Podcast
Questions and Answers
What physiological response occurs to maintain a constant Mean Arterial Pressure (MAP) when cardiac output decreases?
What physiological response occurs to maintain a constant Mean Arterial Pressure (MAP) when cardiac output decreases?
- End-diastolic volume decreases dramatically
- Total Peripheral Resistance must increase (correct)
- Heart rate must decrease to balance the system
- Vasodilation decreases Total Peripheral Resistance (TPR)
How does the body primarily regulate blood pressure during exercise?
How does the body primarily regulate blood pressure during exercise?
- By maintaining constant blood volume
- By increasing heart rate alone
- By adjusting vessel diameter to change resistance (correct)
- By decreasing stroke volume
In terms of myocardial oxygen utilization during exercise, what primarily influences the heart's energy needs?
In terms of myocardial oxygen utilization during exercise, what primarily influences the heart's energy needs?
- Total Peripheral Resistance alone
- Vasodilation of coronary vessels
- Only heart rate changes
- Cardiac Output and stroke volume (correct)
What is the effect of arterioles relaxing on blood flow and blood pressure?
What is the effect of arterioles relaxing on blood flow and blood pressure?
What happens to Total Peripheral Resistance when there is an increase in stroke volume during exercise?
What happens to Total Peripheral Resistance when there is an increase in stroke volume during exercise?
With respect to the Rate Pressure Product, which factor would most likely increase it during intense physical activity?
With respect to the Rate Pressure Product, which factor would most likely increase it during intense physical activity?
What role does vasoconstriction play in blood pressure regulation?
What role does vasoconstriction play in blood pressure regulation?
How does body position affect cardiovascular response during upper body versus lower body exercise?
How does body position affect cardiovascular response during upper body versus lower body exercise?
What is the role of baroreceptors in blood pressure regulation during standing?
What is the role of baroreceptors in blood pressure regulation during standing?
How does resistance training primarily affect myocardial oxygen utilization compared to aerobic exercises?
How does resistance training primarily affect myocardial oxygen utilization compared to aerobic exercises?
What primarily differentiates blood pressure responses in upper body versus lower body exercises?
What primarily differentiates blood pressure responses in upper body versus lower body exercises?
What physiological changes characterize hypotensive recovery after intense exercise?
What physiological changes characterize hypotensive recovery after intense exercise?
How is Rate Pressure Product (RPP) affected during exercise?
How is Rate Pressure Product (RPP) affected during exercise?
How does increased stroke volume affect mean arterial pressure (MAP)?
How does increased stroke volume affect mean arterial pressure (MAP)?
What is the primary reason that the blood pressure gradient decreases from arteries to veins?
What is the primary reason that the blood pressure gradient decreases from arteries to veins?
During exercise, how is myocardial oxygen utilization primarily affected?
During exercise, how is myocardial oxygen utilization primarily affected?
Which of the following describes the hypotensive recovery response after exercise?
Which of the following describes the hypotensive recovery response after exercise?
What is the significance of the Rate Pressure Product (RPP) during physical exertion?
What is the significance of the Rate Pressure Product (RPP) during physical exertion?
Which of the following factors contributing to arterial blood pressure is least affected by exercise?
Which of the following factors contributing to arterial blood pressure is least affected by exercise?
In terms of blood pressure response, what distinguishes upper body exercise from lower body exercise?
In terms of blood pressure response, what distinguishes upper body exercise from lower body exercise?
What physiological response is most likely to occur during isovolumetric contraction?
What physiological response is most likely to occur during isovolumetric contraction?
How does blood viscosity influence mean arterial pressure in the context of increased exercise intensity?
How does blood viscosity influence mean arterial pressure in the context of increased exercise intensity?
What potential complication can venous pooling cause during prolonged inactivity or after intense exercise?
What potential complication can venous pooling cause during prolonged inactivity or after intense exercise?
What is the physiological response of the heart during vigorous exercise in terms of coronary blood flow?
What is the physiological response of the heart during vigorous exercise in terms of coronary blood flow?
What is the primary determinant of the Rate Pressure Product (RPP)?
What is the primary determinant of the Rate Pressure Product (RPP)?
How does sympathetic stimulation affect heart rate during exercise?
How does sympathetic stimulation affect heart rate during exercise?
