Podcast
Questions and Answers
What is a potential management step for a patient exhibiting sinus bradycardia symptoms?
What is a potential management step for a patient exhibiting sinus bradycardia symptoms?
- May need atropine (correct)
- Immediate surgery
- Administer aspirin
- Increase fluid intake
In what situation should synchronized cardioversion be considered in sinus tachycardia?
In what situation should synchronized cardioversion be considered in sinus tachycardia?
- Patient is experiencing chest pain (correct)
- Patient has a stable heart rate over 100 bpm
- Patient has a resting heart rate below 60 bpm
- Patient is asymptomatic
Which characteristic is true for premature ventricular complexes (PVC)?
Which characteristic is true for premature ventricular complexes (PVC)?
- Always associated with a visible P wave
- Always indicates heart failure
- QRS duration of less than 0.12 seconds
- Irregular rhythm due to early QRS (correct)
What sound is associated with S3 heart sound and when does it occur?
What sound is associated with S3 heart sound and when does it occur?
What might indicate the presence of a fourth heart sound (S4)?
What might indicate the presence of a fourth heart sound (S4)?
How can a friction rub sound be best characterized?
How can a friction rub sound be best characterized?
Which of the following is NOT a common cause of murmurs?
Which of the following is NOT a common cause of murmurs?
What is the appropriate ratio of compressions to rescue breaths in CPR?
What is the appropriate ratio of compressions to rescue breaths in CPR?
Which of the following conditions represents an unresponsive patient needing immediate action?
Which of the following conditions represents an unresponsive patient needing immediate action?
What percentage of Americans are likely to have primary hypertension?
What percentage of Americans are likely to have primary hypertension?
Which of the following is NOT considered a complication of hypertension?
Which of the following is NOT considered a complication of hypertension?
What is the primary purpose of thiazide diuretics in the treatment of hypertension?
What is the primary purpose of thiazide diuretics in the treatment of hypertension?
In a hypertensive emergency, what should the mean arterial pressure be reduced by during the first hour?
In a hypertensive emergency, what should the mean arterial pressure be reduced by during the first hour?
Which medication is associated with the side effect of a dry cough?
Which medication is associated with the side effect of a dry cough?
Which risk factor is associated with a higher prevalence of hypertensive disorders?
Which risk factor is associated with a higher prevalence of hypertensive disorders?
Which characteristic symptom is primarily associated with peripheral artery disease (PAD) in the lower extremities?
Which characteristic symptom is primarily associated with peripheral artery disease (PAD) in the lower extremities?
What is the recommended daily foot care routine for a patient with PAD?
What is the recommended daily foot care routine for a patient with PAD?
Which condition can indicate a serious complication such as compartment syndrome in a patient with PAD?
Which condition can indicate a serious complication such as compartment syndrome in a patient with PAD?
Which treatment modality is classified as a pharmacologic intervention for managing PAD?
Which treatment modality is classified as a pharmacologic intervention for managing PAD?
What pathophysiological change occurs as a result of chronic venous insufficiency?
What pathophysiological change occurs as a result of chronic venous insufficiency?
During which time of day do patients typically experience fewer symptoms of chronic venous insufficiency?
During which time of day do patients typically experience fewer symptoms of chronic venous insufficiency?
Which of the following is NOT a recommended patient education point for managing foot health in PAD?
Which of the following is NOT a recommended patient education point for managing foot health in PAD?
What term describes the indication of fluid imbalances that includes urine output changes and altered mental status in PAD-related complications?
What term describes the indication of fluid imbalances that includes urine output changes and altered mental status in PAD-related complications?
In the management of PAD, what does the acronym '5 P's' stand for?
In the management of PAD, what does the acronym '5 P's' stand for?
Which of the following is a surgical treatment option for addressing PAD?
Which of the following is a surgical treatment option for addressing PAD?
What is the primary trigger for stable angina?
What is the primary trigger for stable angina?
Which laboratory value should be monitored for a patient receiving Heparin drip?
Which laboratory value should be monitored for a patient receiving Heparin drip?
Which clinical manifestation is primarily associated with right-sided heart failure?
Which clinical manifestation is primarily associated with right-sided heart failure?
What happens as a result of Angiotensin II stimulation in the RAAS system?
What happens as a result of Angiotensin II stimulation in the RAAS system?
Which of the following medications is commonly used to prevent platelet aggregation in patients at risk for myocardial infarction?
Which of the following medications is commonly used to prevent platelet aggregation in patients at risk for myocardial infarction?
What is the goal of using diuretics in patients with pulmonary edema?
What is the goal of using diuretics in patients with pulmonary edema?
What is a potential consequence of the compensatory mechanisms activated during heart failure?
What is a potential consequence of the compensatory mechanisms activated during heart failure?
Which risk factor for atherosclerosis is considered modifiable?
Which risk factor for atherosclerosis is considered modifiable?
Which symptom is most indicative of left-sided heart failure?
Which symptom is most indicative of left-sided heart failure?
What is the purpose of a Left Ventricular Assist Device (LVAD)?
What is the purpose of a Left Ventricular Assist Device (LVAD)?
What is indicated by the presence of ECG changes in two contiguous leads during a myocardial infarction?
What is indicated by the presence of ECG changes in two contiguous leads during a myocardial infarction?
Which of the following is a contraindication for administering Nitroglycerin?
Which of the following is a contraindication for administering Nitroglycerin?
Which modifiable risk factor is associated with coronary artery disease (CAD)?
Which modifiable risk factor is associated with coronary artery disease (CAD)?
