Podcast
Questions and Answers
Which characteristic distinguishes arteries from veins?
Which characteristic distinguishes arteries from veins?
- Arteries lack a tunica media, unlike veins.
- Arteries carry blood away from the heart, while veins carry blood toward it. (correct)
- Arteries carry blood toward the heart, while veins carry blood away.
- Arteries have thicker tunica externa compared to veins.
What structural feature of veins is MOST important in counteracting the effects of gravity in the lower limbs?
What structural feature of veins is MOST important in counteracting the effects of gravity in the lower limbs?
- The tunica media in veins is more muscular, aiding in upward blood flow.
- Veins have valves that prevent the backflow of blood. (correct)
- The thicker tunica externa in veins provides additional support.
- Veins have a larger diameter compared to arteries, reducing resistance.
Which type of blood vessel is BEST suited for exchange of substances between blood and surrounding tissues?
Which type of blood vessel is BEST suited for exchange of substances between blood and surrounding tissues?
- Venules
- Arterioles
- Capillaries (correct)
- Muscular arteries
Which layer of a blood vessel wall primarily controls vasoconstriction and vasodilation?
Which layer of a blood vessel wall primarily controls vasoconstriction and vasodilation?
What is a key characteristic feature of continuous capillaries?
What is a key characteristic feature of continuous capillaries?
In which of the following locations would you expect to find fenestrated capillaries?
In which of the following locations would you expect to find fenestrated capillaries?
What unique structural adaptation is present in sinusoidal capillaries compared to other capillary types?
What unique structural adaptation is present in sinusoidal capillaries compared to other capillary types?
If multiple arteries merge before supplying a capillary bed, what are these arteries called?
If multiple arteries merge before supplying a capillary bed, what are these arteries called?
Which characteristic is MOST representative of blood pressure in veins?
Which characteristic is MOST representative of blood pressure in veins?
What is the primary mechanism by which skeletal muscle contraction aids in venous return?
What is the primary mechanism by which skeletal muscle contraction aids in venous return?
Approximately what percentage of total blood volume is typically found in the systemic venous system, acting as a blood reservoir?
Approximately what percentage of total blood volume is typically found in the systemic venous system, acting as a blood reservoir?
What is the physiological effect of venoconstriction?
What is the physiological effect of venoconstriction?
Which of the following factors does NOT directly contribute to total peripheral resistance?
Which of the following factors does NOT directly contribute to total peripheral resistance?
Which adjustment will cause the GREATEST decrease in vascular resistance?
Which adjustment will cause the GREATEST decrease in vascular resistance?
How does vessel length affect vascular resistance?
How does vessel length affect vascular resistance?
What is the effect of increased blood viscosity on peripheral resistance, assuming other factors remain constant?
What is the effect of increased blood viscosity on peripheral resistance, assuming other factors remain constant?
Which condition is MOST likely to cause turbulence in blood flow?
Which condition is MOST likely to cause turbulence in blood flow?
Where is blood flow velocity the LOWEST, which is ideal for substance exchange?
Where is blood flow velocity the LOWEST, which is ideal for substance exchange?
What is the MOST accurate definition of pulse pressure?
What is the MOST accurate definition of pulse pressure?
What calculation determines the mean arterial pressure (MAP)?
What calculation determines the mean arterial pressure (MAP)?
Which of the following is a direct effect of capillary hydrostatic pressure (CHP)?
Which of the following is a direct effect of capillary hydrostatic pressure (CHP)?
What happens to net filtration pressure (NFP) as blood moves from the arterial end to the venous end of a capillary?
What happens to net filtration pressure (NFP) as blood moves from the arterial end to the venous end of a capillary?
What is generally true about the amounts of fluid that leaves the bloodstream compared to amount that is reabsorbed by capillaries?
What is generally true about the amounts of fluid that leaves the bloodstream compared to amount that is reabsorbed by capillaries?
If the blood colloid osmotic pressure (BCOP) increases above normal, what effect will this have on capillary exchange?
If the blood colloid osmotic pressure (BCOP) increases above normal, what effect will this have on capillary exchange?
What is the term for the accumulation of excess fluid in peripheral tissues due to the CHP rising or the BCOP decreasing?
What is the term for the accumulation of excess fluid in peripheral tissues due to the CHP rising or the BCOP decreasing?
