Podcast
Questions and Answers
What is the primary function of circulation?
What is the primary function of circulation?
- To regulate body temperature
- To facilitate muscle movement
- To remove waste from cells
- To supply cells with the materials needed for survival (correct)
Hemodynamics is the study of the structure of the heart.
Hemodynamics is the study of the structure of the heart.
False (B)
Why do more active cells need more blood per minute?
Why do more active cells need more blood per minute?
Because they require more oxygen and nutrients to support their increased metabolic activity.
Circulation is the only means by which cells can receive _______________ needed for survival and have their waste removed.
Circulation is the only means by which cells can receive _______________ needed for survival and have their waste removed.
Match the following statements with their correct descriptions:
Match the following statements with their correct descriptions:
What is the primary importance of circulation?
What is the primary importance of circulation?
What happens to the membrane when it reaches the threshold potential?
What happens to the membrane when it reaches the threshold potential?
Conduction fibers are specifically adapted for slow conduction through the syncytium.
Conduction fibers are specifically adapted for slow conduction through the syncytium.
What is the term for the continuous production of action potentials in the syncytium?
What is the term for the continuous production of action potentials in the syncytium?
The impulse conduction generates tiny electrical currents in the heart that spread through the surrounding tissues to the surface of the body, which can be recorded by an _______________________.
The impulse conduction generates tiny electrical currents in the heart that spread through the surrounding tissues to the surface of the body, which can be recorded by an _______________________.
Match the following components of the heart with their functions:
Match the following components of the heart with their functions:
What is the term for the specialized fibers that carry action potentials from pacemakers to more distant areas of the syncytium?
What is the term for the specialized fibers that carry action potentials from pacemakers to more distant areas of the syncytium?
What event marks the beginning of atrial systole?
What event marks the beginning of atrial systole?
During atrial systole, the AV valves are closed.
During atrial systole, the AV valves are closed.
What is the result of the contracting force created during atrial systole?
What is the result of the contracting force created during atrial systole?
Atrial systole is characterized by the electrical wave of _______________________ followed by contracting myocardium of the atria.
Atrial systole is characterized by the electrical wave of _______________________ followed by contracting myocardium of the atria.
Match the following events with their descriptions:
Match the following events with their descriptions:
Atrial systole occurs simultaneously with ventricular systole.
Atrial systole occurs simultaneously with ventricular systole.
Which of the following nerves is involved in the parasympathetic impulses that regulate the heart rate?
Which of the following nerves is involved in the parasympathetic impulses that regulate the heart rate?
Increased peripheral resistance decreases blood flow.
Increased peripheral resistance decreases blood flow.
What type of reflex is influenced by emotions, exercise, hormones, blood temperature, pain, and stimulation of various exteroceptors?
What type of reflex is influenced by emotions, exercise, hormones, blood temperature, pain, and stimulation of various exteroceptors?
The cardiac control center sends parasympathetic impulses through the _______________________ nerve to reach the SA node.
The cardiac control center sends parasympathetic impulses through the _______________________ nerve to reach the SA node.
Match the following terms with their definitions:
Match the following terms with their definitions:
What type of impulses travel from the cardiac control center to the SA node?
What type of impulses travel from the cardiac control center to the SA node?
Where are the receptors sensitive to changes in pressure located in the heart?
Where are the receptors sensitive to changes in pressure located in the heart?
The carotid sinus reflex is located at the end of the internal carotid artery.
The carotid sinus reflex is located at the end of the internal carotid artery.
What nerve do the sensory fibers from carotid sinus baroreceptors run through?
What nerve do the sensory fibers from carotid sinus baroreceptors run through?
The carotid sinus reflex is located at the _______________________ of the internal carotid artery.
The carotid sinus reflex is located at the _______________________ of the internal carotid artery.
Match the following types of receptors with their locations:
Match the following types of receptors with their locations:
What is the path of the sensory fibers from carotid sinus baroreceptors?
What is the path of the sensory fibers from carotid sinus baroreceptors?