What should be monitored post-cardiac catheterization to assess potential complications?
What should be monitored post-cardiac catheterization to assess potential complications?
In the assessment of a myocardial infarction, elevated Troponin levels indicate what?
In the assessment of a myocardial infarction, elevated Troponin levels indicate what?
What is the first intervention recommended for treating a myocardial infarction?
What is the first intervention recommended for treating a myocardial infarction?
Which lifestyle modification is vital for patients at risk for coronary artery disease?
Which lifestyle modification is vital for patients at risk for coronary artery disease?
What is the primary nursing intervention to be performed during an acute myocardial infarction?
What is the primary nursing intervention to be performed during an acute myocardial infarction?
Which of the following best describes a NSTEMI?
Which of the following best describes a NSTEMI?
What specific cardiac condition does preeclampsia increase the risk for later in life?
What specific cardiac condition does preeclampsia increase the risk for later in life?
Flashcards are hidden until you start studying
Study Notes
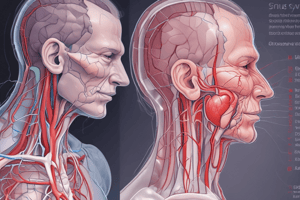
Cardiac Rhythms and Management
- An increase of 10 bpm or more in resting heart rate is linked to a higher risk of sudden cardiac death, atrial fibrillation, heart failure, coronary artery disease (CAD), stroke, and cardiovascular disease.
Sinus Bradycardia
- Characterized by a heart rate of less than 60 bpm, normal P wave positioned before QRS, PR interval between 0.12 and 0.20 seconds.
- 1:1 ratio of P waves to QRS complexes.
- Management based on symptoms: symptomatic patients may require atropine, transcutaneous pacing, or catecholamines.
- Nurse actions include patient assessment for symptoms like fatigue and light-headedness. For asymptomatic cases, monitor ECG and vital signs.
Sinus Tachycardia
- Defined by a heart rate greater than 100 bpm with a regular rhythm and normal P waves (which may be obscured in T waves).
- Management involves treating underlying causes, with symptomatic patients potentially requiring synchronized cardioversion or adenosine administration.
- Important nursing actions include assessing patient status and checking for factors such as fever or dehydration.
Ventricular Dysrhythmias
- Premature Ventricular Complex (PVC): Early impulse from the ventricle with abnormal QRS morphology, visible P waves depend on PVC timing, PR interval less than 0.12 seconds.
- Ventricular Tachycardia (VTACH), Ventricular Fibrillation (VFIB), PEA, and Asystole are critical pulseless rhythms that necessitate immediate CPR.
Heart Sounds and Clinical Assessment
- Third Heart Sound (S3) is indicative of heart failure, heard during rapid ventricular filling.
- Fourth Heart Sound (S4) relates to hypertensive heart disease, occurring during atrial contraction.
- Other sounds include opening snaps (associated with AV valve malfunction) and systolic clicks (from stenosis of semilunar valves).
- Murmurs caused by turbulent blood flow can result from narrowed or malfunctioning valves.
- A friction rub is a harsh sound linked to pericarditis and can mimic murmurs.
Cardiopulmonary Resuscitation (CPR)
- Effective CPR consists of a compression to breath ratio of 30:2.
- The process prioritizes assessing the patient's responsiveness and circulation, followed by calling for assistance.
- Essential to provide blood flow to vital organs until circulation is restored.
Myocardial Infarction
- Acute Coronary Syndrome leads to myocardial death due to ischemia.
- STEMI shows characteristic ECG changes; NSTEMI presents elevated cardiac biomarkers without notable ECG changes.
- Treatment begins with oxygen, followed by nitroglycerin, morphine, and aspirin (with contraindications for low blood pressure and viagra use).
- Patient education includes lifestyle modifications and monitoring for cardiac symptoms.
Coronary Artery Disease (CAD) Risk Factors
- Modifiable: hyperlipidemia, tobacco use, hypertension, diabetes, and obesity.
- Nonmodifiable: family history, age, gender, race.
- Post-Operative Care after CABG focuses on ensuring adequate heart function and monitoring for complications.
Heart Failure
- Key diagnostic test: B-type natriuretic peptide (BNP).
- Right heart failure presents with edema and distended neck veins; left heart failure affects lung function, causing dyspnea.
- Risk factors include myocardial infarction, aging, and valve abnormalities.
- Education emphasizes a low-sodium diet and daily weight monitoring.
Atherosclerosis and Peripheral Vascular Disease (PAD)
- Atherosclerosis involves plaque build-up influenced by both modifiable (smoking, diabetes) and nonmodifiable (age, genetics) risk factors.
- PAD often presents as intermittent claudication and is characterized by reduced blood flow to limbs.
- Patient education on foot hygiene is crucial; complications include ulcers and gangrene.
Hypertension
- New definitions categorize hypertension over 130/80 mmHg; complication risks include heart attack and kidney disease.
- Primary hypertension has no identifiable cause; secondary hypertension stems from specific conditions.
- Evidence suggests lifestyle changes and dietary modifications are essential for management.
- Medications include thiazide diuretics, ACE inhibitors, and calcium channel blockers; patient education is crucial for adherence and monitoring.
Hypertensive Crisis
- Defined by severe elevations in blood pressure (>180/100 mmHg).
- Emergency treatment requires immediate intervention to decrease mean arterial pressure by 20-25% with IV vasodilators.
- Urgency requires careful monitoring without evidence of immediate organ damage.
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.