Podcast
Questions and Answers
What is the connective tissue layer that surrounds cartilage called?
What is the connective tissue layer that surrounds cartilage called?
- Capsular matrix
- Perichondrium (correct)
- Interterritorial matrix
- Territorial matrix
What are the clusters of chondrocytes that originate from a single progenitor cell called?
What are the clusters of chondrocytes that originate from a single progenitor cell called?
- Differentiating groups
- Isogenous clusters (correct)
- Territorial groups
- Interterritorial clusters
Which of the following best describes the immediate matrix surrounding individual chondrocytes?
Which of the following best describes the immediate matrix surrounding individual chondrocytes?
- Perichondrium
- Interterritorial matrix
- Capsular matrix
- Territorial matrix (correct)
What is the term for the color variation seen in cartilage matrix, ranging from blue to purple when stained?
What is the term for the color variation seen in cartilage matrix, ranging from blue to purple when stained?
Which component of the cartilage matrix lies between the cell clusters?
Which component of the cartilage matrix lies between the cell clusters?
Which type of collagen is predominantly produced by chondrocytes in fibrocartilage?
Which type of collagen is predominantly produced by chondrocytes in fibrocartilage?
In fibrocartilage, where are the fibroblasts primarily located?
In fibrocartilage, where are the fibroblasts primarily located?
What is a characteristic feature of fibrocartilage compared to other types of cartilage regarding its outer covering?
What is a characteristic feature of fibrocartilage compared to other types of cartilage regarding its outer covering?
Which transcription factor plays a crucial role in the differentiation of chondrogenic nodule cells into chondroblasts during chondrogenesis?
Which transcription factor plays a crucial role in the differentiation of chondrogenic nodule cells into chondroblasts during chondrogenesis?
Which of the following is NOT a typical location where fibrocartilage is found?
Which of the following is NOT a typical location where fibrocartilage is found?
Which of the following is NOT a primary component of cartilage?
Which of the following is NOT a primary component of cartilage?
What is the major contributing factor for the resilience of cartilage?
What is the major contributing factor for the resilience of cartilage?
Which of the following describes the primary function of the perichondrium?
Which of the following describes the primary function of the perichondrium?
Which substance in the extracellular matrix is mostly responsible for cartilage's ability to withstand compression?
Which substance in the extracellular matrix is mostly responsible for cartilage's ability to withstand compression?
How does cartilage receive its nutrients since it’s avascular?
How does cartilage receive its nutrients since it’s avascular?
Which term describes groups of chondrocytes within a single lacuna?
Which term describes groups of chondrocytes within a single lacuna?
What is the main role of the chondroblast?
What is the main role of the chondroblast?
What is the primary function of collagen fibers within the cartilage matrix?
What is the primary function of collagen fibers within the cartilage matrix?
Which of the following is a primary function of multiadhesive glycoproteins within hyaline cartilage?
Which of the following is a primary function of multiadhesive glycoproteins within hyaline cartilage?
What role does Type II collagen play in the extracellular matrix of hyaline cartilage?
What role does Type II collagen play in the extracellular matrix of hyaline cartilage?
What is the primary function of aggrecans in the hyaline cartilage extracellular matrix?
What is the primary function of aggrecans in the hyaline cartilage extracellular matrix?
What does the term 'basophilia' refer to in the context of hyaline cartilage?
What does the term 'basophilia' refer to in the context of hyaline cartilage?
Which component of the hyaline cartilage extracellular matrix has a significant role in resisting swelling pressure?
Which component of the hyaline cartilage extracellular matrix has a significant role in resisting swelling pressure?
What is a consequence of the calcification of the hyaline cartilage extracellular matrix?
What is a consequence of the calcification of the hyaline cartilage extracellular matrix?
Which of the following is true about the hydrated extracellular matrix in hyaline cartilage?
Which of the following is true about the hydrated extracellular matrix in hyaline cartilage?
What is the function of Anchorin CII?
What is the function of Anchorin CII?
Which of the following best describes where appositional growth occurs in cartilage?
Which of the following best describes where appositional growth occurs in cartilage?
Where does interstitial growth of cartilage primarily occur?
Where does interstitial growth of cartilage primarily occur?
Why does cartilage have a limited ability to repair itself?
Why does cartilage have a limited ability to repair itself?
What complication can arise during cartilage repair in adults?
What complication can arise during cartilage repair in adults?
Which of the following is NOT a common situation where hyaline cartilage calcification occurs?
Which of the following is NOT a common situation where hyaline cartilage calcification occurs?
What consequence occurs when cartilage matrix becomes calcified?
What consequence occurs when cartilage matrix becomes calcified?
Which cell type is primarily responsible for removing calcified cartilage matrix?
Which cell type is primarily responsible for removing calcified cartilage matrix?
What happens to the calcified cartilage after chondrocyte cell death?
What happens to the calcified cartilage after chondrocyte cell death?
Which type of cartilage is characterized by a dense network of branching elastic fibers within its matrix?
Which type of cartilage is characterized by a dense network of branching elastic fibers within its matrix?
What is the primary function of the perichondrium in growing cartilage?
