Podcast
Questions and Answers
Why is it important for a physical therapist to identify heart sounds during a cardiovascular assessment?
Why is it important for a physical therapist to identify heart sounds during a cardiovascular assessment?
- To measure the patient's body mass index.
- To identify potential valve abnormalities or heart dysfunction. (correct)
- To assess the patient's skin integrity.
- To determine the patient's level of consciousness.
In what position should a patient be placed to best auscultate heart sounds?
In what position should a patient be placed to best auscultate heart sounds?
- Standing with arms at their side.
- Supine or semi-Fowler's position. (correct)
- Seated, leaning forward.
- Prone with head turned to the side.
When reviewing a patient’s medical chart, what aspects related to cardiovascular health should a physical therapist prioritize?
When reviewing a patient’s medical chart, what aspects related to cardiovascular health should a physical therapist prioritize?
- History of childhood illnesses and vaccinations.
- Dietary preferences and restrictions.
- Patient's preferred recreational activities and hobbies.
- Diagnosis, medications, and special tests performed. (correct)
During a patient interview, what type of questions should a physical therapist avoid to prevent leading the patient to provide biased answers?
During a patient interview, what type of questions should a physical therapist avoid to prevent leading the patient to provide biased answers?
During a physical examination, what observation indicates the use of accessory muscles for respiration?
During a physical examination, what observation indicates the use of accessory muscles for respiration?
What does jugular venous distention (JVD) typically indicate?
What does jugular venous distention (JVD) typically indicate?
When auscultating heart sounds, which side of the stethoscope is best suited for detecting high-pitched sounds like S1 and S2.
When auscultating heart sounds, which side of the stethoscope is best suited for detecting high-pitched sounds like S1 and S2.
What is the physiological cause of normal heart sounds?
What is the physiological cause of normal heart sounds?
Where is S1 typically loudest during auscultation?
Where is S1 typically loudest during auscultation?
What cardiac condition is often associated with a loud S2 heart sound?
What cardiac condition is often associated with a loud S2 heart sound?
An S3 heart sound is typically indicative of:
An S3 heart sound is typically indicative of:
What is typically used to describe heart murmurs?
What is typically used to describe heart murmurs?
What is a common cause of heart murmurs?
What is a common cause of heart murmurs?
In auscultation, where is the recommended location to best hear aortic valve sounds?
In auscultation, where is the recommended location to best hear aortic valve sounds?
What skin-related changes are relevant in a cardiovascular assessment?
What skin-related changes are relevant in a cardiovascular assessment?
What does central cyanosis typically indicate?
What does central cyanosis typically indicate?
What is the clinical significance of pitting edema in a patient with cardiovascular issues?
What is the clinical significance of pitting edema in a patient with cardiovascular issues?
You are assessing a patient and notice a significant amount of edema. When pressing on the skin you notice a ~6mm indentation that takes about 20 seconds to disappear. How would you grade this edema?
You are assessing a patient and notice a significant amount of edema. When pressing on the skin you notice a ~6mm indentation that takes about 20 seconds to disappear. How would you grade this edema?
Where should you palpate to locate the dorsalis pedis pulse?
Where should you palpate to locate the dorsalis pedis pulse?
A therapist assesses a patient's pulse and assigns a grade of '1+'. What does this indicate about the pulse's characteristics?
A therapist assesses a patient's pulse and assigns a grade of '1+'. What does this indicate about the pulse's characteristics?
When conducting the Allen's test, what outcome suggests arterial occlusion?
When conducting the Allen's test, what outcome suggests arterial occlusion?
Why is the Ankle-Brachial Index (ABI) used in cardiovascular assessment?
Why is the Ankle-Brachial Index (ABI) used in cardiovascular assessment?
An ABI result greater than 1.3 indicates:
An ABI result greater than 1.3 indicates:
What is the clinical interpretation of an ABI value of 0.8?
What is the clinical interpretation of an ABI value of 0.8?
What is a clinical indication for performing an ABI?