Autoregulation fails to maintain local blood flow; which regulatory pathway is then activated?
Autoregulation fails to maintain local blood flow; which regulatory pathway is then activated?
How does a local increase in vasodilators influence blood flow in capillary beds?
How does a local increase in vasodilators influence blood flow in capillary beds?
Which of the following is a SHORT-TERM effect of the sympathetic nervous system activation in response to decreased blood pressure?
Which of the following is a SHORT-TERM effect of the sympathetic nervous system activation in response to decreased blood pressure?
Which action is a long-term hormonal response to counteract decreased blood pressure and volume?
Which action is a long-term hormonal response to counteract decreased blood pressure and volume?
How do natriuretic peptides (ANP and BNP) help to reduce high blood volume?
How do natriuretic peptides (ANP and BNP) help to reduce high blood volume?
Which of the following conditions is Monitored by chemoreceptors?
Which of the following conditions is Monitored by chemoreceptors?
Where are chemoreceptors located that monitor blood and CSF composition?
Where are chemoreceptors located that monitor blood and CSF composition?
During light exercise, what adaptation DIRECTLY facilitates increased venous return?
During light exercise, what adaptation DIRECTLY facilitates increased venous return?
During heavy exercise, which systemic adaptations are MOST important for increasing blood flow to skeletal muscles?
During heavy exercise, which systemic adaptations are MOST important for increasing blood flow to skeletal muscles?
How does cardiovascular performance typically differ between trained athletes and non-athletes?
How does cardiovascular performance typically differ between trained athletes and non-athletes?
What percentage of total blood volume can typically be lost before compensation mechanisms become insufficient, leading to shock?
What percentage of total blood volume can typically be lost before compensation mechanisms become insufficient, leading to shock?
During initial response to blood loss, what short-term effect helps to maintain cardiac output?
During initial response to blood loss, what short-term effect helps to maintain cardiac output?
What is the long-term compensation mechanisms after blood loss?
What is the long-term compensation mechanisms after blood loss?
Which condition defines circulatory shock?
Which condition defines circulatory shock?
In progressive shock, what process damages the myocardium, ultimately leading to a further reduction in cardiac output?
In progressive shock, what process damages the myocardium, ultimately leading to a further reduction in cardiac output?
What condition marks the point of circulatory collapse and imminent death in irreversible shock?
What condition marks the point of circulatory collapse and imminent death in irreversible shock?
Flashcards
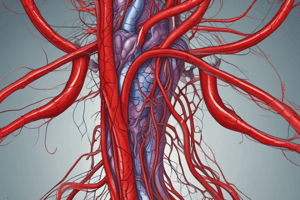
Blood vessels
Blood vessels
Conduct blood between the heart and peripheral tissues.
Arteries
Arteries
Carry blood away from the heart; also called efferent vessels.
Veins
Veins
Carry blood to the heart; also called afferent vessels.
Capillaries
Capillaries
Signup and view all the flashcards
Pulmonary circuit
Pulmonary circuit
Signup and view all the flashcards
Systemic circuit
Systemic circuit
Signup and view all the flashcards
Tunica intima
Tunica intima
Signup and view all the flashcards
Tunica media
Tunica media
Signup and view all the flashcards
Tunica externa
Tunica externa
Signup and view all the flashcards
Vasoconstriction
Vasoconstriction
Signup and view all the flashcards
Vasodilation
Vasodilation
Signup and view all the flashcards
Typical capillary
Typical capillary
Signup and view all the flashcards
Continuous capillary
Continuous capillary
Signup and view all the flashcards
Fenestrated capillary
Fenestrated capillary
Signup and view all the flashcards
Sinusoids
Sinusoids
Signup and view all the flashcards
Capillary bed
Capillary bed
Signup and view all the flashcards
Collaterals
Collaterals
Signup and view all the flashcards
Valves (veins)
Valves (veins)
Signup and view all the flashcards
Blood reservoirs
Blood reservoirs
Signup and view all the flashcards
Venoconstriction
Venoconstriction
Signup and view all the flashcards
Venous return
Venous return
Signup and view all the flashcards
Total peripheral resistance
Total peripheral resistance
Signup and view all the flashcards
Vascular resistance
Vascular resistance
Signup and view all the flashcards