What is the most accurate relationship between myocardial oxygen utilization at rest compared to other tissues?
What is the most accurate relationship between myocardial oxygen utilization at rest compared to other tissues?
During the recovery phase after exercise, which mechanism is primarily responsible for returning heart rate to baseline levels?
During the recovery phase after exercise, which mechanism is primarily responsible for returning heart rate to baseline levels?
Which process is primarily activated to supply adequate oxygen to the myocardium during high-intensity exercise?
Which process is primarily activated to supply adequate oxygen to the myocardium during high-intensity exercise?
What condition arises when blood flow to coronary muscles is compromised?
What condition arises when blood flow to coronary muscles is compromised?
What is the heart rate change range during intense exercise due to extrinsic control?
What is the heart rate change range during intense exercise due to extrinsic control?
Which of the following areas of the heart has the slowest intrinsic rhythm for initiating heart contractions?
Which of the following areas of the heart has the slowest intrinsic rhythm for initiating heart contractions?
During exercise, what immediate cardiovascular change is expected due to anticipatory responses?
During exercise, what immediate cardiovascular change is expected due to anticipatory responses?
What happens to systemic vascular resistance (SVR) during graded exercise as intensity increases?
What happens to systemic vascular resistance (SVR) during graded exercise as intensity increases?
How does upper body exercise compare to lower body exercise in terms of physiological strain?
How does upper body exercise compare to lower body exercise in terms of physiological strain?
What is the effect of maximal exercise on systolic blood pressure (SBP) in individuals with a high aerobic capacity?
What is the effect of maximal exercise on systolic blood pressure (SBP) in individuals with a high aerobic capacity?
What physiological response typically occurs during the hypotensive recovery phase after exercise?
What physiological response typically occurs during the hypotensive recovery phase after exercise?
In the context of myocardial oxygen utilization, how does lower body exercise compare to upper body exercise at maximal effort?
In the context of myocardial oxygen utilization, how does lower body exercise compare to upper body exercise at maximal effort?
Which statement about blood pressure response to resistance exercise is true?
Which statement about blood pressure response to resistance exercise is true?
What defines the Rate Pressure Product (RPP) during exercise?
What defines the Rate Pressure Product (RPP) during exercise?
During steady-rate exercise, what is the primary reason for the initial increase in systolic blood pressure (SBP)?
During steady-rate exercise, what is the primary reason for the initial increase in systolic blood pressure (SBP)?
What best defines Total Peripheral Resistance (TPR) at rest with given values of DBP, SBP, and CO?
What best defines Total Peripheral Resistance (TPR) at rest with given values of DBP, SBP, and CO?
What is the primary function of the cardiovascular system?
What is the primary function of the cardiovascular system?
Which of the following describes systemic circulation?
Which of the following describes systemic circulation?
What type of muscle is primarily responsible for heart contraction?
What type of muscle is primarily responsible for heart contraction?
What is the term for the volume of blood in the heart at rest?
What is the term for the volume of blood in the heart at rest?
Which type of valves are the tricuspid and bicuspid valves classified as?
Which type of valves are the tricuspid and bicuspid valves classified as?
What is the brief period called when all heart valves are shut and the ventricular volume remains the same?
What is the brief period called when all heart valves are shut and the ventricular volume remains the same?
What characteristic differentiates cardiac muscle fibers from skeletal muscle fibers?
What characteristic differentiates cardiac muscle fibers from skeletal muscle fibers?
Which circulation has a higher pressure, systemic or pulmonary?
Which circulation has a higher pressure, systemic or pulmonary?
Which of the following statements accurately describes the role of arteries in the circulatory system?
Which of the following statements accurately describes the role of arteries in the circulatory system?
What distinguishes the pulmonary circulation from systemic circulation?
What distinguishes the pulmonary circulation from systemic circulation?
What is the term for the volume of blood present in the heart at the end of diastole?
What is the term for the volume of blood present in the heart at the end of diastole?
In which phase of the heart cycle do all heart valves remain closed while ventricular pressure rises?
In which phase of the heart cycle do all heart valves remain closed while ventricular pressure rises?
Which type of muscle fibers are found in cardiac muscle?
Which type of muscle fibers are found in cardiac muscle?