Match the following components of the heart with their descriptions:
Match the following components of the heart with their descriptions:
Match the following nerves with their functions:
Match the following nerves with their functions:
Match the following reflexes with their descriptions:
Match the following reflexes with their descriptions:
Match the following components with their locations:
Match the following components with their locations:
Match the following fibers with their functions:
Match the following fibers with their functions:
Match the following descriptions with their corresponding components:
Match the following descriptions with their corresponding components:
Match the following components with their corresponding functions:
Match the following components with their corresponding functions:
Match the following components with their corresponding locations:
Match the following components with their corresponding locations:
Match the following descriptions with their corresponding components:
Match the following descriptions with their corresponding components:
Match the following components with their corresponding functions:
Match the following components with their corresponding functions:
What happens to the ventricular pressure when the SL valves close?
What happens to the ventricular pressure when the SL valves close?
What is the result of the closure of the SL valves?
What is the result of the closure of the SL valves?
Why do the SL valves close?
Why do the SL valves close?
What is the significance of the SL valves snapping shut?
What is the significance of the SL valves snapping shut?
What happens to the volume of the ventricular chambers when the SL valves close?
What happens to the volume of the ventricular chambers when the SL valves close?
What is the purpose of the closure of both sets of valves?
What is the purpose of the closure of both sets of valves?
What occurs at the end of ventricular ejection?
What occurs at the end of ventricular ejection?
What is the result of the closure of the SL valves on ventricular pressure?
What is the result of the closure of the SL valves on ventricular pressure?
What is the significance of the second heart sound?
What is the significance of the second heart sound?
What is the purpose of the SL valves?
What is the purpose of the SL valves?
Flashcards are hidden until you start studying
Study Notes
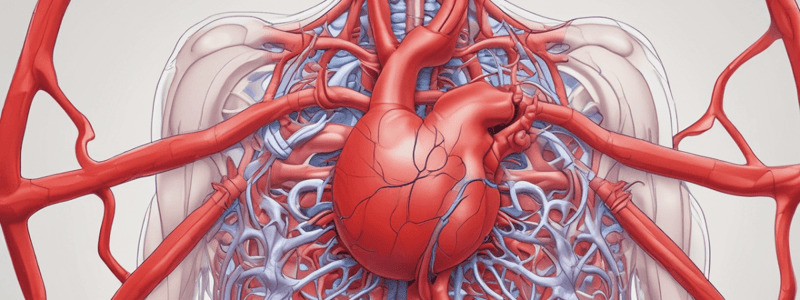
Hemodynamics
- Hemodynamics is a collection of mechanisms that influence the active and changing circulation of blood.
- Circulation is a vital function and the only means by which cells can receive materials needed for survival and have their waste removed.
- Different volumes of blood per minute are required for different organs at different times.
- More active cells need more blood per minute than less active cells.
Conduction Mechanisms
- Conduction fibers are specifically adapted for rapid conduction through the syncytium.
- They are high-speed carriers of action potential from pacemakers to more distant areas of the syncytium.
Electrocardiogram
- Impulse conduction generates tiny electrical currents in the heart that spread through surrounding tissues to the surface of the body.
- The atrial systole begins with the P wave of the ECG, which is an electrical wave of depolarization followed by contracting (systole) myocardium of the atria.
- The contracting force creates a pressure gradient that pushes blood out of the atria into the relaxed ventricles.
- The AV (cuspid) valves remain open during this phase.
Cardiac Reflexes
- Cardiac pressoreflexes involve receptors sensitive to changes in pressure located in two places in the heart: aortic baroreceptors and carotid baroreceptors.
- The carotid sinus reflex is located at the beginning of the internal carotid artery and involves sensory fibers running through the carotid sinus nerve and the glossopharyngeal nerve to the cardiac control center.
- Parasympathetic impulses leave the cardiac control center, travel through the Vagus nerve, and reach the SA node.
- The aortic reflex and other reflexes, including emotions, exercise, hormones, blood temperature, pain, and stimulation of various exteroceptors, also influence the heart.
