Podcast
Questions and Answers
What adaptations in veins ensure the return of blood to the heart?
What adaptations in veins ensure the return of blood to the heart?
Venous valves and venous sinuses
What is the purpose of arterial anastomoses?
What is the purpose of arterial anastomoses?
- Reduce resistance
- Increase blood pressure
- Provide alternate pathways for continuous flow (correct)
- Block blood flow
Varicose veins are caused by competent valves.
Varicose veins are caused by competent valves.
False (B)
Blood flow is directly proportional to blood pressure gradient and inversely proportional to __________.
Blood flow is directly proportional to blood pressure gradient and inversely proportional to __________.
What are the two locations of baroreceptors that are mentioned in the text?
What are the two locations of baroreceptors that are mentioned in the text?
Which hormones regulate blood pressure in the short term?
Which hormones regulate blood pressure in the short term?
How is systemic arterial blood pressure typically measured?
How is systemic arterial blood pressure typically measured?
What is the normal range for systolic blood pressure?
What is the normal range for systolic blood pressure?
What hormone decreases blood pressure by antagonizing aldosterone?
What hormone decreases blood pressure by antagonizing aldosterone?
Why is low capillary pressure desirable?
Why is low capillary pressure desirable?
Hypertension is defined by sustained elevated arterial pressure of 140/90 mm Hg or higher.
Hypertension is defined by sustained elevated arterial pressure of 140/90 mm Hg or higher.
Match the following conditions with the correct blood pressure range: 1) Hypertension, 2) Hypotension
Match the following conditions with the correct blood pressure range: 1) Hypertension, 2) Hypotension
Venous blood pressure changes significantly during the cardiac cycle.
Venous blood pressure changes significantly during the cardiac cycle.
What are the three main factors regulating blood pressure?
What are the three main factors regulating blood pressure?
What is autoregulation in terms of blood flow?
What is autoregulation in terms of blood flow?
Which of the following are examples of vasodilators? (Select all that apply)
Which of the following are examples of vasodilators? (Select all that apply)
Long-term autoregulation can occur within a short period to meet tissue nutrient requirements.
Long-term autoregulation can occur within a short period to meet tissue nutrient requirements.
At rest, myogenic and neural mechanisms predominate in maintaining blood flow at approximately _______L/min.
At rest, myogenic and neural mechanisms predominate in maintaining blood flow at approximately _______L/min.
Match the following control mechanisms with their effects in the brain:
Match the following control mechanisms with their effects in the brain:
What is the relationship between the velocity of blood flow and total cross-sectional area?
What is the relationship between the velocity of blood flow and total cross-sectional area?
Fluid is forced out of the clefts of capillaries at the arterial end, and most of it returns to the blood at the venous end.
Fluid is forced out of the clefts of capillaries at the arterial end, and most of it returns to the blood at the venous end.
Define hydrostatic pressure (HPc) in the context of capillary transport mechanisms.
Define hydrostatic pressure (HPc) in the context of capillary transport mechanisms.
What is the function of the lymphatic system in removing fluid from the body?
What is the function of the lymphatic system in removing fluid from the body?
What pressures drive fluid flow across a capillary?
What pressures drive fluid flow across a capillary?
At the arteriolar end of a capillary, net filtration pressure (NFP) is __ mm Hg.
At the arteriolar end of a capillary, net filtration pressure (NFP) is __ mm Hg.
At the venous end of a capillary, net reabsorption occurs.
At the venous end of a capillary, net reabsorption occurs.
What are the important differences between systemic arteries and veins?
What are the important differences between systemic arteries and veins?
Which of the following statements are true regarding the venous drainage system in the brain and digestive system? (Select all that apply)
Which of the following statements are true regarding the venous drainage system in the brain and digestive system? (Select all that apply)
Systemic vessels always match symmetrically on the right and left sides of the body.
Systemic vessels always match symmetrically on the right and left sides of the body.
What type of blood vessels carry blood away from the heart?
What type of blood vessels carry blood away from the heart?
Capillaries have direct contact with tissue cells to serve cellular needs.
Capillaries have direct contact with tissue cells to serve cellular needs.
