Podcast
Questions and Answers
How would blood viscosity be affected in an individual with polycythemia, and what potential effect could this have on blood flow?
How would blood viscosity be affected in an individual with polycythemia, and what potential effect could this have on blood flow?
- Unchanged viscosity, with no effect on blood flow.
- Increased viscosity, potentially impeding blood flow. (correct)
- Decreased viscosity, potentially increasing blood flow.
- Increased viscosity, potentially increasing blood flow due to heightened pressure.
What physiological response would the body initiate if there's a significant drop in blood oxygen levels, and how does this response help restore homeostasis?
What physiological response would the body initiate if there's a significant drop in blood oxygen levels, and how does this response help restore homeostasis?
- Increased production of anti-A and anti-B antibodies to agglutinate foreign antigens.
- Increased erythropoietin (EPO) production to stimulate red blood cell production. (correct)
- Increased thrombopoietin (TPO) production to increase platelet count.
- Increased leukopenia to fight infection.
A patient with blood type AB is in need of a transfusion. Which blood type(s) can they safely receive, and why?
A patient with blood type AB is in need of a transfusion. Which blood type(s) can they safely receive, and why?
- Only type AB, because they have both A and B antigens.
- Types A, B, AB, or O, because they are a universal recipient and can accept any of these without significant risk of agglutination. (correct)
- Types A, B, or O, because they lack the corresponding antibodies.
- Only type O, because it lacks A and B antigens.
If the mitral valve is stenotic, what effect would this have on blood flow, and where would you expect to see blood accumulating?
If the mitral valve is stenotic, what effect would this have on blood flow, and where would you expect to see blood accumulating?
A cardiologist detects an abnormal heart sound (a murmur) between the 'Lubb' and 'Dupp' sounds. What valve is most likely malfunctioning?
A cardiologist detects an abnormal heart sound (a murmur) between the 'Lubb' and 'Dupp' sounds. What valve is most likely malfunctioning?
Consider an individual experiencing a sudden increase in afterload. What compensatory mechanism would the heart employ to maintain cardiac output, and how does this mechanism achieve this?
Consider an individual experiencing a sudden increase in afterload. What compensatory mechanism would the heart employ to maintain cardiac output, and how does this mechanism achieve this?
How does the autonomic nervous system regulate heart rate, and what specific neurotransmitters are involved in increasing and decreasing heart rate, respectively?
How does the autonomic nervous system regulate heart rate, and what specific neurotransmitters are involved in increasing and decreasing heart rate, respectively?
If a patient is diagnosed with left ventricular failure, what specific clinical sign is most likely to manifest, and how is it directly related to the heart's dysfunction?
If a patient is diagnosed with left ventricular failure, what specific clinical sign is most likely to manifest, and how is it directly related to the heart's dysfunction?
How do veins counteract the effects of gravity to ensure blood returns efficiently to the heart, especially in the lower extremities?
How do veins counteract the effects of gravity to ensure blood returns efficiently to the heart, especially in the lower extremities?
What effect does vasoconstriction have on vascular resistance, and how does this affect blood pressure?
What effect does vasoconstriction have on vascular resistance, and how does this affect blood pressure?
In a patient experiencing hypovolemic shock, what is the primary underlying issue, and how does it lead to inadequate tissue perfusion?
In a patient experiencing hypovolemic shock, what is the primary underlying issue, and how does it lead to inadequate tissue perfusion?
During blood pressure measurement using a sphygmomanometer, what physiological event corresponds to the systolic pressure reading?
During blood pressure measurement using a sphygmomanometer, what physiological event corresponds to the systolic pressure reading?
How does the unique biconcave disc shape of red blood cells enhance their function in oxygen transport?
How does the unique biconcave disc shape of red blood cells enhance their function in oxygen transport?
How do granular leukocytes, specifically neutrophils, contribute to the body's defense mechanisms?
How do granular leukocytes, specifically neutrophils, contribute to the body's defense mechanisms?
Which of the following best describes the role of platelets (thrombocytes) in hemostasis?
Which of the following best describes the role of platelets (thrombocytes) in hemostasis?
What are the potential effects of chronic leukocytosis on the body?
What are the potential effects of chronic leukocytosis on the body?
If a patient has damage to their sinoatrial (SA) node, what is the most likely consequence?
If a patient has damage to their sinoatrial (SA) node, what is the most likely consequence?
Which layer of the heart wall is responsible for the heart's pumping action?
Which layer of the heart wall is responsible for the heart's pumping action?
Which of the following is the correct order of blood flow through the pulmonary circulation?
Which of the following is the correct order of blood flow through the pulmonary circulation?
