Podcast
Questions and Answers
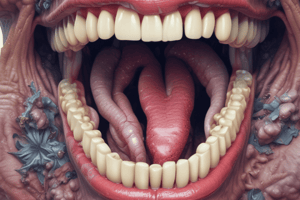
A patient presents with creamy, soft, white plaques in their mouth that can be wiped off, revealing a sore, erythematous base. This presentation is MOST indicative of which condition?
A patient presents with creamy, soft, white plaques in their mouth that can be wiped off, revealing a sore, erythematous base. This presentation is MOST indicative of which condition?
- Median Rhomboid Glossitis
- Chronic Atrophic Candidosis
- Acute Pseudomembranous Candidosis (correct)
- Chronic Hyperplastic Candidosis
Which diagnostic method is MOST suitable for identifying Candida infections in the oral cavity?
Which diagnostic method is MOST suitable for identifying Candida infections in the oral cavity?
- Aspirate Sample
- Antimicrobial Discs
- Oral Rinse (correct)
- Swabs
A patient wearing dentures complains of redness and irritation directly underneath the appliance. What condition is MOST likely causing these symptoms?
A patient wearing dentures complains of redness and irritation directly underneath the appliance. What condition is MOST likely causing these symptoms?
- Angular Cheilitis
- Chronic Atrophic Candidosis (correct)
- Acute Atrophic Candidosis
- Chronic Hyperplastic Candidosis
A dentist notes cracking and inflammation at the corners of a patient's mouth. Which condition is MOST likely associated with these findings?
A dentist notes cracking and inflammation at the corners of a patient's mouth. Which condition is MOST likely associated with these findings?
What is the MOST appropriate initial management strategy for a patient diagnosed with acute atrophic candidosis?
What is the MOST appropriate initial management strategy for a patient diagnosed with acute atrophic candidosis?
Which of the following characteristics is MOST indicative of chronic hyperplastic candidosis?
Which of the following characteristics is MOST indicative of chronic hyperplastic candidosis?
An asymptomatic erythematous, well-demarcated lesion is noted on the midline of the dorsal tongue during a routine dental exam. Which condition does this BEST describe?
An asymptomatic erythematous, well-demarcated lesion is noted on the midline of the dorsal tongue during a routine dental exam. Which condition does this BEST describe?
After obtaining a swab from the oral mucosa, what is the PRIMARY reason for using antimicrobial discs with sensitivity tests?
After obtaining a swab from the oral mucosa, what is the PRIMARY reason for using antimicrobial discs with sensitivity tests?
A patient presents with painful, bleeding gums and necrotic patches. Which bacterial infection is MOST likely the cause?
A patient presents with painful, bleeding gums and necrotic patches. Which bacterial infection is MOST likely the cause?
Which of the following is the MOST appropriate initial treatment for a patient diagnosed with acute bacterial sialadenitis?
Which of the following is the MOST appropriate initial treatment for a patient diagnosed with acute bacterial sialadenitis?
What is the MOST appropriate management strategy for a patient diagnosed with oral actinomycosis?
What is the MOST appropriate management strategy for a patient diagnosed with oral actinomycosis?
A patient presents with red sores that have ruptured and formed honey-colored crusts around the mouth. Which treatment approach is MOST suitable for this condition?
A patient presents with red sores that have ruptured and formed honey-colored crusts around the mouth. Which treatment approach is MOST suitable for this condition?
A patient presents with a sore throat, fever, and redness, but no visible oral lesions. The physician suspects an oral manifestation of a sexually transmitted infection. Which test is MOST appropriate for confirming a Gonorrhea infection?
A patient presents with a sore throat, fever, and redness, but no visible oral lesions. The physician suspects an oral manifestation of a sexually transmitted infection. Which test is MOST appropriate for confirming a Gonorrhea infection?
What distinguishes Herpes Simplex Virus (HSV) infections from Varicella Zoster Virus (VZV) infections in the oral cavity?
What distinguishes Herpes Simplex Virus (HSV) infections from Varicella Zoster Virus (VZV) infections in the oral cavity?
A patient exhibits white patches on the tongue that cannot be wiped away, along with a sore throat, fever, and swollen lymph nodes. Which viral infection is the MOST likely cause of these combined symptoms?
A patient exhibits white patches on the tongue that cannot be wiped away, along with a sore throat, fever, and swollen lymph nodes. Which viral infection is the MOST likely cause of these combined symptoms?
How does the management of mumps differ from the management of measles?
How does the management of mumps differ from the management of measles?