What are the three layers that make up the walls of blood vessels, except for capillaries?
What are the three layers that make up the walls of blood vessels, except for capillaries?
Larger veins are also known as __________ vessels.
Larger veins are also known as __________ vessels.
Match the following blood vessel components with their descriptions:
Match the following blood vessel components with their descriptions:
Flashcards are hidden until you start studying
Study Notes
Blood Vessel Structure and Function
- Blood vessels form a delivery system that works with the lymphatic system to circulate fluids.
- Arteries carry blood away from the heart and are oxygenated, except for pulmonary circulation and umbilical vessels of a fetus.
- Capillaries are responsible for direct contact with tissue cells to serve cellular needs.
- Veins carry blood towards the heart and are deoxygenated, except for pulmonary circulation and umbilical vessels of a fetus.
Venous System and Arterial System
- The venous system has large veins (capacitance vessels) that store blood and smaller veins (capacitance vessels) that branch into capillaries.
- The arterial system has large arteries (elastic arteries) that act as pressure reservoirs and smaller arteries (muscular arteries) that distribute blood to capillaries.
- Lymphatic vessels and nodes are part of the immune system and help defend against infection and disease.
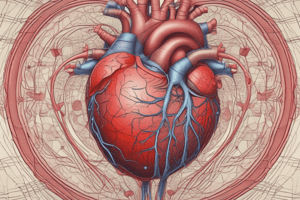
Structure of Blood Vessel Wall
- All vessels, except capillaries, have three layers: tunica intima, tunica media, and tunica externa.
- Tunica intima is the innermost layer, consisting of endothelium and a subendothelial layer.
- Tunica media is the middle layer, composed of smooth muscle and elastic fibers.
- Tunica externa is the outermost layer, made up of collagen fibers and infiltrated with nerve fibers, lymphatic vessels, and tiny blood vessels.
Capillaries
- Capillaries are responsible for exchanging oxygen, nutrients, and waste products between the blood and interstitial fluid.
- Only single red blood cells can pass through capillaries at a time.
- Capillary walls consist of endothelial cells joined by tight junctions with gaps called intercellular clefts.
- Pericytes are spider-shaped stem cells that help stabilize capillary walls, control permeability, and play a role in vessel repair.
Capillary Beds
- Capillary beds are interwoven networks of capillaries between arterioles and venules.
- Microcirculation refers to the flow of blood through capillary beds.
- Capillary beds consist of two types of vessels: vascular shunts and true capillaries.
Veins
- Veins carry blood towards the heart and have larger diameters and thinner walls than arteries.
- Veins are good storage vessels, known as capacitance vessels, which contain up to 65% of the blood supply.
- Veins have adaptations to ensure blood return to the heart, including venous valves and venous sinuses.
Anastomoses
- Anastomoses are interconnections of blood vessels that provide alternate pathways to ensure continuous flow, even if one artery is blocked.
- Arterial anastomoses are common in joints, abdominal organs, brain, and heart, but not in retina, kidneys, or spleen.
Clinical Applications
- Varicose veins are dilated and painful veins due to incompetent valves, often caused by heredity, prolonged standing, obesity, or pregnancy.
- Elevated venous pressure can cause varicose veins, such as hemorrhoids.
Physiology of Circulation
- Blood flow is the volume of blood flowing through a vessel, organ, or entire circulation in a given period.
- Blood pressure is the force per unit area exerted on the wall of a blood vessel by blood.
- Resistance is the opposition to flow, influenced by blood viscosity, total blood vessel length, and blood vessel diameter.
Relationship between Flow, Pressure, and Resistance
- Blood flow is directly proportional to blood pressure gradient and inversely proportional to peripheral resistance.
