Podcast
Questions and Answers
What characteristic of cardiomyocytes allows for the rapid and synchronous contraction of the atria or ventricles?
What characteristic of cardiomyocytes allows for the rapid and synchronous contraction of the atria or ventricles?
- The presence of desmosomes provides structural support, preventing overstretching.
- Electrical insulation between the atria and ventricles prevents simultaneous contraction.
- Independent innervation by motor neurons allows for fine-tuned control of contraction.
- Gap junctions facilitate direct electrical communication, creating an electrical syncytium. (correct)
How does the unique structure of elastic arteries contribute to maintaining continuous blood flow throughout the cardiac cycle?
How does the unique structure of elastic arteries contribute to maintaining continuous blood flow throughout the cardiac cycle?
- The presence of valves ensures unidirectional blood flow, preventing backflow during diastole.
- A high number of vasa vasorum in the tunica externa provides structural support, preventing vessel collapse.
- The thick tunica media with abundant smooth muscle allows for active regulation of blood pressure.
- Elastic sheets in the tunics expand to absorb systolic pressure and recoil to maintain flow during diastole. (correct)
What is the functional significance of the heart being enclosed within the pericardium?
What is the functional significance of the heart being enclosed within the pericardium?
- The serous membrane's dense connective tissue protects and anchors the heart, preventing overfilling.
- The double-walled sac encloses the heart to prevent friction while allowing for movement. (correct)
- The pericardium provides structural support, defining the boundaries of the four heart chambers.
- The fibrous membrane produces serous fluid, acting as the primary source of nutrients for the heart.
What is the effect of increased blood pressure on the semilunar valves?
What is the effect of increased blood pressure on the semilunar valves?
How does the ANS influence the heart?
How does the ANS influence the heart?
What is the significance of the longer action potential duration and refractory period in cardiac muscle compared to skeletal muscle?
What is the significance of the longer action potential duration and refractory period in cardiac muscle compared to skeletal muscle?
If the sinoatrial (SA) node fails what happens?
If the sinoatrial (SA) node fails what happens?
Which statement captures the relationship between blood pressure and the cardiac muscle system?
Which statement captures the relationship between blood pressure and the cardiac muscle system?
What physiological mechanism ensures unidirectional blood flow in veins, particularly against gravity in the lower extremities?
What physiological mechanism ensures unidirectional blood flow in veins, particularly against gravity in the lower extremities?
What structural feature of capillaries optimizes the exchange of gases, nutrients, and waste products between blood and tissues?
What structural feature of capillaries optimizes the exchange of gases, nutrients, and waste products between blood and tissues?
How can congenital defects like ventricular septal defect disrupt normal cardiovascular physiology?
How can congenital defects like ventricular septal defect disrupt normal cardiovascular physiology?
What is the significance of arterioles, as the smallest arteries, having the ability to vasodilate?
What is the significance of arterioles, as the smallest arteries, having the ability to vasodilate?
What physiological consequence is associated with chronic tachycardia?
What physiological consequence is associated with chronic tachycardia?
During high-intensity exercise, how does blood flow distribution shift to support increased metabolic demands?
During high-intensity exercise, how does blood flow distribution shift to support increased metabolic demands?
Which of the following explains the relatively high oxygen demand of the heart?
Which of the following explains the relatively high oxygen demand of the heart?
Which description of the interplay of the cardiac system (atria and ventricles) is correct?
Which description of the interplay of the cardiac system (atria and ventricles) is correct?
Which of the following characteristics are associated with veins?
Which of the following characteristics are associated with veins?
You're analyzing an ECG readout. You notice the QRS wave is extremely large. What do you infer from this?
You're analyzing an ECG readout. You notice the QRS wave is extremely large. What do you infer from this?
What causes the condition known as the 'waterfall' of cardiac signals in the right chambers versus the left?
What causes the condition known as the 'waterfall' of cardiac signals in the right chambers versus the left?