A child presents with multiple painless papules in the oral cavity. Which Human Papillomavirus (HPV)-related condition is MOST likely causing these symptoms?
A child presents with multiple painless papules in the oral cavity. Which Human Papillomavirus (HPV)-related condition is MOST likely causing these symptoms?
Which of the following oral manifestations is MOST commonly associated with Human Immunodeficiency Virus (HIV) infection due to immunodeficiency?
Which of the following oral manifestations is MOST commonly associated with Human Immunodeficiency Virus (HIV) infection due to immunodeficiency?
A patient presents with a painless chancre on their lip. Which stage of syphilis does this lesion MOST likely indicate?
A patient presents with a painless chancre on their lip. Which stage of syphilis does this lesion MOST likely indicate?
A patient presents with gummas and exhibits neurological symptoms. What stage of syphilis has the patient MOST likely progressed to?
A patient presents with gummas and exhibits neurological symptoms. What stage of syphilis has the patient MOST likely progressed to?
Which of the following is the MOST critical management strategy for congenital syphilis?
Which of the following is the MOST critical management strategy for congenital syphilis?
A child presents with sudden onset of fever, anorexia, and small ulcers at the back of the mouth on the soft palate, tonsils, and uvula. Which condition is MOST likely?
A child presents with sudden onset of fever, anorexia, and small ulcers at the back of the mouth on the soft palate, tonsils, and uvula. Which condition is MOST likely?
A patient is diagnosed with Chronic Mucocutaneous Candidiasis (CMC). What is the MOST important aspect of managing this syndrome effectively?
A patient is diagnosed with Chronic Mucocutaneous Candidiasis (CMC). What is the MOST important aspect of managing this syndrome effectively?
A periodontist is collecting samples for lab testing from a deep periodontal pocket. Which method is MOST suitable for sample collection in this scenario?
A periodontist is collecting samples for lab testing from a deep periodontal pocket. Which method is MOST suitable for sample collection in this scenario?
Which of the following factors is MOST crucial in preventing recurrence of chronic atrophic candidosis (denture stomatitis)?
Which of the following factors is MOST crucial in preventing recurrence of chronic atrophic candidosis (denture stomatitis)?
A patient presents with a persistent, white plaque on the lateral border of the tongue that does not wipe off. Which of the following steps should be prioritized?
A patient presents with a persistent, white plaque on the lateral border of the tongue that does not wipe off. Which of the following steps should be prioritized?
When managing a patient with median rhomboid glossitis, what is the PRIMARY treatment focus?
When managing a patient with median rhomboid glossitis, what is the PRIMARY treatment focus?
A patient complains of painful cracking at the corners of their mouth. Upon examination, you notice fissuring and mild inflammation. Which of the following approaches is MOST appropriate for initial management?
A patient complains of painful cracking at the corners of their mouth. Upon examination, you notice fissuring and mild inflammation. Which of the following approaches is MOST appropriate for initial management?
What is the MOST critical step in managing chronic pseudomembranous candidosis in an immunocompromised patient?
What is the MOST critical step in managing chronic pseudomembranous candidosis in an immunocompromised patient?
A patient who recently completed a long course of broad-spectrum antibiotics presents with generalized red patches on their tongue, without any visible white plaques. What is the MOST likely cause?
A patient who recently completed a long course of broad-spectrum antibiotics presents with generalized red patches on their tongue, without any visible white plaques. What is the MOST likely cause?
A dental professional suspects a candida infection in their patient and decides to perform sensitivity tests with antimicrobial discs after obtaining a swab from the oral mucosa. What is the PRIMARY purpose of this approach?
A dental professional suspects a candida infection in their patient and decides to perform sensitivity tests with antimicrobial discs after obtaining a swab from the oral mucosa. What is the PRIMARY purpose of this approach?
Which of the following is the PRIMARY focus in managing Chronic Mucocutaneous Candidiasis (CMC)?
Which of the following is the PRIMARY focus in managing Chronic Mucocutaneous Candidiasis (CMC)?
What is the MOST important aspect of managing Herpes Simplex Virus (HSV) outbreaks?
What is the MOST important aspect of managing Herpes Simplex Virus (HSV) outbreaks?
In severe cases of Varicella Zoster Virus (VZV) infections, what medication might be considered in addition to acyclovir?
In severe cases of Varicella Zoster Virus (VZV) infections, what medication might be considered in addition to acyclovir?
What is the PRIMARY approach to managing infectious mononucleosis caused by the Epstein-Barr Virus (EBV)?