Viscosity
Viscosity
Signup and view all the flashcards
Turbulence
Turbulence
Signup and view all the flashcards
Systolic pressure
Systolic pressure
Signup and view all the flashcards
Diastolic pressure
Diastolic pressure
Signup and view all the flashcards
Pulse pressure
Pulse pressure
Signup and view all the flashcards
Mean arterial pressure (MAP)
Mean arterial pressure (MAP)
Signup and view all the flashcards
Capillary exchange
Capillary exchange
Signup and view all the flashcards
Capillary hydrostatic pressure (CHP)
Capillary hydrostatic pressure (CHP)
Signup and view all the flashcards
Blood colloid osmotic pressure (BCOP)
Blood colloid osmotic pressure (BCOP)
Signup and view all the flashcards
Net filtration pressure (NFP)
Net filtration pressure (NFP)
Signup and view all the flashcards
Capillary exchange variation
Capillary exchange variation
Signup and view all the flashcards
Autoregulation
Autoregulation
Signup and view all the flashcards
Vasodilators
Vasodilators
Signup and view all the flashcards
Central regulation
Central regulation
Signup and view all the flashcards
Baroreceptor reflexes
Baroreceptor reflexes
Signup and view all the flashcards
Chemoreceptor reflexes
Chemoreceptor reflexes
Signup and view all the flashcards
Endocrine responses
Endocrine responses
Signup and view all the flashcards
Tissue perfusion
Tissue perfusion
Signup and view all the flashcards
Study Notes
Chapter 19: Blood Vessels and Circulation
- Blood vessels and circulation are essential for transporting blood throughout the body.
- This chapter covers the different types of blood vessels, the structure of arteries and veins, capillary structure, venous system characteristics, cardiovascular regulation and adjustments during exercise, responses to blood loss, and blood supply to systemic circuits and limbs.
Module 19.1: Blood Vessel Overview and Circuits
- Blood vessels transport blood between the heart and peripheral tissues.
- Arteries, also called efferent vessels, carry blood away from the heart.
- Veins, also known as afferent vessels, carry blood to the heart.
- Capillaries facilitate the exchange of substances between blood and tissues.
- Capillaries interconnect the smallest arteries and veins.
- There are two main circulatory circuits: pulmonary and systemic.
- The pulmonary circuit carries blood to and from gas exchange surfaces in the lungs.
- The systemic circuit transports blood to and from the rest of the body.
Module 19.2: Structure of Arteries and Veins
- Arteries and veins have three layers.
- The tunica intima is the innermost layer, comprising endothelial cells with connective tissue and elastic fibers.
- The tunica media is the middle layer of arteries and veins, which contains concentric sheets of smooth muscle.
- Contraction of the tunica media results in vasoconstriction, decreasing vessel diameter.
- Relaxation of the tunica media results in vasodilation, increasing vessel diameter.
- The tunica externa, or tunica adventitia, is the outermost layer.
- In arteries, the tunica externa contains collagen and scattered elastic fibers.
- In veins, the tunica externa is generally thicker than the tunica media.
- The tunica externa contains networks of elastic fibers and bundles of smooth muscle cells.
- The tunica externa anchors the vessel to surrounding tissues.
Module 19.3: Capillary Structure and Function
- Capillaries consist of a tube of endothelial cells with a delicate basement membrane.
- Capillaries lack both tunica media and tunica externa.
- Continuous capillaries have a complete endothelial lining.
- Continuous capillaries are located throughout the body in all tissues except epithelia and cartilage.
- They permit diffusion of water, small solutes, and lipid-soluble materials.
- Continuous capillaries prevent the loss of blood cells and plasma proteins.
- They have some selective vesicular transport.
- Specialized continuous capillaries in the CNS and thymus have endothelial tight junctions.
- These specialized capillaries enable restricted and regulated permeability.
- Fenestrated capillaries contain "windows," or pores, penetrating the endothelial lining.
- Fenestrated capillaries permit rapid exchange of water and larger solutes.
- Examples of fenestrated capillaries include those found in the choroid plexus of the brain, capillaries of the hypothalamus, pituitary, pineal, thyroid glands, absorptive areas of the intestinal tract, and kidney filtration sites.
- Sinusoids resemble fenestrated capillaries but are flattened and irregularly shaped.
