Podcast
Questions and Answers
Which condition is associated with bradycardia?
Which condition is associated with bradycardia?
- Cardiac tamponade
- Anxiety
- High output states
- Myxedema (correct)
Relative bradycardia occurs when there is a rise in heart rate corresponding fairly to a rise in temperature.
Relative bradycardia occurs when there is a rise in heart rate corresponding fairly to a rise in temperature.
False (B)
What heart rate increase is expected for every 1º rise in temperature, based on the relative bradycardia definition?
What heart rate increase is expected for every 1º rise in temperature, based on the relative bradycardia definition?
10 beats/min
Conditions like _____ and _____ usually do not cause relative bradycardia.
Conditions like _____ and _____ usually do not cause relative bradycardia.
Match the condition with its associated cause:
Match the condition with its associated cause:
What condition is indicated by a pulsus bisferiens?
What condition is indicated by a pulsus bisferiens?
A hypokinetic pulse is characterized by an increased amplitude.
A hypokinetic pulse is characterized by an increased amplitude.
What causes a pulsus dicroticus?
What causes a pulsus dicroticus?
A hypokinetic pulse may be observed due to decreased stroke volume caused by ________ dysfunction.
A hypokinetic pulse may be observed due to decreased stroke volume caused by ________ dysfunction.
Match the pulse type with its corresponding characteristic cause:
Match the pulse type with its corresponding characteristic cause:
Which of the following pulse types is characterized by one peak in systole and one peak in diastole?
Which of the following pulse types is characterized by one peak in systole and one peak in diastole?
Hypertrophic cardiomyopathy is associated with a pulsus bisferiens.
Hypertrophic cardiomyopathy is associated with a pulsus bisferiens.
What waveform characteristics are associated with a pulsus tardus and parvus?
What waveform characteristics are associated with a pulsus tardus and parvus?
What is the primary factor indicated by the arterial pulse waveforms?
What is the primary factor indicated by the arterial pulse waveforms?
The velocity of ejection does not affect the shape of the arterial pulse waveform.
The velocity of ejection does not affect the shape of the arterial pulse waveform.
What position should the patient be in to assess the carotid pulse accurately?
What position should the patient be in to assess the carotid pulse accurately?
A pulse apex deficit greater than _____ suggests atrial fibrillation.
A pulse apex deficit greater than _____ suggests atrial fibrillation.
Match the following aspects of arterial pulse to their descriptions:
Match the following aspects of arterial pulse to their descriptions:
What characterizes a pulsus alternans pulse?
What characterizes a pulsus alternans pulse?
Pulsus bigemini involves normal beats that are followed by late contractions.
Pulsus bigemini involves normal beats that are followed by late contractions.
What mechanism is responsible for pulsus alternans?
What mechanism is responsible for pulsus alternans?
Pulsus paradoxus is defined as a systolic blood pressure fall of >___ mmHg during inspiration.
Pulsus paradoxus is defined as a systolic blood pressure fall of >___ mmHg during inspiration.
Match the following terms with their definitions:
Match the following terms with their definitions:
Which of the following conditions can cause pulsus paradoxus?
Which of the following conditions can cause pulsus paradoxus?
Pulsus alternans rhythm is irregular.
Pulsus alternans rhythm is irregular.
What is a clinical feature used to differentiate between MVP and HCM?
What is a clinical feature used to differentiate between MVP and HCM?
Which of the following conditions is characterized by a high amplitude and high volume pulse?
Which of the following conditions is characterized by a high amplitude and high volume pulse?
Irregularly irregular pulses are a feature of atrial fibrillation.
Irregularly irregular pulses are a feature of atrial fibrillation.
What is the effect of rigid atherosclerotic vessels on stroke volume in the elderly?
What is the effect of rigid atherosclerotic vessels on stroke volume in the elderly?
Which virus is the most common cause of post-viral acute pericarditis?
Which virus is the most common cause of post-viral acute pericarditis?
A dicrotic wave becomes less prominent in a condition with __________.
A dicrotic wave becomes less prominent in a condition with __________.
Match the pulse characteristic with its cause:
Match the pulse characteristic with its cause:
Chest pain associated with acute pericarditis is usually dull and non-pleuritic.
Chest pain associated with acute pericarditis is usually dull and non-pleuritic.
What clinical feature is described as a high-pitched, leathery sound heard in acute pericarditis?
What clinical feature is described as a high-pitched, leathery sound heard in acute pericarditis?
Treatment for acute pericarditis commonly includes __________ and colchicine.
Treatment for acute pericarditis commonly includes __________ and colchicine.
Match the cause of acute pericarditis with its corresponding category:
Match the cause of acute pericarditis with its corresponding category:
What is the primary purpose of assessing the Jugular Venous Pulse (JVP)?