- Peripheral resistance is more important in influencing local blood flow because it can be easily changed by altering blood vessel diameter.### Arterial Blood Pressure
- Volume of blood forced into arteries at any time: 80 mL
- Blood pressure near the heart is pulsatile
- Systolic pressure: 120 mm Hg (during ventricular contraction)
- Diastolic pressure: 40 mm Hg (when the heart is at rest)
- Pulse pressure: difference between systolic and diastolic pressure
- Pulse: throbbing of arteries due to difference in pulse pressure
Mean Arterial Pressure (MAP)
- Pressure that propels blood to tissues
- Calculated by adding diastolic pressure + 1/3 pulse pressure
- Example: BP = 120/80; Pulse Pressure = 40; MAP = 93 mm Hg
- Both pulse pressure and MAP decline with increasing distance from the heart
Clinical Monitoring of Circulatory Efficiency
- Vital signs: pulse and blood pressure, along with respiratory rate and body temperature
- Taking a pulse: radial pulse (taken at the wrist) is the most routinely used, but there are other clinically important pulse points
- Pressure points: areas where arteries are close to the body surface
- Can be compressed to stop blood flow in the event of hemorrhaging
Measuring Blood Pressure
- Systemic arterial BP is measured indirectly by auscultatory methods using a sphygmomanometer
- Wrap cuff around the arm superior to the elbow
- Increase pressure in the cuff until it exceeds systolic pressure in the brachial artery
- Pressure is released slowly, and the examiner listens for sounds of Korotkoff with a stethoscope
- Systolic pressure: normally less than 120 mm Hg
- Diastolic pressure: normally less than 80 mm Hg
Capillary Blood Pressure
- Ranges from 35 mm Hg at the beginning of the capillary bed to 17 mm Hg at the end of the bed
- Low capillary pressure is desirable because:
- High BP would rupture fragile, thin-walled capillaries
- Most capillaries are very permeable, so low pressure forces filtrate into interstitial spaces
Venous Blood Pressure
- Changes little during the cardiac cycle
- Small pressure gradient, only about 15 mm Hg
- Low pressure is due to the cumulative effects of peripheral resistance
- Adaptations to help with venous return:
- Muscular pump: contraction of skeletal muscles "milks" blood back toward the heart
- Respiratory pump: pressure changes during breathing move blood toward the heart
- Sympathetic venoconstriction: under sympathetic control, smooth muscles constrict, pushing blood back toward the heart
Regulation of Blood Pressure
- Maintaining blood pressure requires cooperation of the brain, heart, blood vessels, and kidneys
- Three main factors regulating blood pressure:
- Cardiac output (CO)
- Peripheral resistance (PR)
- Blood volume
- Formula: MAP = CO × R
Neural Controls
- Operate via reflex arcs that involve:
- Cardiovascular center of medulla
- Baroreceptors
- Chemoreceptors
- Higher brain centers
- Role of the cardiovascular center:
- Composed of clusters of sympathetic neurons in medulla
- Consists of:
- Cardiac centers: cardioinhibitory and cardioacceleratory centers
- Vasomotor center: sends steady impulses via sympathetic efferents called vasomotor fibers to blood vessels
Baroreceptor Reflexes
- Located in carotid sinuses, aortic arch, and walls of large arteries of the neck and thorax
- If MAP is high:
- Increased blood pressure stimulates baroreceptors to increase input to the vasomotor center
- Inhibits vasomotor and cardioacceleratory centers
- Stimulates cardioinhibitory center
- Results in arterial vasodilation and venodilation
- If MAP is low:
- Reflex vasoconstriction is initiated that increases CO and blood pressure
Short-Term Regulation: Hormonal Controls
- Hormones regulate BP in short term via changes in peripheral resistance or long term via changes in blood volume
- Adrenal medulla hormones:
- Epinephrine and norepinephrine from the adrenal gland increase CO and vasoconstriction
- Angiotensin II stimulates vasoconstriction
- Antidiuretic hormone: high levels can cause vasoconstriction
- Atrial natriuretic peptide decreases BP by antagonizing aldosterone, causing decreased blood volume### Long-Term Mechanisms: Renal Regulation
- Chronic high or low blood pressure leads to baroreceptors adapting, making them ineffective for long-term regulation
- Long-term mechanisms control blood pressure by altering blood volume via kidneys