The right receives blood from what circuit?
The right receives blood from what circuit?
Why did the cardiac system evolve?
Why did the cardiac system evolve?
What is the relation of the circulatory system to homeostasis?
What is the relation of the circulatory system to homeostasis?
If a patient has been in hypothermia for an extended period, what can we expect to see?
If a patient has been in hypothermia for an extended period, what can we expect to see?
Arteries leaving the right ventricle will supply what?
Arteries leaving the right ventricle will supply what?
Which of the following is accurate about the cardiac system?
Which of the following is accurate about the cardiac system?
If the blockage of coronary blood vessels occurs slowly, what happens?
If the blockage of coronary blood vessels occurs slowly, what happens?
What is the purpose of the Purkinje fibers?
What is the purpose of the Purkinje fibers?
Which statement describes correct relation of blood vessels?
Which statement describes correct relation of blood vessels?
Select the statement that describes the 'plumbing' correcty.
Select the statement that describes the 'plumbing' correcty.
Which statement applies to blood?
Which statement applies to blood?
What is the impact of the Renin Angiotensin Aldosterone system if there is a drop in blood pressure?
What is the impact of the Renin Angiotensin Aldosterone system if there is a drop in blood pressure?
What's one way a brain can be drained if some of a brain's venous system is atypical in terms of layout?
What's one way a brain can be drained if some of a brain's venous system is atypical in terms of layout?
The baroreceptor are responsible for...?
The baroreceptor are responsible for...?
Which statement is accurate?
Which statement is accurate?
What function do the brain and digestive systems have in common?
What function do the brain and digestive systems have in common?
What is the result of action from skeletal muscles?
What is the result of action from skeletal muscles?
Which statement applies to resistance to bloodflow?
Which statement applies to resistance to bloodflow?
In an EKG reading, what indicates atrial contraction?
In an EKG reading, what indicates atrial contraction?
In response to damage to the myocardium how does that present?
In response to damage to the myocardium how does that present?
Flashcards
Circulatory System
Circulatory System
The system where blood circulates, driven by the heart's pumping action.
Pulmonary Circuit
Pulmonary Circuit
The circuit between the heart and lungs for gas exchange.
Systemic Circuit
Systemic Circuit
The circuit between the heart and the rest of the body.
Closed Circulatory System
Closed Circulatory System
Signup and view all the flashcards
Arteries
Arteries
Signup and view all the flashcards
Veins
Veins
Signup and view all the flashcards
Capillary Beds
Capillary Beds
Signup and view all the flashcards
Mediastinum
Mediastinum
Signup and view all the flashcards
Pericardium
Pericardium
Signup and view all the flashcards
Myocardium
Myocardium
Signup and view all the flashcards
Cardiomyocytes
Cardiomyocytes
Signup and view all the flashcards
Intercalated Discs
Intercalated Discs
Signup and view all the flashcards
Atria and Ventricles
Atria and Ventricles
Signup and view all the flashcards
Systole
Systole
Signup and view all the flashcards
Diastole
Diastole
Signup and view all the flashcards
Endocardium
Endocardium
Signup and view all the flashcards
Endocardium
Endocardium
Signup and view all the flashcards
Atria
Atria
Signup and view all the flashcards
Ventricles
Ventricles
Signup and view all the flashcards
Afferent Blood Vessels
Afferent Blood Vessels
Signup and view all the flashcards
Efferent Blood Vessels
Efferent Blood Vessels
Signup and view all the flashcards
Heart Valves
Heart Valves
Signup and view all the flashcards
Atrioventricular Valves
Atrioventricular Valves
Signup and view all the flashcards
SA Node
SA Node
Signup and view all the flashcards
AV Node
