Podcast
Questions and Answers
What is the primary consequence when interstitial fluid pressure exceeds approximately 2 mmHg?
What is the primary consequence when interstitial fluid pressure exceeds approximately 2 mmHg?
- Decreased lymphatic flow
- Edema formation (correct)
- Increased blood pressure
- Enhanced reabsorption in capillaries
Which of the following is NOT a factor responsible for lymphatic pumping?
Which of the following is NOT a factor responsible for lymphatic pumping?
- External compression
- Skeletal muscle contraction
- Contraction of lymph vessel walls
- Increased interstitial fluid pressure (correct)
Which condition is primarily associated with increased fluid filtration leading to edema?
Which condition is primarily associated with increased fluid filtration leading to edema?
- Blood clot formation
- Heart failure
- Histamine release (correct)
- Mastectomy
What is the mechanism by which pitting edema differs from non-pitting edema?
What is the mechanism by which pitting edema differs from non-pitting edema?
What physiological event occurs when the smooth muscle in lymphatic vessels is stretched?
What physiological event occurs when the smooth muscle in lymphatic vessels is stretched?
Which of the following clinical examples does NOT represent decreased fluid reabsorption?
Which of the following clinical examples does NOT represent decreased fluid reabsorption?
Which situation could contribute to the development of edema due to decreased lymphatic flow?
Which situation could contribute to the development of edema due to decreased lymphatic flow?
In which scenario does increased vascular permeability most likely lead to edema?
In which scenario does increased vascular permeability most likely lead to edema?
What is the primary characteristic that defines pitting edema?
What is the primary characteristic that defines pitting edema?
How does the distensibility of veins compare to that of arteries?
How does the distensibility of veins compare to that of arteries?
What effect do small changes in blood volume have on arterial pressure?
What effect do small changes in blood volume have on arterial pressure?
During diastole, what is the primary function of aortic recoil?
During diastole, what is the primary function of aortic recoil?
What anatomical feature of veins contributes to their higher distensibility compared to arteries?
What anatomical feature of veins contributes to their higher distensibility compared to arteries?
Which of the following accurately describes the distribution of blood volume in the body?
Which of the following accurately describes the distribution of blood volume in the body?
When there is an increase in blood volume, how does this impact venous pressure?
When there is an increase in blood volume, how does this impact venous pressure?
What occurs in the arterial system when the volume of blood is significantly increased?
What occurs in the arterial system when the volume of blood is significantly increased?
What role does the elastic recoil of the aorta play in the cardiovascular system?
What role does the elastic recoil of the aorta play in the cardiovascular system?
How is pulse pressure defined?
How is pulse pressure defined?
Which condition is indicated by a high pulse pressure?
Which condition is indicated by a high pulse pressure?
Which factor is MOST likely to lead to a low pulse pressure?
Which factor is MOST likely to lead to a low pulse pressure?
What is the effect of increased stroke volume on pulse pressure?
What is the effect of increased stroke volume on pulse pressure?
If a person's blood pressure is 140/80 mmHg, what is their pulse pressure?
If a person's blood pressure is 140/80 mmHg, what is their pulse pressure?
How does noncompliance of the arterial tree influence pulse pressure?
How does noncompliance of the arterial tree influence pulse pressure?
What could a thready pulse indicate in a clinical scenario?
What could a thready pulse indicate in a clinical scenario?
What percentage of the fluid filtered from capillaries is typically reabsorbed back into capillaries?
What percentage of the fluid filtered from capillaries is typically reabsorbed back into capillaries?
Which substance has the most significant effect on oncotic pressure in blood?
Which substance has the most significant effect on oncotic pressure in blood?
How does fluid move from the interstitial compartment into the intracellular compartment?
How does fluid move from the interstitial compartment into the intracellular compartment?
Which of the following best describes the role of plasma proteins in fluid movement?
Which of the following best describes the role of plasma proteins in fluid movement?
What is the fate of the remaining 10% of the fluid that is filtered out of capillaries?
What is the fate of the remaining 10% of the fluid that is filtered out of capillaries?
Which statement is true regarding the influence of electrolytes on fluid movement?
Which statement is true regarding the influence of electrolytes on fluid movement?
What happens to fluid movement when there is liver dysfunction affecting albumin levels?
What happens to fluid movement when there is liver dysfunction affecting albumin levels?
Which of the following statements about Starling's forces is incorrect?
Which of the following statements about Starling's forces is incorrect?
What is the reason for the higher plasma colloid osmotic pressure at the venous end of the capillary?
What is the reason for the higher plasma colloid osmotic pressure at the venous end of the capillary?
What effect does increased arterial pressure have on net filtration?
What effect does increased arterial pressure have on net filtration?
How does increased venous pressure affect fluid movement in the capillaries?
How does increased venous pressure affect fluid movement in the capillaries?
What percentage of fluid filtered out at the arterial end of the capillaries is typically reabsorbed at the venous end?
What percentage of fluid filtered out at the arterial end of the capillaries is typically reabsorbed at the venous end?