- Kidneys regulate arterial blood pressure through:
- Direct renal mechanism
- Indirect renal mechanism (renin-angiotensin-aldosterone)
Renal Control of Blood Pressure
- Direct renal mechanism:
- Filtration by kidneys
- Urine formation
- Blood volume regulation
- Indirect renal mechanism (renin-angiotensin-aldosterone):
- Renin release from kidneys
- Angiotensin I formation
- Angiotensin converting enzyme (ACE) formation
- Angiotensin II formation
- Aldosterone secretion by adrenal cortex
- Sodium reabsorption and water reabsorption by kidneys
Factors Affecting Mean Arterial Pressure (MAP)
- Activity of muscular pump and respiratory pump
- Release of antinatriuretic peptide (ANP)
- Fluid loss from hemorrhage, excessive sweating, and dehydration
- Crisis stressors: exercise, trauma, and high hematocrit
- Vasomotor tone; bloodborne chemicals (epinephrine, norepinephrine, ADH, and angiotensin II)
Regulation of Blood Pressure
- Homeostatic imbalances in blood pressure:
- Transient elevations in BP occur during changes in posture, physical exertion, emotional upset, and fever
- Age, sex, weight, race, mood, and posture may also cause BP to vary
- Hypertension:
- Sustained elevated arterial pressure of 140/90 mm Hg or higher
- Primary hypertension: 90% of hypertensive conditions; risk factors include heredity, diet, obesity, age, diabetes mellitus, stress, and smoking
- Secondary hypertension: less common; commonly due to obstructed renal arteries, kidney disease, and endocrine disorders
- Hypotension:
- Low blood pressure below 90/60 mm Hg
- Often associated with long life and lack of cardiovascular illness
- Orthostatic hypotension: temporary low BP and dizziness when suddenly rising from sitting or reclining position
- Chronic hypotension: hint of poor nutrition and warning sign for Addison's disease or hypothyroidism
- Acute hypotension: important sign of circulatory shock
Control of Blood Flow
- Functions of blood flow:
- Delivery of O2 and nutrients to, and removal of wastes from, tissue cells
- Gas exchange (lungs)
- Absorption of nutrients (digestive tract)
- Urine formation (kidneys)
- Rate of flow (RF) is precisely right amount to provide proper function to that tissue or organ
- RF is controlled by:
- Extrinsic control: sympathetic nervous system and hormones control blood flow by acting on arteriolar smooth muscle
- Intrinsic control: autoregulation control of blood flow by varying resistance (diameter) of arterioles
Autoregulation: Intrinsic (Local) Regulation of Blood Flow
- Distributes blood flow to individual organs and tissues as needed
- Metabolic or myogenic controls:
- Vasodilators: O2, CO2, H+, K+, prostaglandins, adenosine, nitric oxide, and atrial natriuretic peptide
- Vasoconstrictors: neural or hormonal controls, maintain mean arterial pressure (MAP), and redistribute blood during exercise and thermoregulation
- Long-term autoregulation:
- Occurs when short-term autoregulation cannot meet tissue nutrient requirements
- Number of vessels to region increases (angiogenesis), and existing vessels enlarge
Blood Flow in Special Areas
- Skeletal muscles:
- Blood flow varies with fiber type and activity
- At rest, myogenic and neural mechanisms predominate; maintain flow at ∼1 L/min
- Active or exercise hyperemia: during muscle activity, blood flow increases in direct proportion to metabolic activity
- Brain:
- Blood flow to brain must be constant because neurons are intolerant of ischemia; flow averages ∼750 ml/min
- Control mechanisms: metabolic controls (pH, CO2, and O2) and myogenic controls (MAP)
- Skin:
- Blood flow through venous plexuses below skin surface regulates body temperature
- Flow varies from 50 ml/min to 2500 ml/min, depending on body temperature
- Controlled by sympathetic nervous system reflexes
- Lungs:
- Pulmonary circuit is unusual; pathway is short
- Arteries/arterioles are more like veins/venules (thin-walled, large lumens)
- Autoregulatory mechanisms are opposite; low O2 levels cause vasoconstriction, and high levels promote vasodilation
- Heart:
- Blood flow through heart is influenced by aortic pressures and ventricular pumping
- During ventricular systole, coronary vessels are compressed; myocardial blood flow ceases
- During diastole, high aortic pressure forces blood through coronary circulation
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.