AV Node
Signup and view all the flashcards
Blood Pressure
Blood Pressure
Signup and view all the flashcards
ANS
ANS
Signup and view all the flashcards
Sympathetic Branch
Sympathetic Branch
Signup and view all the flashcards
Parasympathetic Branch
Parasympathetic Branch
Signup and view all the flashcards
Medulla Oblongata
Medulla Oblongata
Signup and view all the flashcards
Norepinephrine Influence
Norepinephrine Influence
Signup and view all the flashcards
Acetycholine Influence
Acetycholine Influence
Signup and view all the flashcards
Electrolyte Imbalances
Electrolyte Imbalances
Signup and view all the flashcards
Tachycardia
Tachycardia
Signup and view all the flashcards
Bradycardia
Bradycardia
Signup and view all the flashcards
Congestive Heart Failure
Congestive Heart Failure
Signup and view all the flashcards
Blood Vessels
Blood Vessels
Signup and view all the flashcards
Capillary Beds
Capillary Beds
Signup and view all the flashcards
Unidirectional Blood Flow
Unidirectional Blood Flow
Signup and view all the flashcards
Study Notes
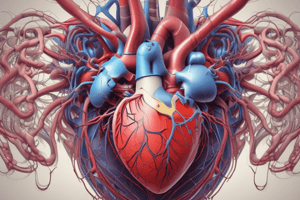
Cardiovascular System
- Blood circulates within the circulatory system, driven by the heart's pumping action.
- The circulatory system consists of two circuits originating from the heart.
- Pulmonary circuit (heart and lungs).
- Systemic circuit (heart and the rest of the body).
- Blood remains within blood vessels at all times, functioning as a closed circulatory system.
- Arteries carry blood away from the heart.
- Veins carry blood back to the heart.
- Branching, fine capillary beds connect arteries and veins, facilitating the exchange between blood and tissues.
Heart Anatomy
- The mediastinum in the thoracic cavity houses the heart, slightly off-center to the left.
- Anterior to the vertebral Column and superior to the diaphragm, separating the thoracic and abdominal cavity.
- The heart is flanked and partly obscured by the lungs.
- The heart is enclosed by the pericardium which is a double-walled sac to protect and prevent overfilling.
- Serous membranes.
- Fibrous membrane.
- The pericardium consists of several tissue layers.
- Fibrous pericardium: Dense connective tissue that protects and anchors the heart.
- Serous Pericardium: A serous membrane that forms a sac around the heart; includes parietal and visceral layers separated by the pericardial cavity filled with fluid.
- Myocardium: "Heart Muscle".
- Cardiac muscle: Striated cardiac muscle cells called cardiomyocytes form a hollow muscle.
- Cardiomyocytes: Mechanically interconnected by connective tissue fibers, known as the cardiac skeleton, for structural support and electrical insulation.
- Cardiomyocytes have no origin and no insertion.
- Intercalated Discs and Desmosomes connect cardiomyocytes.
- The heart has two functional/contractile subunits which are Electrically insulated and Contract Independently.
- Atria (2).
- Ventricles (2).
- Systole refers to contraction, usually of the ventricles.
- Diastole refers to relaxation usually of the ventricles.
- Ventricular systole corresponds to atrial diastole and vice versa.
- Endocardium: The inner heart wall.
- Squamous epithelial tissue is on the connective tissue that lines the heart chambers and heart valves.
- Continuous epithelial lining of the heart with the endothelial lining of blood vessels acts as a "blood proof" barrier.
- The human heart has four chambers.
- Two superior atria (atrium).
- Two inferior ventricles (ventricle).
- Atria are longitudinally separated by the interatrial septum.
- Ventricles are longitudinally separated by the interventricular septum.
- The right ventricle receives blood from the right atrium.
- The left ventricle receives blood from the left atrium.
- The right atrium receives blood from the left ventricle via the systemic circuit (body circuit).
- The left atrium receives blood from the right ventricle via the pulmonary circuit (lung circuit).
- Afferent blood vessels carry blood back to the heart (veins).
