Podcast
Questions and Answers
What primary role does the diaphragm play during inspiration?
What primary role does the diaphragm play during inspiration?
- Lowers the height of the thoracic cavity
- Increases the height of the thoracic cavity (correct)
- Increases the overall lung pressure
- Decreases the thoracic cavity volume
Which muscles are involved in the active process of inspiration?
Which muscles are involved in the active process of inspiration?
- Rectus abdominis and external obliques
- Sternocleidomastoid and pectoralis major
- Internal intercostals and scalenes
- Diaphragm and external intercostals (correct)
What is the effect of the intercostal muscles during inhalation?
What is the effect of the intercostal muscles during inhalation?
- They compress the thoracic cavity
- They relax, decreasing the thoracic cavity volume
- They inhibit diaphragm function
- They contract, pulling ribs up and out (correct)
How do intrapulmonary and intrapleural pressures change during expiration?
How do intrapulmonary and intrapleural pressures change during expiration?
Which statement accurately describes the mechanics of breathing at rest?
Which statement accurately describes the mechanics of breathing at rest?
What is the primary function of bronchial arteries in the lungs?
What is the primary function of bronchial arteries in the lungs?
Which layer of the pleurae directly lines the lungs and dips into the fissures?
Which layer of the pleurae directly lines the lungs and dips into the fissures?
What occurs during pleurisy?
What occurs during pleurisy?
What is the impact of sympathetic fibers on bronchial passages?
What is the impact of sympathetic fibers on bronchial passages?
What is the role of pleural fluid in the thoracic cavity?
What is the role of pleural fluid in the thoracic cavity?
What is pleural effusion?
What is pleural effusion?
What commonly leads to the accumulation of fluid in the pleural cavity?
What commonly leads to the accumulation of fluid in the pleural cavity?
What is the main source of oxygenated blood for lung tissue?
What is the main source of oxygenated blood for lung tissue?
What is transpulmonary pressure?
What is transpulmonary pressure?
What can lead to lung collapse in terms of pressure equalization?
What can lead to lung collapse in terms of pressure equalization?
Which condition is a possible cause of atelectasis?
Which condition is a possible cause of atelectasis?
How does Boyle's law relate to pulmonary ventilation?
How does Boyle's law relate to pulmonary ventilation?
What happens during a pneumothorax?
What happens during a pneumothorax?
What is the mechanism by which volume changes lead to gas flow during respiration?
What is the mechanism by which volume changes lead to gas flow during respiration?
What is a necessary condition to maintain lung inflation?
What is a necessary condition to maintain lung inflation?
What occurs if the intrapleural pressure becomes equal to atmospheric pressure?
What occurs if the intrapleural pressure becomes equal to atmospheric pressure?
What effect does surface tension have on alveoli?
What effect does surface tension have on alveoli?
Which cells are responsible for secreting surfactant in the alveoli?
Which cells are responsible for secreting surfactant in the alveoli?
What is the main consequence of a lack of surfactant in infants?
What is the main consequence of a lack of surfactant in infants?
What is the average tidal volume at rest?
What is the average tidal volume at rest?
Which pulmonary volume is defined as the air that remains in the lungs to prevent collapse?
Which pulmonary volume is defined as the air that remains in the lungs to prevent collapse?
How much air can typically be forcibly inspired beyond a tidal volume inspiration?
How much air can typically be forcibly inspired beyond a tidal volume inspiration?
What is a potential treatment for infants suffering from respiratory distress syndrome due to lack of surfactant?
What is a potential treatment for infants suffering from respiratory distress syndrome due to lack of surfactant?
What is a possible complication from mechanical ventilation in severe cases of infant respiratory distress syndrome?
What is a possible complication from mechanical ventilation in severe cases of infant respiratory distress syndrome?
What is the primary function of the dorsal respiratory group (DRG)?
What is the primary function of the dorsal respiratory group (DRG)?
What effect does damage to the pontine respiratory centers have on breathing?
What effect does damage to the pontine respiratory centers have on breathing?
Which factor directly influences the rate of breathing?
Which factor directly influences the rate of breathing?
What is suggested about the origin of the breathing rhythm?
What is suggested about the origin of the breathing rhythm?
What determines the depth of breathing during inspiration?
What determines the depth of breathing during inspiration?
Which of the following best describes how the pontine respiratory centers function?
Which of the following best describes how the pontine respiratory centers function?
Which mechanisms can directly alter the respiratory centers' activity?
Which mechanisms can directly alter the respiratory centers' activity?
What is the role of peripheral stretch and chemoreceptors in respiratory control?
What is the role of peripheral stretch and chemoreceptors in respiratory control?