What is a clinical indication for performing an ABI?
What formula is used when calculating the Body Mass Index(BMI)?
What formula is used when calculating the Body Mass Index(BMI)?
A patient has a BMI of 31. How would you categorize this patient?
A patient has a BMI of 31. How would you categorize this patient?
What are the health risks for someone with a BMI between 25-29.9?
What are the health risks for someone with a BMI between 25-29.9?
What is assessed using waist circumference measurements?
What is assessed using waist circumference measurements?
When measuring waist circumference, at what level should measurements be taken?
When measuring waist circumference, at what level should measurements be taken?
Why are physical therapist asked to take blood pressure at rest, with activity, and for orthostatic assessment?
Why are physical therapist asked to take blood pressure at rest, with activity, and for orthostatic assessment?
Which sounds are important about the Korotkoff sounds over an artery?
Which sounds are important about the Korotkoff sounds over an artery?
What is an important precaution when taking blood pressure?
What is an important precaution when taking blood pressure?
What defines as elevated blood pressure?
What defines as elevated blood pressure?
What is the blood pressure for infants?
What is the blood pressure for infants?
What decrease in blood pressures determine orthostatic hypotension?
What decrease in blood pressures determine orthostatic hypotension?
Where should the cuff be placed and how should the leg be if testing BP in the thighs?
Where should the cuff be placed and how should the leg be if testing BP in the thighs?
What can the waist circumference tell a therapist?
What can the waist circumference tell a therapist?
What are the measurements for increased cardiovascular risks for men and women?
What are the measurements for increased cardiovascular risks for men and women?
Besides diagnosis and age, what other vital information from a patient's medical chart should a physical therapist review during a cardiovascular assessment to understand their current health status?
Besides diagnosis and age, what other vital information from a patient's medical chart should a physical therapist review during a cardiovascular assessment to understand their current health status?
What is the significance of assessing sleep patterns, specifically orthopnea and paroxysmal nocturnal dyspnea (PND), during a cardiovascular evaluation?
What is the significance of assessing sleep patterns, specifically orthopnea and paroxysmal nocturnal dyspnea (PND), during a cardiovascular evaluation?
What is the MOST important aspect of durable medical equipment usage a physical therapist should note from a patient’s social history during a cardiovascular assessment?
What is the MOST important aspect of durable medical equipment usage a physical therapist should note from a patient’s social history during a cardiovascular assessment?
When gathering subjective information from a patient during a cardiovascular assessment, why is it crucial for a physical therapist to primarily use open-ended questions?
When gathering subjective information from a patient during a cardiovascular assessment, why is it crucial for a physical therapist to primarily use open-ended questions?
Assessing a patient's general appearance during a cardiovascular evaluation provides insights into their overall health status. What might asymmetrical chest movement during respiration suggest?
Assessing a patient's general appearance during a cardiovascular evaluation provides insights into their overall health status. What might asymmetrical chest movement during respiration suggest?
What is indicated by a patient sitting in a tripod position?
What is indicated by a patient sitting in a tripod position?
What critical assessment finding is suggested by jugular venous distention (JVD)?
What critical assessment finding is suggested by jugular venous distention (JVD)?
During auscultation, why is the diaphragm of a stethoscope typically used to assess S1 and S2 heart sounds?
During auscultation, why is the diaphragm of a stethoscope typically used to assess S1 and S2 heart sounds?
In cardiac auscultation, what does the S1 heart sound represent?
In cardiac auscultation, what does the S1 heart sound represent?
When auscultating a patient with suspected aortic stenosis, where would S2 be heard the loudest?
When auscultating a patient with suspected aortic stenosis, where would S2 be heard the loudest?
What is the clinical significance of an S3 heart sound in adults?
What is the clinical significance of an S3 heart sound in adults?
What does the term 'stenosis' mean when describing heart murmurs?
What does the term 'stenosis' mean when describing heart murmurs?
During a cardiovascular examination, where is it recommended to position the stethoscope to best auscultate the pulmonic valve sounds?