What characterizes the stroke volume, calculated by the formula EDV - ESV?
What characterizes the stroke volume, calculated by the formula EDV - ESV?
Which of the following describes the function of the atrioventricular valves?
Which of the following describes the function of the atrioventricular valves?
What type of muscle control is characterized as involuntary in the heart?
What type of muscle control is characterized as involuntary in the heart?
What is the main difference in pressure between systemic circulation and pulmonary circulation?
What is the main difference in pressure between systemic circulation and pulmonary circulation?
Which structural feature is unique to cardiac muscle compared to skeletal muscle?
Which structural feature is unique to cardiac muscle compared to skeletal muscle?
Flashcards are hidden until you start studying
Study Notes
Mean Arterial Pressure (MAP)
- MAP is the average pressure in the arteries during one cardiac cycle, calculated as: MAP = DBP + [⅓(SBP-DBP)]
- MAP is the perfusion pressure of organs; insufficient blood flow can lead to ischemia if MAP is below 60 mmHg for a long period.
- The body can adjust resistance at the ends of vessels to maintain a constant MAP.
- If cardiac output decreases, total peripheral resistance (TPR) must increase to maintain MAP.
Total Peripheral Resistance (TPR)
- Blood vessel diameter is used to regulate blood pressure.
- Nerves control the muscles that cause vessels to contract (vasoconstriction) or dilate (vasodilation).
- TPR is influenced by vessel diameter, length, and viscosity.
- Vessel length remains constant after adulthood; changes in TPR are primarily due to changes in vessel diameter.
Cardiac Output (CO)
- The amount of blood ejected by one ventricle in one minute.
- At rest, CO is approximately 5 L/min.
- CO can be increased by increasing heart rate (HR), stroke volume (SV), or both.
- Increased CO leads to increased MAP.
Steady Rate Exercise
- During the first few minutes of exercise, increased blood flow (CO) rapidly increases systolic blood pressure (SBP).
- Vasodilation in active muscles decreases TPR, increasing blood flow to the peripheral vasculature.
- As exercise continues, SBP gradually decreases due to continued vasodilation and decreased TPR.
- Muscle contraction and relaxation enhance venous return.
Graded Exercise
- SBP increases rapidly at the start of exercise and increases linearly with exercise intensity.
- Diastolic blood pressure (DBP) may remain unchanged or decrease slightly.
- Maximum SBP may exceed 200 mmHg despite reduced TPR.
- This high SBP reflects the heart's increased CO during maximal exercise in individuals with high aerobic capacity.
Blood Pressure Response to Resistance Exercise
- Concentric contractions compress peripheral vasculature, increasing resistance.
- The magnitude of increase in SBP is related to exercise intensity and muscle mass used.
Submaximal Upper Body Exercise (UBE)
- UBE requires greater oxygen consumption than lower body exercise at any submaximal power output due to lower mechanical efficiency, recruitment of stabilizing muscles, and greater physiological strain.
- UBE leads to higher heart rate (HR), ventilation (Ve), blood pressure (BP), and ratings of perceived exertion (RPE).
Maximal Upper Body Exercise
- VO2 values are typically 20-30% lower than lower body exercise.
- Lower maximum HR and pulmonary ventilation due to smaller musculature activated.
Hypotensive Recovery Response
- SBP temporarily decreases below pre-exercise levels for up to 12 hours after sustained light to moderate exercise in both normal and hypertensive individuals.
- This is due to blood pooling in skeletal muscle vascular beds during recovery.
Clinical Significance of Exaggerated BP Response
- Increased risk for hypertension, cardiovascular mortality, and cardiovascular events.
- Presence of cardiac hypertrophy.
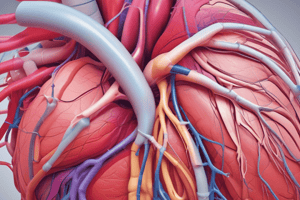
The Heart's Blood Supply
- The heart chambers do not receive nutrients from the blood they contain.
- Coronary circulation supplies the heart muscle with approximately 5% (250ml) of total cardiac output.
- Right and left coronary arteries originate from the aorta behind the aortic valve and divide into dense capillary networks that feed the myocardium.
- Coronary sinus and anterior cardiac veins collect blood and empty directly into the right atrium.