What is the primary purpose of assessing the Jugular Venous Pulse (JVP)?
The Internal Jugular Vein (IJV) is less likely to be affected by extrinsic compression compared to the External Jugular Vein (EJV).
The Internal Jugular Vein (IJV) is less likely to be affected by extrinsic compression compared to the External Jugular Vein (EJV).
Name the preferred vessel for assessing the Jugular Venous Pulse (JVP).
Name the preferred vessel for assessing the Jugular Venous Pulse (JVP).
The IJV is located in the _____ triangle, between the sternal and clavicular head of the sternocleidomastoid muscle.
The IJV is located in the _____ triangle, between the sternal and clavicular head of the sternocleidomastoid muscle.
Match the characteristics of jugular veins with their relevance in assessing JVP:
Match the characteristics of jugular veins with their relevance in assessing JVP:
What is the normal delay for the carotid pulse?
What is the normal delay for the carotid pulse?
An exaggerated delay in pulse assessment is a feature of coarctation of the aorta.
An exaggerated delay in pulse assessment is a feature of coarctation of the aorta.
Name one feature of pulse assessment.
Name one feature of pulse assessment.
The smooth dicrotic notch is associated with a decrease in __________.
The smooth dicrotic notch is associated with a decrease in __________.
Match the imaging technique with its findings regarding coarctation of the aorta:
Match the imaging technique with its findings regarding coarctation of the aorta:
What is a common hemodynamic change observed in cardiac tamponade?
What is a common hemodynamic change observed in cardiac tamponade?
Pulsus paradoxus is only present in some patients with cardiac tamponade.
Pulsus paradoxus is only present in some patients with cardiac tamponade.
What is the primary treatment for cardiac tamponade?
What is the primary treatment for cardiac tamponade?
During the subxiphoid approach for pericardiocentesis, the needle is aimed toward the left ______.
During the subxiphoid approach for pericardiocentesis, the needle is aimed toward the left ______.
Match the components of Beck's triad with their descriptions:
Match the components of Beck's triad with their descriptions:
What characterizes the chest pain experienced during myocardial ischemia or infarction?
What characterizes the chest pain experienced during myocardial ischemia or infarction?
Chest pain in pericarditis improves when the patient leans forward.
Chest pain in pericarditis improves when the patient leans forward.
What autoimmune syndrome occurs more than 2-6 weeks after a myocardial infarction?
What autoimmune syndrome occurs more than 2-6 weeks after a myocardial infarction?
In myocardial ischemia, the duration of chest pain is typically _____ minutes, while in infarction it lasts for _____ hours.
In myocardial ischemia, the duration of chest pain is typically _____ minutes, while in infarction it lasts for _____ hours.
Match the following conditions with their characteristic features:
Match the following conditions with their characteristic features:
Flashcards are hidden until you start studying
Study Notes
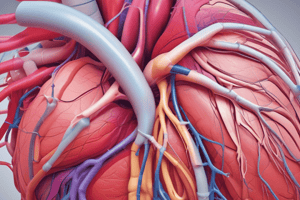
Characterization of Pulse Types
- Pulsus bisferiens: a pulse with two peaks, one in systole and one in diastole
- Causes: severe aortic regurgitation, aortic regurgitation with mild aortic stenosis, hypertrophic cardiomyopathy.
- Mechanism: elevated stroke volume leads to a large amplitude pressure pulse wave.
- Pulsus dicroticus: a pulse with one peak in systole and one peak in diastole
- Cause: left ventricular failure.
- Hypokinetic Pulse: a pulse with a reduced amplitude, often observed in cases of decreased stroke volume due to left ventricular dysfunction.
- Pulsus Tardus and Parvus: a slow and weak pulse, often seen in cases of severe aortic stenosis.
- Palpation: Radial (wrist) arterial pulse palpation is often used to assess pulse types.
Sinus Tachycardia
- Causes: fever, anxiety, exercise, high output states, hypovolemia, myocarditis, anterior wall MI, cardiac tamponade, cardiogenic shock.
Sinus Bradycardia
- Causes: athletes, drugs (beta blockers and calcium channel blockers), increased intracranial tension, hypothermia, inferior wall MI, myxedema (hypothyroidism).
Relative Bradycardia
- Characterized by a rise in heart rate that is not proportional to a rise in temperature.
- For every 1°F rise in temperature, the heart rate should increase by 10 beats/min.
- Other causes: typhoid, Q fever, Legionella, drug fever, lymphoma, CNS lesions, factitious fever.
Pulsus Alternans
- Character: Alternating high and low volume pulse.
- Mechanism: Calcium (Ca²⁺) uptake and release fluctuate, alternating.
- Rhythm: Regular.
Pulsus Bigemini
- Character: Normal beat alternates with premature contractions.