What happens to interstitial fluid pressure when fluid is pushed out of the capillaries?
What happens to interstitial fluid pressure when fluid is pushed out of the capillaries?
Which of the following best describes the fluid dynamics at the venous end of a capillary?
Which of the following best describes the fluid dynamics at the venous end of a capillary?
What is the main consequence of filtration exceeding reabsorption in the capillary system?
What is the main consequence of filtration exceeding reabsorption in the capillary system?
What role do proteins play in plasma colloid osmotic pressure at the venous end of the capillary?
What role do proteins play in plasma colloid osmotic pressure at the venous end of the capillary?
Flashcards are hidden until you start studying
Study Notes
Pulse Pressure
- Pulse pressure is the difference between systolic and diastolic blood pressure (SBP - DBP)
- A high pulse pressure (bounding pulse) can indicate a large difference between systolic and diastolic pressure, but doesn't specify the reason.
- Examples include a healthy exercise blood pressure, hypertension, or a normal systolic pressure with a low diastolic pressure.
- A low pulse pressure (thready pulse) is often due to a low systolic pressure. It also doesn't indicate the reason, similar to a bounding pulse.
Factors Affecting Arterial Pulse Pressure
- Stroke volume: Higher stroke volume leads to greater pressure fluctuations.
- Stroke volume is influenced by cardiac contractility and afterload.
- Compliance of the arterial tree: Low compliance (stiffness) increases arterial pressure.
Fluid Movement Between Compartments
- Vascular and Interstitial: Fluid (water and electrolytes) is filtered from capillaries into the interstitial fluid and reabsorbed back into the capillaries.
- About 90% of the filtered fluid is reabsorbed, with the remaining 10% returning via lymphatic vessels.
- Starling's forces govern this movement. Electrolytes don't significantly influence fluid movement between these compartments.
- Interstitial and Intracellular: Fluid and electrolytes move across interstitial fluid and cell membranes via channels and transporters.
- Electrolyte concentration gradient influences the direction of movement.
- Water movement is dependent on cell osmolarity.
Fluid Filtration
- Plasma Proteins: Plasma proteins contribute to osmotic (oncotic) pressure.
- They don't diffuse through capillaries, creating a "pulling" force that draws fluid from the interstitium back into the plasma.
- Albumin accounts for 80% of colloid osmotic pressure.
- Starling Forces: Four forces govern fluid movement:
- Capillary hydrostatic pressure (pushes fluid out)
- Interstitial hydrostatic pressure (pushes fluid in)
- Capillary osmotic pressure (pulls fluid in)
- Interstitial osmotic pressure (pulls fluid out)
- Capillary Hydrostatic Pressure and Filtration: Increased arterial pressure leads to increased capillary hydrostatic pressure and greater filtration.
- Venous Pressure and Reabsorption: Increased venous pressure reduces fluid reabsorption and increases net filtration.
- Lymphatic Circulation: Under normal conditions, approximately 90% of filtered fluid is reabsorbed at the venous end of the capillaries, with the remaining 10% entering the lymphatic system for circulation.
Lymphatic System
- Lymph Flow: Increased interstitial fluid volume raises interstitial pressure, leading to higher lymph flow until the lymphatic system reaches its maximum capacity.
- Excess fluid accumulation results in edema.
- Lymphatic Pumping: Lymphatic pumping mechanisms include:
- Contraction of lymph vessel walls (smooth muscle)
- Rhythmic compression of lymphatic vessels (skeletal muscle contraction, movement, arterial pulsation, external compression)
Edema
- Causes: Extracellular edema can be caused by:
- Increased fluid filtration: Increased vascular permeability due to factors like histamine release, inflammation, or capillary damage.
- Decreased fluid reabsorption: Increased venous resistance (blood clots, heart failure, external compression) or slowed/stopped lymphatic flow (tumor blockage, surgery, parasitic infections).
- Pitting vs Non-pitting Edema:
- Pitting edema: Excess interstitial fluid accumulates, causing the gel-like structure of the interstitium to transform into free fluid.
- Non-pitting edema: Fluid remains bound to the interstitial matrix, resulting in a solid-like consistency.
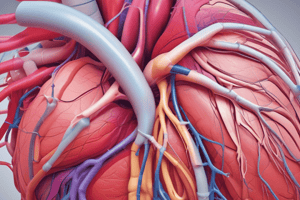
Vascular Function
- Distensibility Differences: Arteries/arterioles have thicker smooth muscle layers than veins/venules.
- This makes veins more distensible than arteries, allowing them to expand more for a given pressure.
- Veins serve as blood reservoirs.
- Volume and Pressure Relationship:
- Arterial system: Small changes in volume significantly affect pressure.
- Venous system: Large changes in volume have a minimal effect on pressure.
- Aortic Distensibility and Circulation: The aorta stretches during systole to accommodate blood.
- During diastole, the aorta recoils, creating an inward pressure that drives blood forward throughout the systemic circulation.
- The aortic valve prevents blood from backflow into the heart.
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.