Podcast
Questions and Answers
Primary osteoporosis can be primarily attributed to a decline in mineral content without any genetic influence.
Primary osteoporosis can be primarily attributed to a decline in mineral content without any genetic influence.
False (B)
Osteomalacia is defined as a condition characterized by inadequate mineralization of the bone matrix, leading to potential pain in areas such as the femoral neck.
Osteomalacia is defined as a condition characterized by inadequate mineralization of the bone matrix, leading to potential pain in areas such as the femoral neck.
True (A)
Secondary hyperparathyroidism is usually associated with decreased filtration of calcium due to renal failure, rather than an increase in phosphate levels.
Secondary hyperparathyroidism is usually associated with decreased filtration of calcium due to renal failure, rather than an increase in phosphate levels.
False (B)
Corticosteroids can lead to secondary osteoporosis by inhibiting osteoblastic activity and impairing vitamin D-dependent intestinal calcium absorption.
Corticosteroids can lead to secondary osteoporosis by inhibiting osteoblastic activity and impairing vitamin D-dependent intestinal calcium absorption.
Rickets is characterized by the presence of closed epiphyseal plates in children, leading to abnormal bone development.
Rickets is characterized by the presence of closed epiphyseal plates in children, leading to abnormal bone development.
Osteomyelitis can be caused by Staphylococcus, streptococcus, and Neisseria gonorrhea.
Osteomyelitis can be caused by Staphylococcus, streptococcus, and Neisseria gonorrhea.
Osteoarthritis is primarily classified as an inflammatory disease affecting the articular cartilage.
Osteoarthritis is primarily classified as an inflammatory disease affecting the articular cartilage.
Septicemia is a complication that can arise from osteomyelitis.
Septicemia is a complication that can arise from osteomyelitis.
The appearance of eburnated bone indicates a temporary stage in osteoarthritis.
The appearance of eburnated bone indicates a temporary stage in osteoarthritis.
Chronic overuse and metabolic conditions can contribute to osteoarthritis.
Chronic overuse and metabolic conditions can contribute to osteoarthritis.
Flashcards are hidden until you start studying
Study Notes
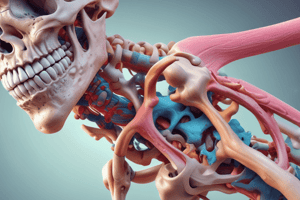
Osteoporosis
- Reduction in bone mass per unit of bone volume
- Metabolic bone disease with normal mineral to matrix ratio
- Primarily categorized into primary and secondary forms
Primary Osteoporosis
- Most common type
- Etiology is uncertain
- Occurs often in postmenopausal women and elderly persons
- Influenced by genetics, estrogen levels, and age
- Factors that can prevent the disease include calcium intake (800mg/day), exercise, and an active lifestyle
- Smoking can lead to estrogen deficiency and potentially cause osteoporosis
Osteopenia
- Decrease in cortical bone thickness
- Reduction in the number and size of bone trabeculae
- Fractures can be an initial sign
- Compression fractures of vertebrae are a common occurrence
Secondary Osteoporosis
- Corticosteroids can lead to osteoporosis due to:
- Inhibition of osteoblastic activity
- Impaired vitamin D-dependent intestinal calcium absorption (secondary hyperparathyroidism)
- Hematologic malignancies are also a cause
- Malabsorption related to gastrointestinal and liver diseases
- Alcoholism leads to osteoporosis due to:
- Inhibition of osteoblasts
- Decreased calcium absorption
Osteomalacia and Rickets
- Inadequate mineralization of newly formed bone matrix (osteomalacia)
- Rickets is a similar condition occurring in children, where it affects epiphyseal plates and cartilage
- Clinical signs of Rickets include:
- Beaded appearance of costochondral junctions
- Pectus carinatum
- Dental abnormalities
- Causes include:
- Vitamin D deficiency (dependent osteomalacia)
- Phosphate deficiency (resistant osteomalacia)
- Defects in mineralization process
Osteomalacia and Rickets: Clinical Presentation
- Osteopenia
- Exaggeration of osteoid seams
- Poorly localized pain
- Pain in the femoral neck, pubic ramus, spine, and ribs
Hyperparathyroidism
- Caused by parathyroid adenoma, hyperplasia, or rare malignancy
- Parathyroid hormone is crucial for bone health and plays a role in:
- Phosphate excretion in urine
- Stimulation of osteoclastic activity leading to hypercalcemia
- Calcium reabsorption in the renal tubules
- Phosphate excretion in the renal tubules
- Stimulation of intestinal calcium absorption
###Hyperparathyroidism: Clinical Features
- Stones: Kidney stones are a common finding.
- Bones: Bone lesions known as "brown tumors" may develop.
- Psychiatric depression may occur.
- Gastrointestinal tract irregularities.
Secondary Hyperparathyroidism:
- Associated with renal osteodystrophy
- Chronic renal failure plays a central role in this process.