Flashcards are hidden until you start studying
Study Notes
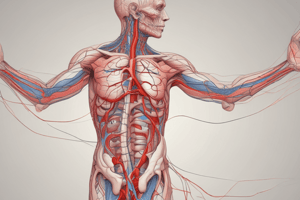
Blood Supply of the Lungs
- Bronchial arteries supply oxygenated blood to lung tissue
- They arise from the aorta and enter the lungs at the hilum.
- They are part of the systemic circulation, unlike the pulmonary arteries that carry deoxygenated blood from the heart to the lungs
- Bronchial arteries supply all lung tissue except the alveoli.
- Bronchial veins anastomose with pulmonary veins
- Pulmonary veins carry most venous blood back to the heart.
Innervation of the Lungs
- Lungs are innervated by parasympathetic and sympathetic fibers, as well as visceral sensory fibers.
- Parasympathetic fibers cause bronchoconstriction, narrowing the airways.
- Sympathetic fibers cause bronchodilation, widening the airways.
The Pleurae
- The pleurae are thin, double-layered membranes that divide the thoracic cavity into two pleural compartments and a central mediastinum.
- Parietal pleura lines the inner surface of the thoracic wall and the superior face of the diaphragm, continuing inward to form the lateral mediastinal walls
- Visceral pleura lines the external lung surface, dipping into fissures
- Pleural fluid fills the slitlike pleural cavity.
- Provides lubrication as visceral and parietal pleurae slide past each other.
- Provides surface tension that resists separation of the pleurae, helps to keep lungs connected to the thoracic wall and diaphragm.
Pleurisy
- Inflammation of the pleurae, often a result of pneumonia.
- This can lead to roughened inflamed pleurae, causing friction and stabbing pain with each breath.
- Inflamed pleurae may produce excessive protective fluid, which can exert pressure on the lungs, hindering breathing.
- Pleurisy can lead to pleural effusion, where fluid accumulates in the pleural cavity.
Pressure Relationships in the Thoracic Cavity
- Transpulmonary pressure: the difference between the intrapulmonary and intrapleural pressures (Ppul - Pip).
- This pressure keeps lung spaces open and prevents them from collapsing.
- The size of the transpulmonary pressure determines the size of the lungs, with more pressure causing greater lung expansion.
- Any condition that allows the intrapleural pressure (Pip) to equalize with the intrapulmonary pressure (Ppul) or atmospheric pressure (Patm) will cause lung collapse
- A negative Pip must be maintained to keep lungs inflated.
- This pressure keeps lung spaces open and prevents them from collapsing.
Pneumothorax
- Air in the pleural cavity, can occur from either a wound in the parietal pleura or a rupture of the visceral pleura.
- This causes lung collapse as the Pip equalizes with the Patm.
- Can be treated by removing air with chest tubes, allowing pleurae to heal and regain normal function.
Atelectasis (Lung Collapse)
- Can occur from plugged bronchioles, which causes collapse of alveoli as trapped air is absorbed.
- This can also result from pneumothorax
- Treated by removing air with chest tubes allowing pleurae to heal and regain normal function (keeping lungs inflated).
Pulmonary Ventilation
- Consists of inspiration and expiration; mechanical process that requires volume changes.
- Volume changes lead to pressure changes, and pressure changes lead to the flow of gases to equalize the pressure
- Boyle's Law explains this relationship: pressure (P) varies inversely with volume (V).
- Volume changes lead to pressure changes, and pressure changes lead to the flow of gases to equalize the pressure
Inspiration
- An active process involving inspiratory muscles, the diaphragm, and external intercostals.
- The diaphragm increases the height of the thoracic cavity (thus volume) by flattening out as it contracts.
- Intercostal muscles increase the diameter of the thorax (thus volume) by pulling ribs up and out.
Expiration
- Usually a passive process, relies on the elastic recoil of lung tissue.
- As inspiratory muscles relax, the chest wall recoils inward.
- Increased intrapulmonary pressure forces air out of the lungs.
- Can be active during forceful expiration, involving internal intercostals and abdominal muscles.
- These muscles increase intrapulmonary pressure, rapidly expelling air from the lungs .
Factors Influencing Pulmonary Ventilation
- Alveolar surface tension
- At a gas-liquid interface, liquid molecules are more strongly attracted to each other than to gas molecules, producing surface tension which tends to draw liquid molecules closer together and resists any force that tends to increase the surface area of the liquid.
- Water, which has very high surface tension, lines alveolar walls in a thin film, tending to shrink (collapse) alveoli to the smallest size.
- Type II alveolar cells secrete surfactant, a detergent-like complex of lipids and proteins.