Myocardial Oxygen Utilization
- At rest, the myocardium extracts 70-80% of the oxygen from the blood flowing in coronary vessels.
- During vigorous exercise, coronary blood flow increases 4-6 times above resting levels.
- Impaired coronary blood supply causes chest pain (angina pectoris).
Impaired Coronary Blood Supply
- Coronary muscle is purely aerobic.
- Exercise increases energy requirements, making it a diagnostic tool for myocardial ischemia.
- A blood clot in the coronary vessels can result in myocardial infarction.
- Ischemia: Restriction in blood supply to tissues.
- Hypoxia: A region of the body is deprived of adequate oxygen supply.
- Infarction: Tissue death caused by a local lack of oxygen.
Rate Pressure Product (RPP)
- Provides a non-invasive estimation of myocardial workload (myocardial oxygen uptake).
- RPP = SBP x HR.
- RPP has a linear relationship with exercise intensity.
- Chronic exposure to higher myocardial workload can lead to cardiac hypertrophy.
Cardiovascular Regulation and Integration
- Cardiac muscle is autorhythmic, meaning it can maintain its own rhythm (heart rate).
- The intrinsic heart rate is approximately 100 BPM.
- Extrinsic control via neurohumoral factors can adjust heart rate from 40 BPM at rest to 220 BPM at peak exercise.
Autorhythmic/Automaticity
- The heart can beat independently without exogenous commands.
Intrinsic Regulation of Heart Rate
- Heart rate originates in the sinoatrial (SA) node, propagating outwards.
- The SA node initiates depolarization, which travels through the atrioventricular (AV) node to the Purkinje fibers and bundle of HIS.
- The signal then travels up the walls of the ventricle.
- The AV node delays the electrical signal for 0.10 seconds, allowing atrial contraction before ventricular filling.
- Ventricular contraction occurs 0.06 seconds after stimulation.
Electrocardiogram (ECG/EKG)
- Records the electrical activity of the heart.
- P-wave: Atrial depolarization.
- QRS complex: Ventricular depolarization and atrial repolarization occurring simultaneously.
- T-wave: Ventricular repolarization.
- ECG abnormalities can indicate coronary heart disease.
Relationship Between Pressure Changes and ECG
- Atrial depolarization leads to atrial contraction, a slight increase in blood volume, and a minimal increase in ventricular pressure.
- Ventricular depolarization leads to ventricular contraction, generating maximum pressure, and signaling ventricular repolarization.
Areas of the Heart that can Initiate a Rhythm and Intrinsic Rate
- Sinus node: 60-100 BPM.
- Atrial tissue: 60-100 BPM.
- AV node: 40-60 BPM.
- Ventricular tissue: 20-40 BPM.
Extrinsic Heart Rate Regulation
- Neural influences superimpose on the inherent rhythm of the myocardium.
- This regulation adjusts heart rate in anticipation of exercise and as exercise intensity changes.
- The range of heart rate regulated by neural influences is 20-200 BPM (dependent on physical fitness).
Sympathetic and Parasympathetic Control
- Sympathetic stimulation: - Catecholamines (NE/Epinephrine). - Results in tachycardia (increased heart rate). - Increases SA node depolarization. - Enhances contractility.
- Parasympathetic influence: - Acetylcholine (vagal influence). - Results in bradycardia (decreased heart rate). - Slows SA node depolarization.
Exercise and Blood Flow
- Parasympathetic Neural Control:
- Peripheral effects include excitation of the iris, gallbladder, and coronary arteries.
- Inhibition of gut sphincters, intestines, and skin vasculature.
- During the onset of exercise, heart rate increases by inhibiting the parasympathetic nervous system (PNS).
Sympathetic Control on Blood Flow
- Mechanism involves NE via adrenergic fibers located in the smooth muscles of small arteries, arterioles, and precapillary sphincters.
- Inactive tissue (vasoconstriction):
- Renal, splanchnic, and inactive skeletal muscle.
- Produces systemic vasoconstriction of inactive muscle.
- Active tissue (vasodilation):
- Active muscle.
- Decreases sympathetic nervous system (SNS) activity.
Neural Response During Exercise
- Anticipatory response:
- Decreased parasympathetic activity.