- Renal failure leads to:
- Decreased phosphate filtration, resulting in hyperphosphatemia
- Impaired active vitamin D production
- Decreased calcium absorption in the gastrointestinal tract, causing hypocalcemia
- All these factors contribute to secondary hyperparathyroidism.
Osteomyelitis
- Inflammation of bone caused by an infectious organism
- Commonly caused by bacteria such as Staphylococcus, Streptococcus, Escherichia coli, Neisseria gonorrhoeae, Haemophilus influenzae, and Salmonella
- Can occur through:
- Direct penetration: Open wounds, fractures, surgery
- Hematogenous spread: Through the bloodstream, often involving the metaphyses (e.g., knee, ankle, hip)
Osteomyelitis: Complications
- Septicemia (blood poisoning)
- Acute bacterial arthritis
- Pathologic fractures
- Squamous cell carcinoma
- Amyloidosis
- Chronic osteomyelitis
Arthritis - Introduction
- Inflammation of joints
- Frequent site for autoimmune injury
- Can also be caused by infections, degeneration (age, stress, lifestyle), and exposure of hidden antigens
Arthritis - Clinical Features
- Pain: Related to inflammation of the capsule, synovium, and periosteum.
- Swelling: Occurs due to inflammation, effusion, and synovial proliferation.
- Restricted movement: Stems from pain, fluid accumulation, synovial swelling, and damage.
- Deformity: Can arise from misalignment, erosion, and ankylosis (joint fusion).
Osteoarthritis
- Most common joint disease
- Slow progressive degeneration of articular cartilage
- Predominantly affects weight-bearing joints (e.g., knees, hips) and the fingers
- Primary osteoarthritis: Defect in cartilage itself, not an inflammatory disease
- Secondary osteoarthritis: Resulting from trauma, crystal deposits, or infection.
- Interphalangeal joints (fingers), knees, hips, cervical and lumbar spine are frequently affected.
Osteoarthritis: Pathology
- Narrowing of the joint space (loss of cartilage)
- Increased thickness of subchondral bone: Known as eburnated bone
- Subchondral bone cysts
- Osteophytes: Bone spurs, also known as Heberden nodes, commonly found on the fingers at the distal interphalangeal joints.
Osteoarthritis: Causes
- Primary osteoarthritis: Due to unknown factors.
- Secondary osteoarthritis:
- Intra-articular fracture
- Previous infective arthritis
- Rheumatoid arthritis
- Congenital dislocation of the hip
- Abnormal stresses:
- Paget's disease: With associated deformity.
- Chronic overuse
- Metabolic and endocrine disorders:
- Hemochromatosis
- Gout
- Calcium phosphate deposition
- Neuropathic disorders:
- Peripheral neuropathy: As seen in diabetes mellitus.
- Intra-articular corticosteroid overuse
Osteoarthritis: Radiographic Findings
- Narrowing of the joint space: Due to cartilage loss
- Osteophyte formation: Bone spurs
- Cyst formation: Subchondral cysts
- Subchondral sclerosis: Hardening of the bone beneath the cartilage
- Sclerosis, ankylosis, and deformity may be present in advanced cases.
Rheumatoid Arthritis (RA)
- Systemic chronic inflammatory disease
- Autoimmune disease
- Primarily affects diarthrodial joints bilaterally
- STARTS AS SYNOVIAL DISEASE (inflammation of the lining of the joint)
- 3:1 female predominance
- Characterized by remissions and exacerbations
- Heredity plays a role, and Epstein-Barr virus (EBV) has been implicated.
RA - Pathogenesis (Theory)
- Genetically susceptible patient: Individuals with specific genetic markers.
- Infection: Potentially triggered by an infection (e.g., EBV).
- Formation of antibodies: The body produces antibodies against its own tissues.
- Antibodies act as new antigens: These antibodies can trigger further immune responses.
- Production of rheumatoid factor: An antibody that targets immunoglobulin G (IgG).
- Deposits of immune complexes in the synovium: These complexes contribute to inflammation.
- Activation of the complement cascade: Part of the immune system, leading to inflammation.
- Inflammation: The joint becomes inflamed.
- Activation of macrophages: Immune cells contribute to inflammation and tissue damage.
- Homing of T cells: Immune cells that contribute to the inflammatory process.
- Secretion of cytokines: Proteins that further promote inflammation.
RA: Definition
- Chronic, multisystem autoimmune inflammatory disorder
- Primarily affects joints leading to proliferative synovitis
- Progresses to destruction of articular cartilage and ankylosis (joint fusion)
- Etiology:
- Genetic susceptibility: Strong association with HLA-DR4 or DR1 in 65% to 80% of cases.
- Microbial inciting agents: Including Epstein-Barr virus, Borrelia, and Mycoplasma.
- Autoimmunity:
- Rheumatoid factor (IgM anti-IgG): A hallmark antibody found in many patients.
- Helper T cells (CD4): Target type II collagen and cartilage glycoprotein-39.
RA: Pathology
- Inflammation of the joint and hyperplasia of the synovium: The lining of the joint becomes inflamed and thickened.
- Destruction of articular structures: Cartilage and bone are damaged.