During a cardiovascular examination, where is it recommended to position the stethoscope to best auscultate the pulmonic valve sounds?
What does the presence of central cyanosis indicate?
What does the presence of central cyanosis indicate?
When assessing for edema, a physical therapist notes a ~4mm indentation that disappears in approximately 12 seconds. How should this edema be graded?
When assessing for edema, a physical therapist notes a ~4mm indentation that disappears in approximately 12 seconds. How should this edema be graded?
If a physical therapist palpates a pulse and assigns a grade of '2+', what does this grading indicate?
If a physical therapist palpates a pulse and assigns a grade of '2+', what does this grading indicate?
Following the Allen's test, what finding would indicate a patent ulnar artery but an occlusion in the radial artery?
Following the Allen's test, what finding would indicate a patent ulnar artery but an occlusion in the radial artery?
What does an Ankle-Brachial Index (ABI) assess in cardiovascular evaluation?
What does an Ankle-Brachial Index (ABI) assess in cardiovascular evaluation?
Which of the following is a potential finding that would suggest peripheral artery disease in the lower limb?
Which of the following is a potential finding that would suggest peripheral artery disease in the lower limb?
What does a BMI help to indicate?
What does a BMI help to indicate?
If a patient's BMI is calculated to be 27, into which category would they be classified.
If a patient's BMI is calculated to be 27, into which category would they be classified.
What range of values does elevated blood pressure fall into?
What range of values does elevated blood pressure fall into?
What is the typical range of blood pressure for infants between 0-12 months of age?
What is the typical range of blood pressure for infants between 0-12 months of age?
To accurately assess blood pressure in the lower extremities, how should the patient be positioned, particularly when measuring blood pressure in the thigh?
To accurately assess blood pressure in the lower extremities, how should the patient be positioned, particularly when measuring blood pressure in the thigh?
What measurements put men and women at increased cardiovascular risk according to waist circumferences?
What measurements put men and women at increased cardiovascular risk according to waist circumferences?
Flashcards
Cardiovascular PT Evaluation
Cardiovascular PT Evaluation
Parts of a physical therapy evaluation regarding a patient's cardiovascular system
Patient Interview
Patient Interview
Evaluation of the patient through interview
Auscultation
Auscultation
Listening for sounds within the body
General Observation
General Observation
Signup and view all the flashcards
Mental Status
Mental Status
Signup and view all the flashcards
Heart Sounds: S3 & S4
Heart Sounds: S3 & S4
Signup and view all the flashcards
Stethoscope
Stethoscope
Signup and view all the flashcards
Heart Sounds: S1 & S2
Heart Sounds: S1 & S2
Signup and view all the flashcards
Heart Murmurs
Heart Murmurs
Signup and view all the flashcards
Auscultation Landmarks
Auscultation Landmarks
Signup and view all the flashcards
Trophic Changes
Trophic Changes
Signup and view all the flashcards
Central Cyanosis
Central Cyanosis
Signup and view all the flashcards
Edema
Edema
Signup and view all the flashcards
Anasarca
Anasarca
Signup and view all the flashcards
Pulse
Pulse
Signup and view all the flashcards
Blood Pressure
Blood Pressure
Signup and view all the flashcards
Korotkoff Sounds
Korotkoff Sounds
Signup and view all the flashcards
Orthostatic Hypotension
Orthostatic Hypotension
Signup and view all the flashcards
Capillary Refill
Capillary Refill
Signup and view all the flashcards
Allen Test
Allen Test
Signup and view all the flashcards
Peripheral Limb Measurement
Peripheral Limb Measurement
Signup and view all the flashcards
Ankle Brachial Index
Ankle Brachial Index
Signup and view all the flashcards
Body Mass Index
Body Mass Index
Signup and view all the flashcards
Waist Circumference
Waist Circumference
Signup and view all the flashcards
Study Notes
- Cardiovascular assessment is part of a PT evaluation especially for cardiovascular patients
Objectives
- Describe PT evaluation aspects related to cardiovascular patients
- Recognise heart sounds and their significance
- Explain the cardiac auscultation procedure
- Identify pulse palpation locations
- Describe skin and edema assessment methods