- Sinusoids commonly have gaps between endothelial cells and a thin or absent basement membrane.
- Sinusoids permit more water and solute, including plasma proteins, exchange.
- Sinusoids can be found in the liver, bone marrow, spleen, and many endocrine organs.
- A capillary bed refers to an interconnected network of capillaries, which may be supplied by more than one artery.
- Collaterals, or multiple arteries, fuse before giving rise to arterioles.
Module 19.4: Venous System
- Blood pressure in the peripheral venules is less than 10 percent of that in ascending aorta.
- Gravity is a force that blood flow needs to be maintained against in the veins
- Veins need mechanisms to maintain blood flow against the force of gravity.
- Valves are folds of the tunica intima projecting from the vessel wall pointing in the direction of blood flow.
- Valves ensure one-way flow of blood toward the heart, aided by the contraction of skeletal muscles.
- Skeletal muscle contraction squeezes veins to permit blood flow toward capillaries.
- Valves prevent backflow of blood toward the capillaries.
- Valves that malfunction can cause blood to pool in veins leading to distension.
- The systemic venous system contains 64% of total blood volume, roughly 3.5 L.
- Blood reservoirs, consisting of 1 L, carrying blood from digestive organs to the liver.
- Systemic arteries contain 13 percent total blood volume.
- The remaining blood is in the systemic capillaries, heart, and pulmonary circuit.
- Venoconstriction is the contraction of smooth muscle fibers in veins, which reduces vessel diameter.
- Venous system can maintain blood volume with blood loss through venoconstriction.
Module 19.5: Cardiovascular Regulation and Venous Return
- Blood pressure in the veins is maintained by valves and muscular compression of peripheral veins.
- As blood moves toward the heart, vessels get larger and resistance decreases.
- Venous return is the amount of blood arriving at the right atrium each minute.
- On average, venous return is equal to the cardiac output.
Module 19.6: Factors Affecting Peripheral Resistance
- Total peripheral resistance comes from the degree of resistance of the the cardiovascular system
- Sufficient pressure from the heart is necessary to overcome circulation to occur
- It then depends on three factors which are vascular resistance, viscosity and turbulence
- Vascular resistance is the opposition to blood flow in vessels and the largest component of the total peripheral resistance, which results from friction between blood and the vessel walls.
- Friction depends on vessel Length and diameter
- Friction between vessel walls and moving blood occurs in vessel length
- Increase in vessel length = increased surface area = increased friction or resistance.
- Vessel diameter has a much larger effect on resistance compared to vessel length
- 𝑅 = 1/𝑟^4 , change in radius (r) affects resistance (R) to the 4th power
- Blood viscosity is about five times that of water
- Viscosity depends on cells and plasma proteins but normally these are stable
- Fluid flow experiences eddies and swirls, a phenomenon refered to as Turbulence.
- Turbulence is caused by high flow rates, irregular surfaces, and sudden changes in vessel diameter.
- Turbulence normally occurs in the heart
Module 19.7: Factors Affecting Blood Flow
- Changes in blood pressure impact blood flow
- Highest flow is inthe aorta
- There is also the highest blood pressure, largest diameter.
- Flow is slowest in the capillaries because of the smallest diameter
- This allows exchange between blood and interstitial fluid
- Flow accelerates in venous system due to larger diameter vessels and lower resistance
- Systolic pressure is the peak pressure measured during systole.
- Diastolic pressure is the minimum pressuring measured during diastole.
- These values are separated by "/" between pressures with an example being 120/80
- Pulse pressure refers to the difference between systolic and diastolic pressure, shown by the example: 120-90 = 30 mm Hg
- Mean arterial pressure is abbreviated to MAP. Adding one-third of pulse pressure to diastolic pressure Example: 90+ (120-90) / 3 = 100 mm Hg
- MAP is important because is accounts for flow, resistance, and pressure within in the arteries, it also allows you to see how well blood is flowing through your body
- Best MAP range is between 70 and 110 mm Hg.
- Capillary exchange is influenced by the combination of diffusion, osmosis, and filtration.
- Capillary hydrostatic pressure is the blood pressure within capillary beds.
- It is a driving force for pushing water and small molecules out of the bloodstream into interstitial fluid, while leaving larger molecules behind.