- Efferent blood vessels carry blood away from the heart (arteries).
- Atria fill ventricles, ventricles fill arteries, veins fill atria.
- The right side of the heart (right atrium/ventricle) drives the pulmonary circuit.
- The left side of the heart (left atrium/ventricle) drives the systemic circuit.
- Veins connect and bring blood to atria.
- Atria connect and bring blood to ventricles.
- Ventricles connect to arteries for blood to be carried away.
- Capillary beds facilitate transitions from the arterial to the venous system.
- The logic or reason the right and left sides of the hearts drive the pulmonary and systemic circuits is unknown, just that evolution has made it this way.
- Pressure-operated valves in afferent (veins) and efferent (arteries) blood vessels, and between the atria and ventricles, ensure unidirectional blood flow.
- Heart valves are connective tissue flaps that open and close in response to blood pressure changes in the different heart sections.
- The returning blood fills the atria, which forces the atrioventricular (AV) valves open when the atria are contracting.
- As the returned blood fills the ventricles, the AV valve flaps hang limply.
- AV valves open when the atrial pressure exceeds the ventricular pressure.
- As the ventricles contract, the AV valves close to prevent backflow of blood into the atria.
- Papillary muscles and chordae tendineae prevent valve flaps from everting into the atria.
- When AV valves are closed, atrial pressure is less than ventricular pressure.
- Valves in Afferent Veins work the same way and Valves in Arteries work the same way!
- High blood pressure upstream forces them open.
- "Upstream" means further away from the heart.
- Higher blood pressure downstream forces them closed.
- "Downstream" means closer to the heart.
- The left ventricle is stronger to generate more force and pressure.
Heart Physiological Requirements
- Muscle contraction consumes substantial amounts of energy.
- Only energy metabolism by aerobic respiration is sustainable over an extended time, fueled by organic substrates and O₂.
- Circulatory system transports O₂ and nutrients to muscles and other energy consumers.
- Heart requires constant activity 24/7 or the deficiency stops the flow of blood and nutrients to the tissues causing necrosis.
- The heart has top priority for O₂ and nutrient supply next to the brain.
- Blockage of coronary blood vessels damages cardiac tissue irreversibly and compromises heart function.
- Also known as "coronary" infarct, otherwise called a heart attack.
- Myocardium is striated with cardiomyocytes.
- Heart cells branch and connect with intercalated discs.
- Firm mechanical joints form between cell membranes via desmosomes.
- The myocardium acts as an electrical syncytium by forming gap junctions.
- The heart beats and contracts and is controlled by intrinsic "pacemakers" that are specialized cardiomyocytes and frequently auto-depolarize called a myogenic heart.
- Pacemakers' cell excitation spreads over the entire myocardium.
- Human hearts are not innervated by motor neurons.
- It has a longer action potential duration, which ensures complete contraction.
- The longer refractory period prevents tetanus and ensures full muscle relaxation between contractions.
- There are multiple pacemaker centers in the human heart.
- The SA Node is the fastest Spontaneous Electrical Depolarization.
- The SA-node is the primary pacemaker, fastest spontaneous electrical depolarization frequency, imposed on secondary and tertiary pacemakers, entire heart.
- When the SA Node fails then the AV Node takes over, and when the AV Node fails then the Purkinje Fibers take over.
- There is a connective tissue barrier electrically isolates atria and ventricles which causes depolarization to not spread directly from the atira to ventricles.
- Depolarizing pacemaker potential is intrinsically generated by the specialized cardiac muscle cells/pacemakers.
- Pacemaker action potential spreads via gap junctions over the entire myocardium (syncytium).
- Cardiac muscle contracts simultaneously.
- The refractory period in cardiac cells prevents tetanus as it repolarizes.
- Atrial muscle is active before ventricles.
- Ventricles only become active after the atria have ceased activity where Atria have ended activity!
Heart Regulation
- Atrial pressure fills ventricles as ventricular blood pressure fills atria.