- Explain BP measurement at rest, during activity, and for orthostatic assessment
- Explain how BMI and waist circumference relate to CV risk
- Identify the proper sequence and steps for emergency procedures, including CPR, rescue breathing, and AED use
Initial Evaluation: Medical Chart Review
- Review of medical chart during the initial evaluation including:
- Diagnosis
- Age
- Medications
- CC/HPI (Chief Complaint/History of Present Illness)
- PMH/PSH ( Past Medical History/Past Surgical History). This includes co-morbidities and possible implications of disease processes
- Risk Factor Analysis
- Special Tests that have been performed
- Social History is important in initial evaluation
- Including where patient lives and with whom
- As well as their durable medical equipment (assistive devices, Oxygen)
- Prior activity level
- Sleep Patterns (orthopnea, PND)
- Hospital Course
- Labs, Tests, Treatments/Interventions and Medications
Initial Evaluation: Patient Interview
- Patient interview is key to initial evaluation including:
- Subjective feedback, "I feel..."
- Pain levels
- Verbal/non-verbal communication
- Use open questions (how, why, when, where, what)
- And close ended questions requesting minimal "Yes," or "No" responses,
- Avoid leading questions that bias patient w/bias
- Objective/Physical Assessment also key in initial evaluation
- Through Patient Observation
- Of Lines/Tubes/Drains
- And Monitoring equipment Orthostatic assessment of vital signs
Sample Social History Gathering
- An example interaction with a patient explaining the PT's role and inquiring about their feelings, living situation.
- Social Hx includes whether they live alone, who they live with, and type of residence (house or apartment) and floors
- Questions focused on home accessibility with questions regarding:
- Stairs, elevators, railings, and the availability of equipment like canes, walkers, commodes, or shower chairs.
Initial Evaluation: Physical Assessment
- Physical assessments includes general observation/appearance, mental status, auscultation, and skin/vasculature
- Observations:
- Heart/Lungs
- Wounds
- Pulses
- Capillary refill _ Sensation
- Balance:
- Sitting
- Standing
- Coordination
- Functional Assessment
- Bed mobility
- Transfers
- Ambulation including level and stairs
Initial Evaluation: Observation
- The level of respiratory distress provides valuable insights
- Look for: SOB(tachypnea)/DOE, Nasal flaring, Pursed lip breathing, Use of accessory muscles, Cyanosis
- Observation – Position plays a factor
- Bed and Extremity positions
- Tripod position indicates use of accessory muscles of respiration
Initial Evaluation: Observation
- Body Type:
- Apple vs. Pear
- Cachectic
- Head & Neck:
- Especially the Jugular venous distention (JVD)
- Is considered present if superficial veins distend above the level of the clavicles
Initial Evaluation: Mental Status
- Assess Level of consciousness
- Assess ability to follow directions
Auscultation
- Primarily done to listen for murmurs and crackles in the heart or lungs
- A stethoscope is used, particularly the Diaphragm and Bell portions
Heart Sounds
- Heart sounds that are audible originate from the sounds of blood moving thru the valve closures
- Sounds to Recognize Include:
- 1st Heart Sound = S1
- 2nd Heart Sound = S2
- 3rd Heart Sound = S3
- 4th Heart Sound = S4
- A loud 2nd heart sound is suggestive of pulmonary HTN
Heart Sounds: Systolic
- S1 and S2 are normal heart sounds, and relatively high pitched
- Commonly referred to as "Lub-Dub"
- When listening for the sounds you should use the diaphragm side of the stethoscope
- S1: "Lub" sound originates with the Atrioventricular valves closing
- Closing of MV (Mitral Valve) and TV (Tricuspid Valve)
- S2: "Dub" sound originates with the Semilunar valves closing
- Closing of AV (Aortic Valve) and PV (Pulmonic Valve)
- Differentiating involves noting that S1 tends to be shorter in duration than S2
- S2 is then longer in duration that S1
- Auscultation allows for ventricles to fill Splitting can occur with S1 or S2
Heart Sounds: S1 vs S2
- S1 correlates with the "Lub" sounds
- "Lub" sounds arise from the closure of the atrioventricular valves indicating the beginning of systole
- S1 is usually loudest at the Mitral area (cardiac apex) where S1 is louder than S2 Has two components, Tricuspid and Mitral
- Auscultation uses the diaphragm with firm pressure
- S2 correlates withe sounds arising from the closure of the semilunar valves
- Indicating the end of systole.