Module 19.8: Capillary Exchange Dynamics
- Capillary exchange involves diffusion, filtration, and reabsorption.
- Diffusion happens from an area of higher concentration to lower concentration occurs most rapidly when distances are short, when the concentration gradient is large, and when ions or molecules involved are small.
- Diffusion continuously occurs across capillary walls, but the transport mechanism varies.
- Filtration is where capillary hydrostatic pressure is at its highest and small solutes enter interstitial fluid.
- As filtration occurs, pressure increases. Water leaves capillary, and plasma proteins remain
- Net filration pressures can be explained through a few formulas, including; NFP = CHP – BCOP.
- The results are positive at the beginning of capillary leading to filtration and negative by end reabsorption
- Capillary hydrostatic pressure, blood colloid osmotic pressure euals zero for movement of the capillaries.
- Reabsorption predominates in which: Capillary hydrostatic pressure falls below blood colloid osmotic pressure.CHP < BCOP. Difference (about 3.6 L/day) enters the lymphatic vessels and is eventually returned to the venous system due to a water move into the capillary.
- Conditions that affects the pressure of blood or interstital fluid of hydrostatic and osmotic forces.
- If hemorrhaging occurs, both blood volume and blood pressure decline
- This can cause the NFP to lower and increases the amount of capillary reabsorption.
- If dehydration occurs, the plasma water volume will decrease and then the concentration of plasma proteins increase
- If the CHP rises or the BCOP decreases, fluid moves out of the blood in capillaries and builds up in peripheral tissues, calling this edema.
Module 19.9: Cardiovascular Regulatory Mechanisms
- Homeostatic mechanisms aim to ensure adequate tissue perfusion (blood flow through tissues) with two regulatory pathways which are Autoregulation and Central regulation.
- Autoregulation occurs at local level and Involves local changes in blood flow within capillary beds, regulated by precapillary sphincters in reaction to chemical changes in interstitial fluid with Vasodilators.
- Central regulation can have either Neural and endocrine control which is only activated if autoregulation is ineffective, Activation of cardioacceleratory center with Release of primarily NE,producing long-term increases in blood pressure.
- In baroreceptor reflexes cardiac centers decrease or increase cardiac output through sympathetic innervation to the heart.
- There can also be Widespread peripheral vasodilation due to the inhibition of the vasomotor center of the medulla oblongata.
Module 19.10: Hormonal Responses
- Endocrine responses provide short-term and long-term regulation ▪ The heart,The kidneys are endocrine functions, including anti-diuretic hormone or (ADH).
- If there is low blood pressure/volume there is typically a Immediate:E and NE adrenal medullae And Long-term response:Antidiuretic hormone (ADH), Angiotensin II, Erythropoietin (EPO), Aldosterone. With a high blood pressure/volume causes volume stretches the heart wall to: trigger atrial natriuretic peptide or brain natriuretic peptide.
Module 19.11: Chemoreceptors and Chemical Composition
- Responds to blood and of the Cerebral Spinal Fluid in carbon dioxide, oxygen, etc.
- Carotid and arotic bodies
- Venrolateral stimulation triggers adjustmen to cardiovascular function and respiratory functions
Module 19.12: Cardiovascular Adjustments During Exercise
- Cardiac output = 5800 mL/min at rest.
- Three changes takes place during light exercise
- Vasodilation occurs and capillary blood flow increases
- Venus return is high
- output increased and is mainly caused by venuous return
- During heavy exercise
- high cardiac outputs and major changes to the blood distribution allow high flow to skeletal muscles, and decreased visera but unchanged to the brain
- Cardiac output in athlete can be fifty percent higher
Module 19.13: Responses to Blood Loss and Module
- Immediate maintence of the blood pressure in the peripeheral blood flow
- Long term problem is restorign blood volume
- Homeastasis that is between and thirty percent volume can be coped with
- Blood Loss: Typically caused by Carotid and aortic reflexes increase cardiac output and stress
- In which there is pain so increase in sympatic system to get more volume and shift to aterial system
- Decreased blood pressure by 35% causes:Blood pressure remains low and venous return reduced and cardiac output inadequate.
- Damag to the muocardum or decrease in peripherial blood can causes schock and damage
- Low pH can casue permiability and will shut down if severe.
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.