- Mechanism: Stroke volume of the premature beat (PMB) decreases, followed by post-PMB pause.
- Rhythm: Regular.
Pulsus Paradoxus
- Definition: Systolic blood pressure falls by >10 mmHg during inspiration.
- Causes: cardiac tamponade, chronic constrictive pericarditis, COPD, pulmonary embolism, superior vena cava (SVC) obstruction.
Reverse Pulsus Paradoxus
- Definition: Systolic blood pressure increases with inspiration.
- Causes: increased intrathoracic pressure in left ventricular failure, isorhythmic AV dissociation, hypertrophic cardiomyopathy.
Arterial Pulse
- A pressure wave originating in the aorta during left ventricular (LV) systole, traveling along the arterial wall.
- Rate: 5 m/s (faster than the blood column - 50 cm/s).
- Indicator of LV performance status and how the vascular system reacts to it.
- Best felt at the carotid arteries.
Pulse Apex Deficits
- Patient position: Patient in supine position with neck slightly turned towards the side of palpation.
- Assessment: Palpate carotid pulse and simultaneously auscultate for heart sounds.
- Significance: A pulse apex deficit greater than 10 suggests atrial fibrillation.
Hyperkinetic Pulse
- High amplitude / high volume pulse: ↑ SV → ↑ CO.
- In elderly:
- Have rigid atherosclerotic vessels → SV does not increase.
- Volume high (D/t non-distensibility).
- ↓ PVR (To maintain BP)
- Condition with ↓ CO but ↑ amplitude: Complete heart block (CO = SV × HR ↓).
Acute Pericarditis
- Inflammation of the pericardium.
- Causes: infections (post viral, tuberculosis), drugs (procainamide, hydralazine, anthracyclines, minoxidil), tumors, autoimmune conditions (IgG4, SLE, HIV), post-traumatic, post-myocardial infarction (MI), uremia.
- Clinical Features: sharp, pleuritic chest pain relieved by sitting up and leaning forward, paradoxical pericardial friction rub, high-pitched leathery/scratchy heart sounds best heard in a sitting position at the lower left sternal border.
- Investigations: ECG (global ST elevation, followed by Spodick's sign: TP segment depression), CXR (possible pericardial effusion), Echo (to rule out cardiac tamponade).
- Management: aspirin, NSAIDs, colchicine, bed rest, steroids.
Jugular Venous Pulse (JVP)
- A window to the right heart, allowing for a non-invasive assessment of right atrial pressure.
- Indicator of right heart hemodynamics, volume of blood in the venous system, venous tone.
- Right Internal Jugular Vein (IJV) is the preferred vessel used to visualize JVP.
- IJV is located in the carotid triangle, between the sternal and clavicular head of the sternocleidomastoid muscle.
- IJV is lateral to the carotid artery and deep to the sternocleidomastoid muscle.
- IJV is in a straight line with the right atrium (RA) and is less likely to be affected by extrinsic compression.
Brachiofemoral Delay
- Normal Delay:
- Carotid: 30 ms
- Brachial: 60 ms
- Radial: 80 ms
- Femoral: 75 ms
- Exaggerated Delay: Coarctation of aorta.
Pathophysiology of Cardiac Tamponade
- Characterized by rapid accumulation of fluid, leading to:
- Increased pericardial pressure.
- Exaggerated interventricular dependence (Pulsus paradoxus).
- Hemodynamic changes: Holodiastolic elevation & equalization of diastolic pressure in all 4 chambers.
- LV Compression: ↓ BP, Obstructive shock, Dyspnoea, Tachycardia.
- JVP: Sharp, rapid, prominent x descent and absent y descent.
- Beck's triad: Hypotension, prominent JVP, muffled heart sounds.
- ECG: Alternating high & low volume complexes (Electrical alternans).
- Treatment: Immediate pericardiocentesis.
Complications: Repeated attacks Lead to MI vs Pericarditis
- Pericarditis: sharp, stabbing chest pain, worsened with inspiration, worse when supine, improved when sitting up or leaning forward, lasts for hours to days, no change with nitroglycerin, friction rub present in most patients, ECG shows widespread concave ST segment elevation and frequent PR segment depression.
- Myocardial Ischemia or Infarction: pressure-like heavy, squeezing chest pain, no change with respiration or position, lasts for minutes (ischemia), hours (infarction), improved with nitroglycerin, friction rub absent, ECG shows localized convex ST segment elevation and rare PR segment depression.
Dressler's Syndrome
- Etiology: >2-6 wks post MI, autoimmune.
- Clinical Features: Fever + pleuritic pain + polyserositis, pericardial rub (+).
- ECG: (N) or features of acute pericarditis.
- Rx: NSAIDS.
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.