- Blood pressure opposes to the cardiac muscle system without muscular antagonists.
- Contraction of the myocardium generates blood pressure.
- When muscle cells of the atria are excited and contract, ventricle cells relax and the reverse.
- There is extrinsic innervation of the heart by the Autonomic Nervous System (ANS).
- The sympathetic branch accelerates to increase the heart rate / contraction force.
- The Vagus nerve(parasympathetic) branch to decelerate slows heart rate and vigor.
- The cardiac control center is located in the medulla oblongata.
- Efferent ANS neurons connect to the cardiac plexus, innervating the SA and AV nodes, myocardium, and smooth muscles of the coronary arteries.
- ANS innervation occurs indirectly via chemical synapses with varicosities in the vicinity of target cells where the neurotransmitters of ANS are released in the extracellular space near target cells/tissues.
- Diffuse hormone-like influence at some distance of the target cells.
- The sympathetic system releases norepinephrine (NE), which increases heart rate and vigor and lowers the pacemaker threshold, thus generating more frequent APs.
- The parasitic system releases acetylcholine (ACh), which reduces heart rate by hyperpolarizing pacemakers and slows down AP frequency.
- Epinephrine, also known as adrenaline, is released by the adrenal medulla and has the same effect as norepinephrine but works in a long-term chronic stress response.
- Thyroxin is released by the thyroid glands and controls metabolic rate and body heat, causes a sustained heart rate increase, and enhances epinephrine/norepinephrine effects (synergistic action).
- An electrolyte imbalance can cause abnormal ion gradients between cells and extracellular space with altered dynamics and kinetics of ion flow across the membrane.
- The shift in the membrane potential affects the generation of APs and repolarization.
Electrolyte Regulation
- Low Ca²⁺: Depresses heart rate.
- High Ca²⁺: Increases heart rate.
- Very High Ca²⁺: Disrupts heart function (arrhythmias).
- High or Low K⁺: Both Dangerous and lead to cardiac arrest because cardiac cells are polarized..
- High K⁺: Hyperpolarizes.
- Low K⁺: Leads to arrhythmias.
Other Regulatory Factors:
- Average heart rate is fastest in the fetus (140-160 bpm) and declines with age.
- Average BPM in females is 72-80 bpm in females.
- Average BPM in males is 64-72 bpm.
- Lower heart rates are found in physically trained individuals.
- Heat(fever) increases heart rate by generally increasing metabolic activity.
- Cold slows metabolism and heart rate.
- Tachycardia is an abnormally fast heart with over 100bpm, caused by high body temperature, drugs, or heart disease, chronic tachycardia increases risk of fibrillation.
- Bradycardia is unusually slow with under 60bpm, caused by low body temperature, drugs, or endurance training, and inadequate by trauma or edema.
- Congestive Heart Failure(CHF): Inadequate heart function due to the Coronary Arteriosclerosis.
- Coronary Arteriosclerosis can lead to hypoxia with clots of fat deposits.
- The left ventricle with a higher than 90mm HG can lead to the heart having to work harder to generate hypertension.
- Myocardial Infarctions(coronary, heart attack) can lead to heart weakening and scar tissue development.
- Dilated Cardiomyopathy degeneration of myocardium affecting mainly ventricles, probably caused by infections and or drugs.
- Imbalances of Maintainance in Blood Circulation due to weakened ventricles lead to Pulmonary Congestion.
- Lack of blood moved caused by one side of the heart, typically the left ventricle, leading to overload of blood and leaking into the lungs(Pulmonary Congestion).
- Peripheral Congestion may occur if there is insufficient volume moved by the side of the heart causing hypoxia and shortage of blood flow.
Congenital "brith" Defects of human hearts:
- Ventricular Septal Defect: An Incomplete formation of Interventricular Septum and incomplete separation of both ventricles which mixing of blood and shunting of blood with weakened Right Ventricle that causes low oxygen levels.