A doctor notes the following vital signs for a patient: heart rate of 50 bpm and stroke volume of 70 mL/beat. Calculate the cardiac output and determine if it falls within the normal range (4-8 L/min).
A doctor notes the following vital signs for a patient: heart rate of 50 bpm and stroke volume of 70 mL/beat. Calculate the cardiac output and determine if it falls within the normal range (4-8 L/min).
Flashcards
Blood Volume
Blood Volume
The volume of blood in the human body. Males typically have 5-6 liters, while females have 4-5 liters.
Regulation (Blood Function)
Regulation (Blood Function)
Maintaining pH, body temperature, and osmotic pressure to ensure proper physiological conditions.
Red Blood Cells (Erythrocytes)
Red Blood Cells (Erythrocytes)
Biconcave discs lacking a nucleus. Transport oxygen via hemoglobin and have a lifespan of ~120 days.
Leukocytosis
Leukocytosis
Signup and view all the flashcards
Polycythemia
Polycythemia
Signup and view all the flashcards
Erythropoietin (EPO)
Erythropoietin (EPO)
Signup and view all the flashcards
Type O Blood
Type O Blood
Signup and view all the flashcards
Apex of the Heart
Apex of the Heart
Signup and view all the flashcards
Base of the Heart
Base of the Heart
Signup and view all the flashcards
Atrioventricular Valves
Atrioventricular Valves
Signup and view all the flashcards
Systemic Circulation
Systemic Circulation
Signup and view all the flashcards
Pulmonary Circulation
Pulmonary Circulation
Signup and view all the flashcards
Myocardium
Myocardium
Signup and view all the flashcards
Sinoatrial (SA) Node
Sinoatrial (SA) Node
Signup and view all the flashcards
Cardiac Output Formula
Cardiac Output Formula
Signup and view all the flashcards
Stenosis (Valve)
Stenosis (Valve)
Signup and view all the flashcards
Congestive Heart Failure
Congestive Heart Failure
Signup and view all the flashcards
Arteries
Arteries
Signup and view all the flashcards
Veins
Veins
Signup and view all the flashcards
Korotkoff Sounds
Korotkoff Sounds
Signup and view all the flashcards
Study Notes
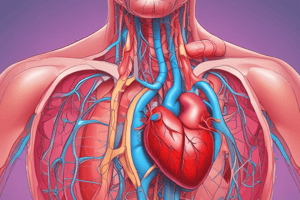
- Exam 2 Study Guide covers Blood, The Heart and Cardiovascular Function, and Blood Vessels and Circulation
Blood Volume and Properties
- Blood volume in males is 5-6 liters, while in females it is 4-5 liters.
- Blood temperature is approximately 38°C (100.4°F).
- Blood pH ranges from 7.35 to 7.45, making it slightly alkaline.
- Blood is a liquid connective tissue, thicker than water and slightly sticky.
Functions of Blood
- Blood transports gases (O₂ and CO₂), nutrients, hormones, and waste products.
- Blood maintains pH, body temperature, and osmotic pressure.
- Blood provides clotting mechanisms and immune cells (white blood cells) along with proteins for protection.
Components of Blood
- Blood plasma is composed of 91.5% water and 8.5% solutes, primarily proteins like albumin and fibrinogen, that maintain osmotic balance.
- Red Blood Cells (RBCs/Erythrocytes) have a biconcave disc shape to maximize surface area for oxygen exchange.
- RBCs lack a nucleus and mitochondria and live for about 120 days.
- Males average 5.4 million RBCs/µL, while females average 4.8 million RBCs/µL.
- Hemoglobin in RBCs contains four polypeptide chains, each with a heme group that binds oxygen.
- White Blood Cells (WBCs/Leukocytes) are divided into granular (neutrophils, eosinophils, basophils) and agranular (lymphocytes, monocytes) types.
- Neutrophils are the most common WBCs and are key phagocytes.
- Lymphocytes include B cells (antibody production), T cells (cell-mediated immunity), and NK cells (tumor/infected cell destruction).
- Leukocytosis (increased WBC count) is a normal response to stress/infection, while leukopenia is harmful.
- Platelets (Thrombocytes) are small cell fragments produced by megakaryocyte fragmentation.
- Platelets are essential for hemostasis, aggregating to form plugs and initiate the clotting cascade, with a short lifespan of 5–9 days.
Additional Blood Concepts
- Polycythemia is an abnormally high percentage of RBCs, increasing blood viscosity and potentially impeding flow.
- Erythropoietin (EPO) stimulates RBC production (erythropoiesis).
- Thrombopoietin (TPO) stimulates platelet production.