What is the PRIMARY approach to managing infectious mononucleosis caused by the Epstein-Barr Virus (EBV)?
What is the PRIMARY treatment for Cytomegalovirus (CMV) infections?
What is the PRIMARY treatment for Cytomegalovirus (CMV) infections?
What is the MOST effective treatment approach for Necrotizing Ulcerative Gingivitis (NUG)?
What is the MOST effective treatment approach for Necrotizing Ulcerative Gingivitis (NUG)?
A patient presents with a painless chancre on their lip. What is the MOST appropriate next step in management?
A patient presents with a painless chancre on their lip. What is the MOST appropriate next step in management?
Which of the following is the MOST effective strategy for preventing congenital syphilis?
Which of the following is the MOST effective strategy for preventing congenital syphilis?
What is the PRIMARY treatment approach for tuberculosis when oral manifestations are present?
What is the PRIMARY treatment approach for tuberculosis when oral manifestations are present?
A patient presents with acute bacterial sialadenitis. Besides antibiotics, what additional measure is MOST important in managing this condition?
A patient presents with acute bacterial sialadenitis. Besides antibiotics, what additional measure is MOST important in managing this condition?
What is the INITIAL treatment for oral actinomycosis?
What is the INITIAL treatment for oral actinomycosis?
What is the MOST appropriate treatment for impetigo?
What is the MOST appropriate treatment for impetigo?
What diagnostic step is especially important in managing Gonorrhea?
What diagnostic step is especially important in managing Gonorrhea?
What is the PRIMARY focus of managing mumps?
What is the PRIMARY focus of managing mumps?
What is the typical management for oral squamous cell papillomas caused by HPV?
What is the typical management for oral squamous cell papillomas caused by HPV?
Flashcards
Acute Pseudomembranous Candidosis (Thrush)
Acute Pseudomembranous Candidosis (Thrush)
Creamy, soft, white plaques on the oral mucosa that can be wiped off, revealing a sore, red base.
Chronic Pseudomembranous Candidosis
Chronic Pseudomembranous Candidosis
Similar to acute thrush, but more painful and occurs in immunocompromised patients.
Acute Atrophic Candidosis
Acute Atrophic Candidosis
Generalized red, desquamative areas without white plaques.
Chronic Atrophic Candidosis (Denture Stomatitis)
Chronic Atrophic Candidosis (Denture Stomatitis)
Signup and view all the flashcards
Chronic Hyperplastic Candidosis (Candida Leukoplakia)
Chronic Hyperplastic Candidosis (Candida Leukoplakia)
Signup and view all the flashcards
Median Rhomboid Glossitis
Median Rhomboid Glossitis
Signup and view all the flashcards
Angular Cheilitis
Angular Cheilitis
Signup and view all the flashcards
Chronic Mucocutaneous Candidosis (CMC)
Chronic Mucocutaneous Candidosis (CMC)
Signup and view all the flashcards
Acute Herpetic Gingivostomatitis
Acute Herpetic Gingivostomatitis
Signup and view all the flashcards
Herpes Labialis
Herpes Labialis
Signup and view all the flashcards
Shingles
Shingles
Signup and view all the flashcards
Oral Hairy Leukoplakia
Oral Hairy Leukoplakia
Signup and view all the flashcards
Necrotizing Ulcerative Gingivitis
Necrotizing Ulcerative Gingivitis
Signup and view all the flashcards
Primary Syphilis
Primary Syphilis
Signup and view all the flashcards
Secondary Syphilis
Secondary Syphilis
Signup and view all the flashcards
Tertiary Syphilis
Tertiary Syphilis
Signup and view all the flashcards
Congenital Syphilis
Congenital Syphilis
Signup and view all the flashcards
Acute Bacterial Sialadenitis
Acute Bacterial Sialadenitis
Signup and view all the flashcards
Actinomycosis
Actinomycosis
Signup and view all the flashcards
Impetigo
Impetigo
Signup and view all the flashcards
Mumps
Mumps
Signup and view all the flashcards
Herpangina
Herpangina
Signup and view all the flashcards
Aspirate Sample
Aspirate Sample
Signup and view all the flashcards
Swab Sample
Swab Sample
Signup and view all the flashcards
Oral Rinse Sample
Oral Rinse Sample
Signup and view all the flashcards
Sensitivity Tests
Sensitivity Tests
Signup and view all the flashcards
Chronic Atrophic Candidosis/Denture Stomatitis
Chronic Atrophic Candidosis/Denture Stomatitis
Signup and view all the flashcards
Shingles (Herpes Zoster)
Shingles (Herpes Zoster)
Signup and view all the flashcards
Necrotizing Ulcerative Gingivitis (NUG)
Necrotizing Ulcerative Gingivitis (NUG)
Signup and view all the flashcards
Measles
Measles
Signup and view all the flashcards
Squamous Cell Papilloma