- Increased sympathetic activity.
- Exercise: - Parasympathetic inhibition (early). - Sympathetic stimulation (more intense).
- Results: - Increased heart rate and contractility. - Increased arterial blood pressure. - Vasodilation of active skeletal muscles. - Vasoconstriction of skin, gut, spleen, etc. - Vasoconstriction increases venous return.
Functional Sympatholysis
- Sympathetic neural activity normally causes vasoconstriction.
- Local changes in muscle metabolites and other substances reduce vascular responsiveness to alpha-adrenergic receptor activation, allowing for vasodilation in active tissues.
Peripheral Input Control of CV Response
- The initial signal for cardiovascular system activation originates in higher brain centers.
- This signal is fine-tuned by feedback from:
- Chemoreceptors (sensitive to blood oxygen, carbon dioxide, and pH levels).
- Baroreceptors (sensitive to changes in arterial blood pressure).
- Muscle mechanoreceptors (heart, skin, joints; sensitive to force and speed of muscle movement).
- Metaboreflex muscle chemoreceptors (sensitive to muscle metabolites like potassium and lactic acid).
BP Response to Standing
- Gravity-induced drop in BP due to blood pooling in the legs is detected by baroreceptors in the carotid arteries and aorta.
- Baroreceptors signal the brain, activating the sympathetic nervous system.
- This increases heart rate, contractility, and cardiac output.
- Blood vessels constrict via alpha-1 receptors to increase blood volume.
Baroreceptors
- Located in the aortic arch and common carotid arteries.
- When blood pressure is too high:
- Baroreceptors are stimulated and signal the brain.
- The cardioacceleratory center is inhibited, and the cardioinhibitory center is stimulated.
- This decreases heart rate, cardiac output, and vasoconstriction.
- Arterial vasodilation occurs, reducing blood pressure.
Chemoreceptors
- Sensitive to oxygen, carbon dioxide, and pH levels.
- When homeostasis is disturbed (decreased oxygen and pH, increased carbon dioxide):
- Chemoreceptors are stimulated and signal reflex responses.
- The cardioinhibitory center is inhibited, and the cardioacceleratory center is stimulated.
- Cardiac output increases.
- The respiratory center is stimulated, increasing respiratory rate.
Blood Flow Regulation
- Blood Flow = Pressure x Resistance.
- TPR is influenced by physical characteristics of the blood (viscosity) and the size of individual vessels (length and diameter).
Poiseuille’s Law
- Quantifies blood flow resistance.
- Flow = pressure gradient x vessel radius^4 / vessel length x viscosity.
- Vessel diameter is the most significant factor in influencing blood flow resistance.
- Vessel length and blood viscosity have less of an impact because they remain relatively constant.
Exercise and Blood Flow
- Nerve and local metabolites cause dilation of arterioles in active muscle beds.
- Vasoconstriction in visceral organs and the muscle pump bring blood to central circulation.
- Example:
- Kidneys:
- Rest = 1100 ml/minute (20% of CO).
- Exercise = 250 ml/minute (1% of CO).
- Kidneys:
Active Muscle
- At rest, only 1 out of 40 capillaries in active muscle are open.
- Opening dormant capillaries during exercise:
- Increases muscle blood flow.
- Allows for a large blood volume with minimal increase in blood flow velocity.
- Increases the surface area for gas and nutrient exchange between blood and muscle fibers.
- Local factors (autoregulatory mechanisms) involved in capillary opening:
- Decreased pH, increased PCO2, increased ADP, increased Ca++, increased temperature.
Key Functions of the Cardiovascular System
- Delivers oxygen and nutrients to active tissues.
- Returns deoxygenated blood to the lungs.
- Transports heat (byproduct of cellular metabolism) and hormones.
Circulatory System
- Also known as Cardiovascular System.
- The heart functions as a dual pump.
- Two blood flow circuits exist:
- Systemic circulation: Circulates blood between the heart and the body (excluding the lungs).
- Pulmonary circulation: Circulates blood between the heart and the lungs.
- Some differences between the circuits:
- Pulmonary circuit blood flow travels shorter distances.
- Systemic circulation has higher pressure.
- Arteries carry blood away from the heart, but this blood may not always be oxygenated.