- S2 loudest at the Aortic and Pulmonic area where S2 is louder than S1
- Has two components, Aortic and Pulmonic
- Auscultation uses the diaphragm with firm pressure
Heart Sounds: Abnormal Sounds
- S3, S4 often indicates presence of diastolic sounds, and are low frequency and soft
- Use the bell shaped side of the stethoscope
- S3 (lub-dub-dub):
- Is heard in early diastole
- S4 (la-lub-dub):
- Is heard in late diastole
Heart Sounds: Gallop Rhythms
- Additional abnormal sounds include:
- S3= LUB-DUB-DUB(S1, S2, S3)
- Is AKA Gallop S3, or a "ventricular gallop"
- Representing loss of ventricular compliance, heard immediately after S2
- S3 occurs early in diastole
- And is produced during passive LV filling
- Usually normal in children, young adults, and well trained athletes
- But abnormal among older patients with heart disease.
- It can be a key diagnostic sign for CHF, as well as for Mitral regurgitation, Ventricular Septal Defect, or Congenital Heart Block
- Best heard in the Mitral area with patient in left lateral decubitus, following exercise where S3 is louder than S2
- Low pitch – use bell to auscultate (LIGHT PRESSURE)
Heart Sounds: Atrial Gallop
- S4= LALUB-DUB:
- Is aka Gallop S4, or “atrial gallop” which represents increased resistance to ventricular filling before S1
- It occurs late in diastole during active LV filling and is rarely normal
- When abnormal, usually the patient is:
- Children
- Or adults
- Typically common in patients with hypertensive cardiac disease, CAD, and with pulmonary disease, as well as MI or post bypass surgery.
- Conditions typically associated includes:
- AS(Aortic Stenosis)
- PS (Pulmonary Stenosis)
- Hypertrophic cardiomyopathy (HCM)
- Low pitch – use bell to auscultate (LIGHT PRESSURE)
- The Summation Gallop arises from the S1, S2, S3 and S4 sounds
- Is due to the S3 and S4 frequencies being superimposed rhythmically Often resulting in a quadruple rhythm, mimicking the sound of a galloping horse
- Usually is found in patients with tachycardia
- And tends to be associated with cardiac disease, stenotic lesions, MI, CHF
Heart Sounds: Murmurs
- Murmurs generate a "whoosh" turbulence that is not related to valve closing
- They tend to be caused by turbulent blood flow and are Described by:
- Position in cardiac cycle (systolic vs. diastolic)
- Duration (Entire phase, Start/stop w/in phase)
- Quality (sharp, snapping, dull, rumbling, blowing, musical, scratchy, harsh, soft, swishing) Intensity/Loudness (based on Levine scale)
- Causes Include:
- High rates of flow through normal and abnormal valves
- Forward flow through constricted and/or irregular shaped valves into a dilated vessel (stenosis)
- Backward flow through an incompetent valve (REGURGITATION)
- Decreased viscosity leading to an increased turbulence (FLUID OVERLOAD)
Ejection vs Opening Sounds
- Systolic Murmurs: include Aortic Stenosis, Mitral Valve Prolapse, Mitral Regurgitation, Pulmonary Stenosis, Ventricular Septal Defect, and Atrial Septal Defect
- Diastolic Murmurs: include Aortic Regurgitation and Mitral Stenosis
- Ejection sounds occur during the systole phase
- Arise due to forceful/rapid ejection of blood, typically past an obstruction
- And results in high frequency sounds .