Squamous Cell Papilloma
Signup and view all the flashcards
Study Notes
Diagnostic Methods for Oral Infections
- Aspirate samples are used for fluid-filled cavities like dental abscesses
- Broad-spectrum antibiotics (e.g., amoxicillin) are typically used empirically
- Paper points may be used by periodontists for lab testing
- Swabs are a common method, especially for clean mucosa
- Swabs may be moistened or dried based on the site characteristics
- Sensitivity tests with antimicrobial discs help determine appropriate antibiotics
- Oral Rinse is primarily used for diagnosing Candida infections
- Patients rinse with sterile saline, which is then analyzed in the lab
Candida Infections
- Oral infections caused by Candida species, typically Candida albicans
Acute Pseudomembranous Candidosis (Thrush)
- Creamy, soft, white plaques can be wiped off to reveal an erythematous, sore background
- Commonly seen in infants and women
- Often associated with angular cheilitis
- Management includes good oral hygiene and antifungal treatments like miconazole or nystatin; treat associated angular cheilitis
Chronic Pseudomembranous Candidosis
- Similar to the acute form but more painful
- Occurs in immunocompromised patients
- Management involves antifungal treatments and addressing underlying immunocompromised conditions
Acute Atrophic Candidosis
- Generalized desquamative areas appear as diffuse red patches without white plaque
- Management involves stopping causative antibiotics or steroids, improving oral hygiene, and using topical antifungal therapy
Chronic Atrophic Candidosis (Denture Stomatitis) or Erythematous Candidosis (Non-Denture)
- Red, velvet-like lesions appear under dentures or in non-denture wearers
- Management includes antifungals, good denture hygiene, removing dentures at night, and possibly replacing ill-fitting dentures
Chronic Hyperplastic Candidosis or Candida Leukoplakia
- Thick, white, painful plaques are difficult to remove
- Requires biopsy for diagnosis
- Management includes antifungal therapy and addressing contributing factors like smoking or iron deficiency
Median Rhomboid Glossitis
- Asymptomatic, erythematous, well-demarcated area is present on the midline of the dorsal tongue
- Management involves antifungals and addressing any contributing factors like corticosteroid use or smoking
Angular Cheilitis
- Cracking appears at the corners of the mouth, sometimes with Candida or bacterial infection
- Management involves an appropriate topical antifungal or antibiotic
- Consider underlying factors like denture fit or nutritional deficiencies
Chronic Mucocutaneous Candidosis Syndromes (CMC)
- Persistent Candida infections occur on the skin, nails, oral, and genital mucosa
- Management involves long-term antifungal therapy, possibly combined with treatments for associated disorders like immunoglobulin or stem cell transplantation
Viral Infections
- Infections caused by various viruses affecting the oral cavity and surrounding tissues
Herpes Simplex Virus (HSV)
- Types include acute herpetic gingivostomatitis and herpes labialis
- Acute Herpetic Gingivostomatitis: Severe oral soreness, fever, swollen lymph nodes
- Herpes Labialis: Cold sores with burning sensation before blistering
- Management: Antivirals like acyclovir during outbreaks, and supportive care, including hydration and pain management
Varicella Zoster Virus
- Types include chickenpox and shingles
- Chickenpox: Oral and body lesions
- Shingles: Painful rash along dermatomes, possibly involving the face
- Management: Acyclovir and possibly steroids for severe cases, pain management for post-herpetic neuralgia
Epstein-Barr Virus (EBV)
- Associated with infectious mononucleosis, oral hairy leukoplakia, nasopharyngeal carcinoma, and Burkitt lymphoma
- Infectious Mononucleosis: Sore throat, fever, swollen lymph nodes
- Oral Hairy Leukoplakia: White patches on the tongue that cannot be wiped away
- Management: Mostly supportive; antivirals may reduce symptoms but do not alter the course
Cytomegalovirus (CMV)
- Rare in healthy individuals, may cause mouth ulcers and retinitis
- Management: Antiviral treatments like ganciclovir
Bacterial Infections
- Infections caused by bacteria, leading to various oral and systemic manifestations
Necrotizing Ulcerative Gingivitis
- Painful, bleeding gums with necrotic patches
- Management: Improved oral hygiene and antibiotic therapy like metronidazole
Syphilis
- Primary Syphilis:
- Painless chancre at the infection site
- Management: Treated with penicillin to prevent progression
- Secondary Syphilis:
- Rashes, especially on palms and soles, mucous patches, fever, and swollen lymph nodes
- Management: Penicillin treatment continues; additional care for symptom relief may be necessary
- Tertiary Syphilis:
- Gummas (painful ulcers), neurological, or cardiovascular symptoms
- Management: Requires longer durations of antibiotic therapy, possibly including hospitalization for intensive care
- Congenital Syphilis:
- Occurs in infants born to infected mothers, can cause multiple organ malformations
- Management: Prevention is key via prenatal screening and treatment of the mother; infants need antibiotic therapy
Tuberculosis
- Oral manifestations are rare, but may include painful ulcers, nodules, or fissures
- Management: Antitubercular therapy in coordination with medical specialists, particularly if pulmonary TB is also present
Acute Bacterial Sialadenitis
- Painful swelling of the salivary glands, potentially with pus
- Management: Hydration, antibiotics, and possibly surgical intervention to remove blockages
Actinomycosis
- Rare oral infections are characterized by abscesses and sinus tract formation
- Management: Surgical drainage and prolonged antibiotic therapy, typically with amoxicillin or ceftriaxone
Impetigo
- Red sores that quickly rupture and form honey-colored crusts
- Management: Antibiotic creams or oral antibiotics, and hygiene measures to prevent spread
Gonorrhea
- May include a sore throat, redness in the throat, and fever; oral lesions are less common
- Management: Antibiotics, with confirmation of diagnosis by culture or smear to ensure appropriate treatment
Paramyxoviruses
- Viral infections caused by paramyxoviruses
Mumps
- Swelling of the parotid glands, sometimes accompanied by orchitis or meningoencephalitis
- Management: Supportive care, as there is no specific treatment for mumps
Measles
- Koplik spots inside the mouth, fever, conjunctivitis, and a characteristic red-brown rash
- Management: Supportive care, vitamin A supplements, and monitoring for complications
Human Papillomavirus (HPV)
- Viral infection that can cause several oral manifestations
Oral Manifestations
- Squamous Cell Papilloma: Warty growths due to HPV types 6 and 11
- Condyloma Acuminatum: Pink nodules with a cauliflower appearance
- Heck's Disease (Focal Epithelial Hyperplasia): Multiple painless papules, often in children and immunocompromised individuals
- Verruca Vulgaris: Common warts with a rough surface
- Management: Surgical excision of papillomas, monitoring for potential malignancy, especially with HPV types 16 and 18 related to oropharyngeal carcinoma
Human Immunodeficiency Virus (HIV) Related Infections
- Increased susceptibility to infections like candidiasis, herpes zoster, and oral hairy leukoplakia due to immunodeficiency
- Management: Highly active antiretroviral therapy (HAART) has significantly reduced the incidence of these infections, but supportive care and specific treatments for oral lesions are necessary
Coxsackie Infections
- Viral infections caused by Coxsackieviruses
- Coxsackieviruses are a group of enteroviruses that consist of RNA viruses
- Two notable diseases caused by different strains of Coxsackie A virus are Herpangina and Hand, Foot, and Mouth Disease (HFMD)
- Both conditions predominantly affect children and are transmitted primarily via the feco-oral route
Herpangina
- Caused by Coxsackievirus A, typically affecting children
- Transmission is via the oro-faecal route
- Symptoms: Sudden onset of mild illness with fever, anorexia, dysphagia, and sore throat
- Small vesicles develop into ulcers (1-2mm in diameter) located at the back of the mouth, including the tonsils, soft palate, and uvula, lesions typically last 2-3 days
- Can be difficult to distinguish from acute primary herpes, which usually involves the anterior oral regions, whereas herpangina affects more posterior areas of the mouth
- Management: Supportive care, including mouth rinses with topical analgesics along with antipyretic analgesics to manage fever
Hand, Foot, and Mouth Disease (HFMD)
- Caused by various types of Coxsackievirus A, often type 16
- Transmission is via close contact, common in children
- Symptoms: Small, scattered ulcers more anteriorly than herpangina, often presenting as shallow painful ulcers, and rarely intact vesicles and lesions typically appear on the palms of the hands and soles of the feet
- Management: Primarily supportive, resolving within 7 days
- This disease is not the same as the foot-and-mouth disease found in cattle
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.