What is the primary function of the perichondrium in growing cartilage?
Which type of cartilage lacks a perichondrium?
Which type of cartilage lacks a perichondrium?
What is the predominant type of collagen found in hyaline cartilage?
What is the predominant type of collagen found in hyaline cartilage?
Which of the following is a characteristic of fibrocartilage?
Which of the following is a characteristic of fibrocartilage?
During osteoarthritis, an increase in which enzyme activity contributes to cartilage matrix breakdown?
During osteoarthritis, an increase in which enzyme activity contributes to cartilage matrix breakdown?
Which of the following structures contains hyaline cartilage?
Which of the following structures contains hyaline cartilage?
What are the two layers of the perichondrium in growing cartilage?
What are the two layers of the perichondrium in growing cartilage?
In electron microscopy, what are some notable features of chondrocytes?
In electron microscopy, what are some notable features of chondrocytes?
What is the function of multiadhesive glycoproteins secreted by chondrocytes?
What is the function of multiadhesive glycoproteins secreted by chondrocytes?
Flashcards
Perichondrium
Perichondrium
A layer of connective tissue surrounding cartilage, containing cells that can differentiate into chondroblasts.
Differentiating chondroblasts
Differentiating chondroblasts
Immature chondrocytes actively producing and secreting cartilage matrix.
Chondrocytes
Chondrocytes
Mature cartilage cells that reside in spaces called lacunae within the cartilage matrix.
Isogenic clusters
Isogenic clusters
Signup and view all the flashcards
Territorial matrix
Territorial matrix
Signup and view all the flashcards
What is Fibrocartilage?
What is Fibrocartilage?
Signup and view all the flashcards
Where is Fibrocartilage found?
Where is Fibrocartilage found?
Signup and view all the flashcards
Does Fibrocartilage have a perichondrium?
Does Fibrocartilage have a perichondrium?
Signup and view all the flashcards
What are Chondrocytes?
What are Chondrocytes?
Signup and view all the flashcards
What are Fibroblasts?
What are Fibroblasts?
Signup and view all the flashcards
Appositional Growth of Cartilage
Appositional Growth of Cartilage
Signup and view all the flashcards
Interstitial Growth of Cartilage
Interstitial Growth of Cartilage
Signup and view all the flashcards
Cartilage Repair
Cartilage Repair
Signup and view all the flashcards
Hyaline Cartilage Calcification
Hyaline Cartilage Calcification
Signup and view all the flashcards
When Does Hyaline Cartilage Calcify?
When Does Hyaline Cartilage Calcify?
Signup and view all the flashcards
What Happens When Cartilage Calcifies?
What Happens When Cartilage Calcifies?
Signup and view all the flashcards
Chondroclasts
Chondroclasts
Signup and view all the flashcards
Hyaline Cartilage Aging
Hyaline Cartilage Aging
Signup and view all the flashcards
What is Perichondrium?
What is Perichondrium?
Signup and view all the flashcards
What is the chondrogenic layer?
What is the chondrogenic layer?
Signup and view all the flashcards
What is the fibrous layer?
What is the fibrous layer?
Signup and view all the flashcards
What is articular cartilage?
What is articular cartilage?
Signup and view all the flashcards
What is osteoarthritis?
What is osteoarthritis?
Signup and view all the flashcards
What is elastic cartilage?
What is elastic cartilage?
Signup and view all the flashcards
What is the epiphyseal plate?
What is the epiphyseal plate?
Signup and view all the flashcards
What is hyaline cartilage?
What is hyaline cartilage?
Signup and view all the flashcards
Hyaline Cartilage Extracellular Matrix Components
Hyaline Cartilage Extracellular Matrix Components
Signup and view all the flashcards
What is cartilage?
What is cartilage?
Signup and view all the flashcards
Multiadhesive Glycoproteins in Hyaline Cartilage
Multiadhesive Glycoproteins in Hyaline Cartilage
Signup and view all the flashcards
Anchorin CII Function
Anchorin CII Function
Signup and view all the flashcards
Why is cartilage avascular?
Why is cartilage avascular?
Signup and view all the flashcards
Type II Collagen Function in Hyaline Cartilage
Type II Collagen Function in Hyaline Cartilage
Signup and view all the flashcards
What makes cartilage resilient?
What makes cartilage resilient?
Signup and view all the flashcards
Aggrecans and Hydration in Hyaline Cartilage
Aggrecans and Hydration in Hyaline Cartilage
Signup and view all the flashcards
What are the components of the ECM?
What are the components of the ECM?
Signup and view all the flashcards
Explain proteoglycan aggregates.
Explain proteoglycan aggregates.
Signup and view all the flashcards
Basophilia in Hyaline Cartilage
Basophilia in Hyaline Cartilage
Signup and view all the flashcards
Metachromasia in Hyaline Cartilage
Metachromasia in Hyaline Cartilage
Signup and view all the flashcards
What are chondroblasts and chondrocytes?
What are chondroblasts and chondrocytes?
Signup and view all the flashcards
Describe hyaline cartilage.
Describe hyaline cartilage.
