tissue without abnormal calcium metabolism; often seen in necrotic tissues and certain tumors.
- Metastatic calcification occurs in living tissues due to hypercalcemia, linked to conditions such as primary or metastatic bone tumors, renal failure, and increased parathyroid hormone secretion.
Key Terms
- Psammoma Bodies are dystrophic calcified deposits found in certain malignant tumors, indicating a specific type of calcification associated with cancerous growths.
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.