- Arise due to forceful/rapid ejection of blood, typically past an obstruction
Systolic vs Diastolic Clicks
- Systolic Click
- Is caused by the prolapsed mitral (or tricuspid) valve that falls backward into the atria, and leads to regurgitant blood flowing forcefully past the prolapsed valve which causes turbulence.
- Its sounds are heard as single or multiple "clicking” sounds during systole
- Mitral valve prolapse is more common in females, usually benign
- Pericardial friction rub is caused by an increase in the pericardial fluid in the pericardial sac which is often associated with pericarditis.
- This often Impairs filling of the ventricles during diastole
- The filling ventricles “rub” against the engorged pericardial sac and produces leathery or squeaky sound Occurring during diastole, and usually also during systole when there is marked pericardial fluid present
Auscultation Procedure
_ Create a quiet environment and ask patient breathes quietly to listen better
- Expose areas for auscultation ensuring there is bare skin for auscultation
- To avoid extra sounds from clothing
- Use the diaphragm rather than the bell Ensure pt is in a supine or semi-fowlers position
- Good for most heart sounds
- Ensure to start the process from apex of heart, working superiorly toward the base
Auscultation Procedure Locations
- The most common auscultation locations include:
- Aortic: 2nd ICS, and right sternal border
- Pulmonic: 2nd ICS, and left sternal border
- Tricuspid: 4th (and often also including the 5th) ICS, left sternal border
- Mitral: cardiac apex/PMI, 5th ICS, medial to the line from the midclavicular line
- Erb's Point (best for S2 heart sound) at the Left sternal border, 3 rd ICS
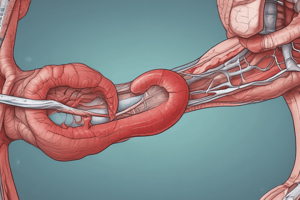
Vascular Assessment
-
Trophic changes and Pigmentation
-
One should assess the skin for:
- Abnormal pigmentation
- Dermatitis
- Ulceration
- Coloration and changes with position of the limb/body
- Loss of hair from the area
- Thickened nail bed
- Hemosiderin
- Presence of any Incisions, wounds, or dressings
- Whether the site is exhibiting signs of Pallor or Diaphoresis/flushing
-
Skin Assessment looks for presence of cyanosis (lips, tounge) and/or hypoxemia
-
Also looks for clubbing (pulmonary HTN, CF)
-
Peripheral cyanosis
-
May indicate Inadequate CO leading to decreased peripheral perfusion (PVD)
- Possibly with varicosities, or PAD – CAD and/or obesity, male patients using tobacco as well as Raynaud's phenomenon
Skin Assessment: Edema
- Edema presence can be classified as Pitting vs non-pitting
- That is present in the Extremities or Abdomen
- Note: Anasarca – severe, generalized, massive (total body) edema
- Pitting edema evaluation and grading requires two fingers against a particular area
- The assessment will usually take two to three seconds (if an indentation occurs then the edema is classified as "pitting”)
- Once qualified the, further graded based on depth of "pit" & how long it remains.