Signup and view all the flashcards
Calcification of Hyaline Cartilage
Calcification of Hyaline Cartilage
Signup and view all the flashcards
Study Notes
Cartilage Overview
- Cartilage is a specialized connective tissue, providing a combination of resilience, rigidity, and elasticity
- It's a key component in fetal skeleton development and growing bones
- Cartilage matrix is primarily composed of chondrocytes (cells) and an extracellular matrix (95%)
- The extracellular matrix gives cartilage its resilience due to its composition
Cartilage - General Facts
- Cartilage is avascular; relying on diffusion for nutrient acquisition
- The composition of the extracellular matrix (ECM) is critical for chondrocyte survival
- The ECM consists of fibers (mostly collagen) and ground substance (glycosaminoglycans in the form of proteoglycan aggregates)
Proteoglycan Aggregates
- Proteoglycans are made of glycosaminoglycans (GAGs) linked to a core protein
- Proteoglycan aggregates consist of several proteoglycans, facilitating diffusion of nutrients from blood vessels to chondrocytes
Classification of Cartilage
- There are three main types of cartilage: hyaline, elastic, and fibrocartilage, each with distinct characteristics in their extracellular matrix
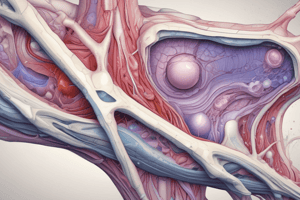
Hyaline Cartilage
- Hyaline cartilage appears glassy in the living state
- Distinguished by a smooth, amorphous extracellular matrix
- Spaces within the matrix are called lacunae, which house chondrocytes that produce the ECM
- Contains type II collagen, proteoglycans (e.g., aggrecan), and multiadhesive glycoproteins
- Found in the nasal septum, larynx, trachea, costal cartilage, articular cartilage of joints, and the epiphyseal plate
Elastic Cartilage
- Distinguished by the presence of elastin fibers
- Contains a dense network of branching and anastomosing elastic fibers and sheets
- Provides elasticity, and found in the epiglottis, external ear, and parts of the auditory tube
Fibrocartilage
- A combination of dense regular connective tissue and hyaline cartilage
- Chondrocytes are dispersed amongst collagen fibers, arranged singly or in rows / isogenic groups
- Contains type I collagen, proteoglycans, and multiadhesive glycoproteins
- Found in the annulus fibrosus of intervertebral discs, symphysis pubis, menisci of the knee joint, articular discs of TMJ, and the triangular fibrocartilage complex
Chondrocytes
- Chondrocytes are located within spaces called lacunae
- Their appearance (cytoplasm) varies depending on their level of activity in matrix production
- Active chondrocytes typically display a basophilic cytoplasm related to protein synthesis and visible Golgi bodies
- Less active chondrocytes contain glycogen stores and lipid droplets
Extracellular Matrix of Hyaline Cartilage
- Hyaline cartilage ECM contains three major components: collagen, proteoglycans, and multiadhesive glycoproteins
- Collagen, primarily type II, provides tensile strength and shape
- Proteoglycans, especially aggrecans, bind water and contribute to resilience and the resistance of swelling pressure
- Multiadhesive glycoproteins influence the interaction of chondrocytes with the matrix
Regions of Extracellular Matrix
- The extracellular matrix exhibits three characteristic regions within: capsular (pericellular), territorial, and interterritorial
- The capsular region is adjacent to the chondrocyte, with a high proteoglycan concentration
- The territorial area surrounds the isogenous groups, with lower proteoglycan concentration than the capsular area
- The interterritorial region is between isogenous groups, containing the fewest proteoglycans
Chondrogenesis
- Chondrogenesis is the process of cartilage formation originating from mesenchymal cells or ectomesenchyme, which differentiate into isogenous cell clusters.
Cartilage Growth
- Two types: appositional and interstitial
- Appositional growth occurs on the surface of existing cartilage through differentiation and secretion of cartilage matrix by chondroblasts from the inner cellular layer of the perichondrium.
- Interstitial growth occurs within the existing cartilage through the division of chondrocytes within their lacunae, and the secretion of new matrix pushing cells apart.
Cartilage Repair
- Cartilage has a limited ability to repair due to its avascular nature and the limited ability of mature chondrocytes to proliferate.
- New blood vessels at the healing site may stimulate bone formation instead of cartilage repair.
Hyaline Cartilage Calcification
- Calcification is a common process in cartilage, especially in growing bones and as part of the ageing process.
- Calcification involves the deposition of calcium phosphate crystals in the cartilage matrix, impacting nutrient diffusion and potentially causing chondrocyte death
Age Changes of Hyaline Cartilage
- Aging often leads to hyaline cartilage calcification in parts of the tracheal cartilage and other locations within articulating surfaces of joints
- In these situations, bone formation sometimes replaces the calcified cartilage matrix tissue
What Happens When Cartilage is Calcified
- Calcification impairs nutrient diffusion, leading to chondrocyte death
- Dead calcified matrix is removed by phagocytes and replaced by bone tissue, often causing long-term effects like osteoarthritis.
Cartilage Summary
- Summarizes the key aspects of cartilage types, structure, formation and function of the three types of cartilage.
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.