- Narrowed Aorta(Corartation aorta): Increased heart workloads that impact pressure and proper blood volumes pumped into the systemic circuit that can be surgically widened.
- Tetralogy of Fallout(Multiple defects) with a narrowed Pulmonary trunk and pulmonary Valve stenosed (constricted), thus impacting the volume released from the pulmonary circuit.
- Hypertrophy (enlargement) of the right ventricle due to workload with a Ventricular septal defect and Aorta connects to both ventricles for maximized blood volumes.
Blood Vessels
- Lymphatic system vessels form with and are the circulatory system.
- Closed System: Lumen with hearts in the middle. Lymph stays in their vessels at all times.
- Arteries carry blood away
- Veins carry blood toward
- Capillary beds perfuse through tissue.
- Exchange between blood and tissue is all in lymph vessels.
- Flow is driven by fluids.
- Generated by hear drives ventricle to sustain contractions to a larger blood pressure in lymphatic Arterials. -Systolic is pressure at 99 to 120 at Contraction or >140 mm Hg for hyper -Diastolic blood pressures 60+ that are hypertension above this level the person needs immediate attention.
- Tonic beds require much more Differences must be maintained to meet.
- Vascular all made by layers, also called tunnelis or three layers with lumen Inner tunnels are in contact with the blood.
- Middles are middle layers.
- Externus is outside the middle. -Connective tissue which loose collogen support and support. -infiltraded vessel to protect tissue
Arteries and Veins
- Smooth muscle controls cross Section VASOCONSTRICTION restricts cell movement.
- VASOSODULATION for greater.
- Tunics are external as ANS.
- Tynica is to reduce pressure.
- Vasular as most
- Veins are lower pressure
- Veinus walls are different as aterial is stronger
- Lacking vessels
- Pressure needed for the heart.
- Valves provide pressure
- Samples and infusions should be performed before.
- Collaterals must be continuous.
- Collatorations
- The volumes moved have a limit to 5 feet,
- Blood moves throughout or in winds at an increase to cardiac output and resistance.
- Arterial system pressure is highest.
- Action generates is higher from the system to overcome heart failure.
- Strotic pressure maintains ventricle contractions at 90 and the diastolic maintains between 60
- The pulse from the beats maintains systemic functions.
- Higher velocity of blood requires more.
- Maintains flow is maintained required .
- Pressure systems must be controlled with Low pressure with High pressure.
- The highest pressures are in the lymphatic regions.
- Valves maintain resistance.
- High intensity exercises are high levels of C02.
- Blood volume is maintained by control in water pressure as hyrdo smotic concentrations.
- Neuronal controls for short term for c02 control.
- Controls over all functions. Control bloods distrobution , the body.
- Baroreceptors Chemoreceptors Chemo control over a large system of the medulla. Hyerthsamus to command center over the kidneys regulation and filteration. Angiotension promotes kidney filtration
- Aldestrone promotes sodium increases
- Potent pressure for regulation increases. Total flow depends on how high or low. Flow is also based on level. Cardio, cardio shock causes tissues to require more nutrients.
- Aorta supplies major blood vessels.
- Lung veins for O2 blood and supply. Systems are divided to two circuits that control bodily functions and the circulatory system.
- Short to light and back for respiratory gas exchange.
- "Long" long from lungs for vessels.
Systemic Circuits
- Pulmonary Trunk/Circulation Main Arteries
- O2 lungs and supplies a lung wing. Lobar Arteries and Alveoli.
- Arterial supplies in aortic arches to parts of body and smaller arterioles.
- Veins drain system from the body and are Atypical while lymph vessels are opposite.
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.
Related Documents
Description
Overview of the cardiovascular system, including the heart's role in circulating blood through pulmonary and systemic circuits. Discussion of heart anatomy, its location in the mediastinum, and the protective pericardium.