Podcast
Questions and Answers
What is the brachial plexus?
What is the brachial plexus?
A complex network of nerves that supplies motor and sensory innervation to the upper limb.
How many roots does the brachial plexus have?
How many roots does the brachial plexus have?
Five
What are the components of the brachial plexus?
What are the components of the brachial plexus?
- Five roots
- Three trunks
- Six divisions
- All of the above (correct)
What are the three trunks of the brachial plexus?
What are the three trunks of the brachial plexus?
Which nerve innervates the Biceps Brachii?
Which nerve innervates the Biceps Brachii?
The musculocutaneous nerve is responsible for sensory innervation only.
The musculocutaneous nerve is responsible for sensory innervation only.
What is the clinical significance of an injury to the musculocutaneous nerve?
What is the clinical significance of an injury to the musculocutaneous nerve?
What muscles does the axillary nerve innervate?
What muscles does the axillary nerve innervate?
What area does the axillary nerve supply sensory innervation to?
What area does the axillary nerve supply sensory innervation to?
Axillary nerve injury can result in difficulty abducting the arm.
Axillary nerve injury can result in difficulty abducting the arm.
What is the origin of the median nerve?
What is the origin of the median nerve?
Flashcards are hidden until you start studying
Study Notes
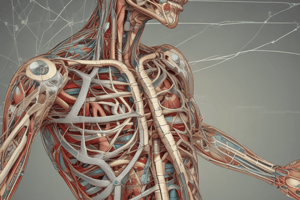
Brachial Plexus Structure
- The Brachial Plexus is a network of nerves that supplies the upper limb
- It is divided into roots, trunks, divisions, cords and branches.
- The five roots are the anterior rami of spinal nerves C5, C6, C7, C8 and T1.
- Roots combine to form three trunks:
- Superior trunk (C5 and C6)
- Middle trunk (C7)
- Inferior trunk (C8 and T1)
- Trunks split into six divisions:
- Three anterior and three posterior
- Divisions regroup into three cords:
- Lateral cord (from superior and middle trunk anterior divisions)
- Posterior cord (from all posterior divisions)
- Medial cord (from inferior trunk anterior division)
Branches
- There are five terminal branches and several pre-terminal or collateral branches
- Terminal branches are:
- Musculocutaneous nerve (from lateral cord)
- Axillary nerve (from posterior cord)
- Radial nerve (from posterior cord)
- Median nerve (from lateral and medial cords)
- Ulnar nerve (from medial cord)
Musculocutaneous Nerve
- Originates from C5, C6 and C7 spinal nerve roots
- Motor function:
- Coracobrachialis: assists with arm flexion and adduction
- Biceps brachii: flexes and supinates forearm
- Brachialis: flexes the forearm
- Sensory function: supplies sensation to lateral forearm
- Clinical significance:
- Injury can cause weakened flexion and supination of the forearm and sensory loss in the lateral forearm
- May be injured due to trauma or compression in the axilla
Axillary Nerve
- Origin: posterior cord (C5 and C6)
- Course: passes through the quadrangular space, winds around the surgical neck of the humerus
- Motor function:
- Deltoid: abduction of arm beyond 15 degrees
- Teres minor: assists with lateral rotation of the arm
- Sensory function:
- Supplies sensation to the skin over the deltoid
- Clinical significance:
- Commonly injured in fractures of the surgical neck of the humerus or anterior shoulder dislocations
- Motor deficits: weakness or paralysis of the deltoid leading to difficulty abducting the arm
- Sensory deficits: sensory loss or alteration over the deltoid region (regimental badge area)
- Quadrangular space syndrome can compress the nerve, leading to pain and weakness in the shoulder
Median Nerve
- Origin: lateral cord (C5, C6, C7) and medial cord (C8, T1)
- Motor function:
- Pronator teres: pronates forearm
- Flexor carpi radialis: flexes and abducts wrist
- Palmaris longus: flexes wrist
- Flexor digitorum superficialis: flexes middle phalanges of fingers 2-5
- Flexor digitorum profundus (lateral half): flexes distal phalanges of fingers 2 and 3
- Abductor pollicis brevis: abducts thumb
- Opponens pollicis: opposes thumb
- Flexor pollicis brevis: flexes thumb
- Lumbricals (2 and 3): flexes metacarpophalangeal joints and extends interphalangeal joints of fingers 2-3
- Sensory function:
- Supplies sensation to palmar aspect of thumb, index, middle and radial half of ring finger
- Also supplies sensation to dorsal aspect of distal phalanges of index and middle finger
- Clinical significance:
- Injury can lead to weakness in hand and forearm muscles causing difficulty with fine motor movements, grasping, and pronation.
- Commonly injured:
- In the carpal tunnel
- At the elbow
- In the forearm
- During surgical procedures
Radial Nerve
- Origin: posterior cord
- Motor function:
- Triceps brachii: extends elbow
- Anconeus: extends elbow and stabilizes elbow joint
- Brachioradialis: flexes elbow and supinates forearm
- Extensor carpi radialis longus: extends and abducts wrist
- Extensor carpi radialis brevis: extends and abducts wrist
- Extensor digitorum: extends fingers 2-5
- Extensor digiti minimi: extends little finger
- Extensor carpi ulnaris: extends and adducts wrist
- Supinator: supinates forearm
- Abductor pollicis longus: abducts and extends thumb
- Extensor pollicis brevis: extends thumb metacarpophalangeal joint
- Extensor pollicis longus: extends thumb interphalangeal joint
- Sensory function:
- Supplies sensation to dorsal aspect of hand and fingers, except the medial one and a half fingers
- Clinical significance:
- Injury causes wrist drop (inability to extend the wrist), loss of sensation in the affected area, and weakness in forearm and hand muscles.
- Commonly injured:
- At the humerus (e.g., midshaft fractures)
- At the elbow
- In the forearm
Ulnar Nerve
- Origin: medial cord (C8 and T1)
- Motor function:
- Flexor carpi ulnaris: flexes and adducts wrist
- Flexor digitorum profundus (medial half): flexes distal phalanges of fingers 4 and 5
- Hypothenar muscles (abductor digiti minimi, flexor digiti minimi, opponens digiti minimi): control the little finger
- Interossei muscles: adduct and abduct fingers
- Lumbricals (4 and 5): flexes metacarpophalangeal joints and extends interphalangeal joints of fingers 4 and 5
- Adductor pollicis: adducts thumb
- Sensory function:
- Supplies sensation to the palmar and dorsal aspects of the little finger and the medial half of the ring finger
- Clinical significance:
- Injury can result in claw hand deformity, altered sensation in the little finger and half of the ring finger, weakness in hand muscles, and difficulty with fine motor movements.
- Commonly injured:
- At the elbow (funny bone)
- At the wrist
- In the forearm
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.