- Systemic circulation is responsible for carrying oxygenated blood away from the heart towards the body and returning deoxygenated blood back to the heart.
Heart Cell Types
- Two types of cells exist in the heart:
- Electrical cells: Responsible for conducting electrical signals.
- Contractile cells: Responsible for the mechanical contraction of the heart.
Heart Structure and Function
- Skeletal muscle:
- Striated, tubular fibers containing multiple nuclei.
- Voluntary control (consciously controlled).
- Usually attached to the skeleton.
- Cardiac muscle:
- Striated, branched fibers with only one nucleus per fiber.
- Involuntary control (not consciously controlled).
- Found solely within the heart walls.
Anatomy of the Heart
- Four chambers:
- Right atrium: Receives deoxygenated blood from the body.
- Right ventricle: Pumps deoxygenated blood to the lungs.
- Left atrium: Receives oxygenated blood from the lungs.
- Left ventricle: Pumps oxygenated blood to the body.
- Four valves:
- Atrioventricular valves:
- Tricuspid (right): Controls blood flow between the right atrium and right ventricle.
- Bicuspid/mitral (left): Controls blood flow between the left atrium and the left ventricle.
- Semilunar valves:
- Pulmonary: Prevents blood from flowing back into the right ventricle from the pulmonary artery.
- Aortic: Prevents blood from flowing back into the left ventricle from the aorta.
- Atrioventricular valves:
Terms and Definitions for Heart Contraction
- Diastole: The resting phase of the heart.
- End Diastolic Volume (EDV): The volume of blood in the heart during diastole (rest).
- Systole: The contracting phase of the heart.
- End Systolic Volume (ESV): The volume of blood remaining in the heart after contraction.
- Stroke Volume (SV): The amount of blood ejected with each heartbeat (calculated as EDV-ESV).
- Isovolumetric: Refers to a period of constant volume.
- Isovolumetric contraction: A brief period (0.02-0.06 seconds) during which all four heart valves are closed, and ventricular pressure rises rapidly.
Key Functions of the Cardiovascular System
- Delivers oxygen and nutrients to active tissues.
- Returns deoxygenated blood to the lungs
- Transports heat (byproduct of cellular metabolism) and hormones.
Circulatory System
- Also known as the Cardiovascular system.
- The heart acts as a dual pump.
- Consists of two blood flow circuits:
- Systemic Circulation: Heart and system; includes all parts of the body besides the lungs.
- Pulmonary Circulation: Heart and lungs.
- The blood flow in the pulmonary circuit is shorter than in the systemic circuit, so the blood doesn't need to travel as far.
- Systemic circulation has higher pressure compared to pulmonary circulation.
- Arteries carry blood away from the heart but may not always be oxygenated.
- Systemic circulation carries oxygenated blood away from the heart to the body and returns deoxygenated blood back to the heart.
Heart Cell Types
- Two types of cells in the heart:
- Electrical: Responsible for the electrical pathway in the heart.
- Contractile: Responsible for the mechanical function (contractions) of the Heart.
Cardiac Muscle
- Cardiac muscle has striations, branches, and is uninucleated.
- It is involuntary and only covers the walls of the heart.
- Unlike skeletal muscle, which is voluntary, striated, tubular, and multinucleated while also being attached to the skeleton, cardiac muscle is involuntary.
Anatomy of the Heart
- Consists of four chambers:
- Right Atrium
- Right Ventricle
- Left Atrium
- Left Ventricle
- Consists of four valves:
- Atrioventricular Valves:
- Tricuspid (Right)
- Bicuspid/Mitral (Left)
- Semilunar Valves:
- Pulmonary
- Aortic
- Atrioventricular Valves:
Terms and Definitions for Heart Contraction
- Diastole: The resting phase of the heart.
- End Diastolic Volume (EDV): Volume of blood in the heart during diastole (rest).
- Systole: The contraction phase of the heart.
- End Systolic Volume (ESV): Volume of blood in the heart during systole (contraction).
- Stroke Volume (SV): The amount of blood ejected with each heartbeat. Calculated as EDV - ESV.
- Isovolumetric: Means "same volume"
- Isovolumetric Contraction: A brief period (0.02-0.06 seconds) when all heart valves remain closed, and ventricular pressure rises, resulting in the first heart sound.
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.