- This includes:
- 1+ = ~2mm in depth or very shallow); disappears rapidly
- 2+ = ~4mm in depth; skin rebounds in < 15 sec
- 3+ = ~6 mm in depth; extremity looks grossly swollen; skin rebounds in varying times found (15-30 sec, > 1 min)
- 4+ = ~8 mm in depth (or more); skin rebounds in varying times found (> 30 sec, may last > 2 min)
Vascular Assessment: Pulses
- Palpation or use of Doppler enables grading pulse on the following scale:
- 0 = no palpable pulse
- 1+ = faint, but detectable pulse
- 2+ = slightly more diminished pulse than normal
- 3+ = normal pulse
- 4+ = bounding pulse
- Auscultation is also key in assessing vascular activity
- Checking for Bruit and "Thrill" which means something is being palpated
- Temperature can be used to asses if there are gross differences
Palpation Sites
- Carotid, Brachial, Radial, Femoral, Popliteal, Dorsalis pedis and Posterior tibial pulses And the Apical Pulse
- The point of maximal impulse (PMI) which you palpate or auscultate
Pulse Assessment
- Carotid: use light pressure as you can cause a vagal response
- Brachial: cubital fossa medial to the biceps tendon
- Radial: medial to the radial styloid process on the palmar surface of the forearm
- Femoral: just inferior to the inguinal ligament half way between the ASIS and the pubic tubercle
- Popliteal: in the popliteal fossa with the Knee flexed
- Dorsalis pedis: between the ext hallicus longus and the ext digitorum longus on the dorsum of the foot (Absent in 10% of population)
- Posterior tibial: posterior and inferior to medial malleolus Assessments of arterial pulses include considering: Rate, Regularity, and Quality
- Newborn (0-3 months): 100-150 bpm
- Infants (3-12 months): 80-120 bpm
- Children (1 – 10 years): 70-130 bpm
- Children > 10 years & Adults: 60-100 bpm
Vascular Assessment pt II
- Measuring blood pressure involves:
- Korotkoff sounds -sound heard over an artery
- Use correct cuff size, and note that too wide a cuff will result too low a reading
- While too small a cuff will result too high a reading
- Blood pressure can Be taken at Brachial, Thigh and Calf
- However, there are precautions when taking Brachial: Mastectomy, DVT, in presence of IV lines, AV fistula, and Fracture cases As well as with Lymphedema, Lymph node dissection or Sentinel node dissections
Blood Pressure: Classifications
- A blood pressure category of normal indicates the patient's: Systolic is less than 120 and Diastolic is less than 80
- An elevated range indicates the patient's: Systolic is 120 -129 and Diastolic is still less than 80
- High Blood Pressure (Hypertension) Stage 1 patient's reading: Systolic is 130-139 or Diastolic 80-89
- High Blood Pressure (Hypertension) Stage 2 patient's reading: Systolic is 140 or higher or Diastolic is 90 or higher
- Hypertensive Crisis requires you to consult the doctor immediately due to reading: Systolic is higher than 180 and/or Diastolic is higher than 120
Blood Pressure: Norms by Age
- For children under 10 years, the following guidelines apply
- 0-12 months: 65-100 mmHg / 45-65 mmHg
- 1-12 years: 90-120 mmHg / 55-75 mmHg
- And after 12+ years: 110-135 mmHg / 65-85 mmHg
- Orthostatic or Postural Vitals are useful for when you evaluate body's response to position changes especially suspicion of intravascular volume loss. This includes checking for:- Decreased SBP (20 mmHg or greater) Decreased DBP (10 mmHg or greater) Increase HR often occurs in response to sudden drop in BP (often 20 bpm or greater)
- Recommendations for BP assessment include, taking it when a pt is:
- In supine
- 1 min post standing
- 3 min post standing after
Taking Ankle/Thigh Blood Pressures
- When taking a thigh blood pressure you must ensure the patient is in a:
- Pt supine w/ hip+knees flexed, or in prune position
- Place the cuff proximal to the popliteal artery (2-3 cm)
- Then using a Doppler or stethescope listen near the popliteal artery to assess Taking an ankle Blood pressure
- Place the patient supine
- Place the cuff above the malleoli (2-3 cm)
- Then you can palpate of posterior tibial or dorsalis pedis artery
- However, be aware that Doppler is the only way to accurately measure pressure.
Diagnostic Testing and Measures
- Capillary Refill Time
- Allen Test
- Waist Circumference or Peripheral limb measurements
- ABI = ankle brachial index
- BMI = body mass index
- Waist Circumference The Capillary Refill Test (Nail Blanch Test) measures: Time for capillary bed to refill after being by pressure
- This test is an Indication of perfusion to extremities
- Procedure relies on applying firm pressure to nail bed or bony prominence release pressure pressure
- and the checking if Time for nail or skin to regain full color.