- Blood groups are based on A and B antigens (and the Rh factor).
- Type A blood has antigen A and contains anti-B antibodies.
- Type B blood has antigen B and contains anti-A antibodies.
- Type AB blood has both A and B antigens, making it the universal recipient.
- Type O blood lacks both A and B antigens, making it the universal donor.
Heart Anatomy and Orientation
- The heart resides in the mediastinum, between the lungs, extending from the sternum to the vertebral column.
- The apex is the inferior, leftward-pointing tip of the heart resting on the diaphragm.
- The base is the superior surface of the heart.
- The atria (upper chambers) receive blood, while the ventricles (lower chambers) pump blood out.
- Interatrial and interventricular septa separate the left and right sides of the heart.
- Atrioventricular Valves: Tricuspid (right) and Mitral/Bicuspid (left) open during atrial contraction and close during ventricular systole.
- Semilunar Valves: Pulmonary (right) and Aortic (left) prevent backflow during ventricular relaxation.
Blood Flow and Circulatory Routes
- Systemic Circulation: Left atrium → Mitral valve → Left ventricle → Aortic valve → Aorta → Body tissues → Superior/Inferior vena cava → Right atrium, transporting oxygenated blood to the body.
- Pulmonary Circulation: Right atrium → Tricuspid valve → Right ventricle → Pulmonary valve → Pulmonary trunk → Pulmonary arteries → Lungs (oxygenation) → Pulmonary veins → Left atrium, transporting deoxygenated blood to the lungs and returns oxygenated blood.
Layers of the Heart Wall and Pericardium
- Epicardium: Outermost protective layer of the heart wall.
- Myocardium: Thick, muscular middle layer of the heart wall (95% cardiac muscle).
- Endocardium: Smooth, innermost lining of the heart wall that minimizes friction.
- Pericardium: Double-layered membrane consisting of the fibrous pericardium (outer, tough layer) and the serous pericardium (inner, with parietal and visceral layers).
- The pericardial cavity, located between the pericardial layers, contains lubricating fluid.
Cardiac Conduction and Regulation
- The conduction system starts at the Sinoatrial (SA) Node (the natural pacemaker in the right atrium), passes to the Atrioventricular (AV) Node, then through the Bundle of His, bundle branches, and finally through Purkinje fibers to stimulate ventricular contraction.
- The autonomic nervous system regulates heart function: Epinephrine increases heart rate and contractility, while acetylcholine decreases heart rate.
- Thyroid hormones further modulate heart rate and strength of contraction.
- Cardiac Output = Stroke Volume × Heart Rate.
- Regulating Factors of Cardiac Output: Preload (degree of stretch), contractility, and afterload (pressure to overcome).
Clinical Terms and Conditions
- Stenosis: Narrowing of a valve restricting blood flow (e.g., mitral stenosis).
- Mitral Valve Prolapse: Incomplete closure of the mitral valve.
- Congestive heart failure describes a loss of pumping efficiency.
- Left ventricle failure often leads to pulmonary edema; right ventricle failure to peripheral edema.
- Auscultation: Heart sounds (“Lubb” = closure of atrioventricular valves; “Dupp” = closure of semilunar valves) are used to assess valve function.
- A patent foramen ovale or Tetralogy of Fallot (“blue baby”) are examples of congenital defects that affect normal blood flow.
Types and Structure of Blood Vessels
- Arteries carry blood away from the heart and typically have thick, muscular walls (tunica media) for withstanding high pressure.
- Veins return blood to the heart and have thinner walls, larger lumens, and valves to prevent backflow.
- Capillaries are the smallest vessels where the exchange of gases, nutrients, and waste occurs.
Hemodynamics and Vascular Resistance
- Vascular Resistance Factors: Lumen size (vasoconstriction increases resistance), blood viscosity (thicker blood increases resistance), and vessel length (longer vessels create more friction).
- Blood Pressure Measurement: Typically measured at the brachial artery using a sphygmomanometer.
- Korotkoff Sounds: The first audible sound marks systolic pressure, and the disappearance of sound marks diastolic pressure.
- Shock: A state where the cardiovascular system fails to deliver sufficient oxygen and nutrients.
- Types of Shock: Hypovolemic (low blood volume), cardiogenic (poor heart pump), vascular (excessive vasodilation), and obstructive (blockage in circulation).
Major Vessels
- The ascending aorta gives off the coronary arteries.
- The arch of the aorta branches into the brachiocephalic trunk, common carotid, and subclavian arteries.
- The superior and inferior vena cava return deoxygenated blood to the right atrium.
- Specific veins (e.g., coronary sinus, jugular veins) drain defined regions of the body.
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.