- Synovial infiltration: Lymphocytes, plasma cells, and macrophages infiltrate the synovium.
- Fibrin exudation: Fibrin, a clotting protein, deposits in the synovial fluid.
- Rice bodies: Small soft bodies formed from fibrin exudate in the joint fluid.
- Neutrophil polymorphs: White blood cells found within the joint.
RA: Pathology: Reversible and Irreversible Changes
- Reversible changes: All the aforementioned pathological changes are reversible in the early stages of RA.
- Irreversible changes: When granulation tissue (scar tissue) grows over the surface of the articular cartilage, a process called pannus formation occurs. This pannus interferes with cartilage nutrition, ultimately leading to permanent joint damage.
- Histopathological features:
- Rice bodies: Small soft bodies, often seen in the synovial fluid.
- Hyperplastic synovium: Thickened inflamed synovium.
- Pannus: Granulation tissue that grows over the articular cartilage.
- Allison-Ghormley bodies: Loose bodies within the joint cavity.
- Rheumatoid nodules: Lumps that are characteristic of RA.
Extra-Articular RA:
- Rheumatoid nodules: Subcutaneous nodules commonly found near elbows, fingers, and tendons.
- Vasculitis: Inflammation of blood vessels.
- Cardiac disease: Pericarditis (inflammation of the sac surrounding the heart) and valvular complications.
- Pulmonary disease: Pleuritis (inflammation of the lining of the lungs) and interstitial lung disease.
- Serosal inflammation: Inflammation of the membranes lining body cavities.
- Amyloidosis: Deposition of amyloid protein, potentially affecting organs.
- Anemia: Anemia due to chronic inflammation.
- Eye involvement: Sjogren's syndrome, which can cause dry eyes and dry mouth.
Morphology of RA:
- Proliferative synovitis with lymphocytes (CD4), plasma cells, and macrophages: The joint lining is inflamed with a cellular infiltrate.
- Pannus formation: The granulation tissue that grows over the cartilage.
- Organizing fibrin (rice bodies): Small soft bodies within the synovial fluid.
- Neutrophils on the joint surface and fluid: White blood cells contributing to inflammation.
- Juxta-articular erosions, cysts, and osteoporosis: Bone erosion, cysts, and bone thinning.
- Fibrous ankylosis: Joints may become fused by fibrous tissue.
- Skin: Rheumatoid nodules.
- Vasculitis: Inflammation of blood vessels, commonly affecting digital arteries.
Early Destruction in RA:
- Swan neck deformity: A characteristic deformity of the fingers in RA.
RA - Clinical Features:
- Morning stiffness: Stiffness that improves throughout the day, especially upon movement.
- Arthritis in three or more joint areas: Joint inflammation in multiple joints.
- Arthritis of small hand joints: Affects the joints of the hands, particularly the metacarpophalangeal (MCP) and proximal interphalangeal (PIP) joints.
- Symmetric arthritis: Joint inflammation is symmetrical, affecting the same joints on both sides of the body.
- Rheumatoid nodules: Subcutaneous lumps that are characteristic of RA.
- Serum rheumatoid factor: An antibody that is often present in patients with RA, but not specific for the disease.
- Typical radiographic changes:
- Erosion of the joint surface: Typically seen in the hands and feet.
- Narrowed joint spaces: Due to loss of cartilage.
- Bone remodeling and joint deformities.
- At least four features for diagnosis: The presence of at least four of these features is often used to diagnose RA.
Pannus in RA:
- Hyperplastic inflamed synovium: The inflamed and thickened joint lining.
Extra-Articular Manifestations of RA:
- Rheumatoid nodules: Lumps that can affect the skin, tendons, and internal organs.
- Vasculitis: Blood vessel inflammation that may cause skin lesions, ulcers, or nerve damage.
- Pleuritis: Inflammation of the lining of the lungs.
- Pericarditis: Inflammation of the lining of the heart.
- Tendonitis: Inflammation of tendons.
Skin RA Nodule:
- Palisading macrophages: Macrophages (immune cells) arranged in a ring-like pattern.
- Central fibrinoid necrosis: A characteristic central area of dead tissue.
Joint Involvement in RA:
- Synovial inflammation: Inflammation of the joint lining.
- Cartilage destruction: Erosion of the protective cartilage.
- Bone erosion: Damage to the underlying bone.
- Joint deformities: Abnormal alignment of the joints.
Swan Neck Deformity in RA:
- A characteristic deformity of the fingers in RA, resulting from tendon and ligament inflammation.
Differentiating Features: Rheumatoid Arthritis vs. Osteoarthritis
- Rheumatoid Arthritis:
- Younger age of onset
- Affects primarily small joints: Hands, wrists, feet
- Autoimmune basis: Immune system attack on the joints
- Synovial inflammation: Inflammation of the joint lining
- Osteoarthritis:
- Older age of onset
- Affects primarily large joints: Hips, knees, shoulders
- Degenerative basis: Wear and tear of the cartilage
- Cartilage degeneration: Breakdown of the protective cartilage
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.