Peripheral Resistance
- Peripheral resistance is the resistance to blood flow imposed by the force of friction between blood and the walls of its vessels.
Heart Structure and Function
- Valves ensure one-way flow, enabling the heart to act as a pump.
- The heart is divided into four chambers: two upper chambers called the Atria (atrium singular) and two lower chambers called the Ventricles.
- The Atria are separated into left and right chambers by a septum (interatrial septum).
- The Atria are called "receiving chambers" as they receive blood from veins.
- Veins pump blood toward the heart from various tissues.
ECG Waves
- The T wave reflects repolarization of the ventricles.
- An inverted T wave is often seen after myocardial muscle damage.
- A U wave can appear as a tiny hump at the end of the T wave, representing late repolarization of subendocardial branches (Purkinje fibers) in the papillary muscle of the ventricular myocardium.
Blood Pressure Regulation
- Arterial blood pressure is proportional to arterial blood volume.
- An increase in arterial blood volume increases arterial pressure, and vice versa.
- Factors that determine arterial pressure include cardiac output (CO) and peripheral resistance.
Cardiac Output and Peripheral Resistance
- Cardiac output affects the blood entering the arteries.
- If cardiac input increases, the amount of blood entering the arteries increases, tending to increase the volume in the arteries.
- Peripheral resistance affects the blood leaving the arteries.
- If peripheral resistance increases, it decreases the amount of blood leaving the arteries, which increases the amount of blood left in them.
Ejection Fraction and Afterload
- Ejection fraction (EF) is the ratio of stroke volume (SV) to end-diastolic volume (EDV).
- EF is usually expressed as a percentage (EF = (SV ÷ EDV) × 100).
- Healthy adults have an EF of at least 55%.
- EF goes down as the myocardium fails.
- Afterload is also influenced by neutral factors.
- Unusually high afterload from flow resistance in arteries can cause heart failure.
Cardiac Pressoreflexes
- Cardiac pressoreflexes have receptors sensitive to changes in pressure located in two places in the heart: aortic baroreceptors and carotid baroreceptors.
- The carotid sinus reflex is located at the beginning of the internal carotid artery.
- Sensory fibers from carotid sinus baroreceptors run through the carotid sinus nerve and the glossopharyngeal nerve to the cardiac control center.
Hemodynamics and Cardiovascular System
- Many controls mechanisms help regulate and integrate each function and component of the cardiovascular system.
- Hemodynamics refers to the collection of mechanisms that influence the active and changing circulation of blood.
Circulation
- Circulation is a vital function and the only means by which cells can receive material needed for survival and have their waste removed.
- Different organs require circulation of different volumes of blood per minute at different times.
- More active cells need more blood per minute than less active cells.
Electrocardiogram (ECG)
- The T wave reflects repolarization of the ventricles.
- An inverted T wave is often seen after myocardial muscle damage.
- Sometimes a U wave can appear as a tiny hump at the end of the T wave, representing late repolarization of subendocardial branches (Purkinje fibers) in the papillary muscle of the ventricular myocardium.
Cardiac Cycle
- One cycle consists of contraction (systole) and relaxation (diastole) of both atria and both ventricles.
- The two atria contract simultaneously, then as they relax, the two ventricles contract and relax, giving the heart a pumping action.
- The cardiac cycle illustrates and integrates changes in pressure gradients in the left atrium, left ventricle, and aorta.
Steps of the Cardiac Cycle
- Step 1: SL valves remain closed as the arterial pressure is higher than the pressure in the relaxed ventricles.
- Step 2: Isovolumic ventricular contraction, where intraventricular pressure begins to increase, closing the AV valves and producing the first heart sound.
- Step 3: End of ventricular ejection, the SL valves close when the ventricular pressure drops, producing the second heart sound.
- Step 4: (Not mentioned in the text)
- Step 5: (Not mentioned in the text)
Heart Failure
- In heart failure, the residual volume remaining in the ventricles may greatly exceed that ejected during systole.
- Diastasis-reduced ventricular filling of the heart occurs in heart failure.
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.