- Usually full color returns in less than 2 seconds.
Diagnostic Testing and Measures pt II
- Allen Test
- Assesses for Vascular Insufficiency
- Place sitting pt and have then open/close hand several times, then hold in closed position
- As you compress radial and ulnar arteries release hand and you release pressure on one of the arteries, and note that there is immediate flushing of the area.
- In a positive test the pt will have delayed or absent flushing and may indicate occlusion in related arteries
- Peripheral Limb Measurement looks for Girth changes due to edema
- Compare leg to leg or arm to arm often using the same landmarks each time Ankle Brachial Index (ABI)
- Is obtained by dividing the systolic pressure at the ankle by the brachial systolic pressure.
- You should usethe highest brachial pressure to work
- Note that the Ankle SBP is normally higher than Brachial SBP Make sure you are testing when pt is supine as well
Ankle Brachial Index (ABI)
- The ABI provides use of Doppler and will help amplify the sounds when used to measure a patient pressure
- Calculation is Ankle SBP / Brachial SBP (ex: 140 mmHg / 130 mmHg = 1.08)
- And lower calculation would indicate disease( ex:110 mmHg / 130 mmHg = .85)
- Is useful for evaluate:
- Claudication or a Vascular component of rest pain,
- Evaluate appropriateness and safety for exercise and for use of compression garments
- And/or checking Tissue health when distal perfusion testing for would healing is needed Normal reading for lower extremeties _ 60 mmHg is normal _ 80 mmHg is normal
Ankle Brachial Index (ABI)
- AHA: 0.90 or less clinical suspicion for PAD
- Normal: 1.0 - 1.1
- Borderline: 0.91 - 0.99
- Abnormal:
- Less than <0.9 or >1.3
- If above> 1.3, the vessels test unreliably due to presence of calcified vessels (diabetes) causing falsely elevated pressures
- If Below<0.9 suggests significant narrowing in 1 or more blood vessels with claudication
- Often with rest pain or severe occlusive disease causing ischemic to gangrenous extremities
- Acute Care Handbook reads numbers as follows:
/=1.0-1.3 equals normal function with normal range /= 0.7-0.8 equals borderline perfusion <=0.5 indicates cases with severe ischemia <=0.4 indicates critical limb ischemia
- While review books reads >/=1.30 as Rigid arteries. The values indicate a need for U/S check for PAD The rest follows a: 1.0-1.3 normal without blockage 0.8-0.99 Mild Blockage showing beginning stage for PAD 0.4-0.79 Moderate Blockage, associated with intermittent claudication <=0.4 Severe blockage, Suggestive of severe PAD, may have claudication pain at rest. What is Body Mass Index (BMI)? Meausres weight relative to Height ratio = Body mass index (BMI) is a measure of body fat based on height and weight A reliable indicator of body fatness for most people and Used to screen for weight categories that may lead to health problems Calculated via Weight/Height² and Expressed in kg/m² or lb/in²
- Weight status categories on BMI are the same for all ages and for men and women And it Correlates to direct measures of body fat, such as underwater weighing and dual energy x-ray absorptiometry (DXA). Underweight when its Lessthan 18.5 Normal weight = 18.5-24.9; Overweight when its equal or between 25-29.9;
BMI Categories
Obesity: Is a BMI of 30 or greater, which can be calculated via online BMI calculator.
- The additional Waist Circumference enables assessing abdominal fat
- And also is useful re: estimating decreased abdominal fat even without changes in BMI by positioning patient in standing
- tape measure around abdomen at level of iliac crest at end of normal exhalation Results in higher risk when more than 102 cm (>40 inches) for men And greater than> 88 cm (> 35 inches) for women Results in higher risk for Type 2 DM, HTN, dyslipidemia, and cardiovascular disease
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.