- This lessens surface tension of alveolar fluid, prevents alveolar collapse and reduces the work of lung inflation.
Infant Respiratory Distress Syndrome (IRDS)
- Caused by a lack of surfactant, resulting in alveoli collapsing after each breath due to excessive surface tension.
- This requires lots of energy to reinflate lungs with each inspiration.
- It is common in premature babies as fetal lungs don’t produce enough surfactant until the last two months of development.
- Treated with a spray of natural or synthetic surfactant into a newborn’s airways.
- Positive pressure devices can also help to keep alveoli open between breaths.
- Severe cases may require mechanical ventilation which can lead to bronchopulmonary dysplasia (a chronic lung disease that begins in childhood).
Pulmonary Volumes
- There are four pulmonary (lung) volumes:
- Tidal volume (TV): amount of air moved into and out of lung with each breath (average ~500ml at rest).
- Inspiratory reserve volume (IRV): amount of air that can be forcibly inspired beyond a tidal volume inspiration (2100–3200 ml).
- Expiratory reserve volume (ERV): amount of air that can be forcibly expired beyond a tidal volume expiration (1000–1200 ml).
- Residual volume (RV): amount of air that always remains in the lungs, keeps alveoli open (prevents collapse); ~1200 ml.
Pulmonary Capacities
- These are combinations of pulmonary volumes:
- Inspiratory capacity (IC): TV + IRV, total amount of air that can be inspired after a normal expiration (~3600 ml).
- Functional residual capacity (FRC): ERV + RV, amount of air remaining in the lungs after a normal expiration (~2400 ml).
- Vital capacity (VC): TV + IRV + ERV, amount of air that can be forcibly exhaled after a maximal inspiration (~4800 ml).
- Total lung capacity (TLC): TV + IRV + ERV + RV, total amount of air the lungs can hold (~6000 ml).
Neural Mechanisms of Breathing
- Neural control of breathing involves several areas in the brainstem, particularly in the medulla oblongata:
- Dorsal respiratory group (DRG)
- Integrates input from peripheral stretch and chemoreceptors, then modifies information to VRG neurons.
- Responsible for inspiration.
- Ventral respiratory group (VRG)
- Contains neurons that fire rhythmically, creating the basic breathing pattern.
- Can generate inspiratory and expiratory signals, also involved in forceful exhalation.
- Pontine respiratory centers
- Influence and modify activity of the VRG, smoothing transitions between inspiration and expiration.
- Communicate with the VRG during vocalization, sleep, and exercise to fine-tune breathing rhythms.
- Also receive inputs from higher brain centers and peripheral receptors.
- Dorsal respiratory group (DRG)
Factors Influencing Breathing Rate and Depth
- Depth of breathing
- Determined by how actively the VRG stimulates respiratory muscles.
- Greater stimulation activates more motor units, increasing the depth (tidal volume) of inspiration.
- Rate of breathing
- Determined by how long inspiratory neurons are active (or how quickly they are switched off).
- Both depth and rate are determined by the changing demands of the body, with respiratory centers being affected by chemical factors, influence of higher brain centers, pulmonary irritant reflexes, the inflation reflex.
- Determined by how actively the VRG stimulates respiratory muscles.
Chemical Factors
- Carbon dioxide (CO2)
- Increased CO2 levels in the blood cause an increase in breathing rate and depth (hyperventilation) to eliminate excess CO2.
- Oxygen (O2)
- Decreased O2 levels in the blood cause an increase in breathing rate and depth (hyperventilation) to increase oxygen uptake., however, a decrease in Oxygen normally has a lesser effect on respiration than an increase in CO2.
- Hydrogen ions (H+)
- Increased H+ levels (acidity) in the blood stimulate the chemoreceptors to increase breathing rate and depth, but it is mainly the increase in CO2 which triggers H+ production and therefore increases breathing.
Influence of Higher Brain Centers
- The cerebral cortex can influence breathing rate and depth:
- Allows for voluntary control of breathing.
- Can override the automatic control of the respiratory center and send signals to the VRG.
- The hypothalamus influences breathing rate and depth:
- Responds to emotional states, stress, and pain.
Pulmonary Irritant Reflexes
- Stimulation of receptors in the airways by irritants (dust, smoke, noxious gases) triggers the cough or sneeze reflex:
- Helps to clear irritants from the airways and the lungs.
The Inflation Reflex (Hering-Breuer Reflex)
- Stretch receptors in the lungs detect excessive lung inflation, which triggers inhibition of inspiratory neurons.
- This helps to prevent over-inflation of the lungs, allowing for more even gas exchange and preventing damage to the lungs.
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.