Podcast
Questions and Answers
Which of the following accurately describes the function of baroreceptors in blood pressure regulation?
Which of the following accurately describes the function of baroreceptors in blood pressure regulation?
- They primarily function to decrease heart rate and cause vasodilation via the sympathetic nervous system.
- They detect changes in blood pressure through stretch in arterial walls and trigger autonomic responses. (correct)
- They primarily regulate long-term blood volume by controlling water reabsorption in the kidneys.
- They directly stimulate the release of renin from the kidneys in response to high blood pressure.
What is the primary effect of Angiotensin II on blood pressure regulation?
What is the primary effect of Angiotensin II on blood pressure regulation?
- Increased sodium excretion and decreased ADH release, lowering blood pressure.
- Decreased heart rate and increased renal perfusion, stabilizing blood pressure.
- Vasodilation and decreased aldosterone release, leading to reduced blood volume.
- Vasoconstriction and increased aldosterone release, leading to increased blood volume. (correct)
How does the posterior pituitary gland respond to poor perfusion, and what is the overall effect of this response?
How does the posterior pituitary gland respond to poor perfusion, and what is the overall effect of this response?
- It releases ADH, promoting water reabsorption in the kidneys and increasing blood volume and pressure. (correct)
- It releases ANP, promoting water loss and decreasing blood pressure.
- It stimulates renin release, ultimately decreasing blood volume through naturesis.
- It inhibits ADH release, leading to increased urine output and decreased blood pressure.
How do ANP and BNP contribute to blood pressure regulation?
How do ANP and BNP contribute to blood pressure regulation?
What is the role of LDL cholesterol in the development of atherosclerosis?
What is the role of LDL cholesterol in the development of atherosclerosis?
How does elevated blood glucose contribute to cardiovascular disease?
How does elevated blood glucose contribute to cardiovascular disease?
How do free radicals contribute to the development of atherosclerosis?
How do free radicals contribute to the development of atherosclerosis?
What is the primary mechanism by which nicotine increases the risk of heart disease?
What is the primary mechanism by which nicotine increases the risk of heart disease?
How might a vitamin B deficiency contribute to an increased risk of heart disease?
How might a vitamin B deficiency contribute to an increased risk of heart disease?
In the context of blood pressure regulation, what is the immediate response triggered by the sympathetic nervous system (SNS) when baroreceptors detect a drop in blood pressure?
In the context of blood pressure regulation, what is the immediate response triggered by the sympathetic nervous system (SNS) when baroreceptors detect a drop in blood pressure?
Flashcards
Baroreceptors
Baroreceptors
Sense drops in blood pressure via stretch in arterial walls, signaling the brain.
Sympathetic Nervous System (SNS)
Sympathetic Nervous System (SNS)
Responds to baroreceptor signals by increasing heart rate and vasoconstriction.
Decreased Renal Perfusion
Decreased Renal Perfusion
Triggers renin secretion when reduced, activating the RAAS system.
Angiotensin II
Angiotensin II
Signup and view all the flashcards
Antidiuretic Hormone (ADH)
Antidiuretic Hormone (ADH)
Signup and view all the flashcards
Baroreceptor Function
Baroreceptor Function
Signup and view all the flashcards
Natriuresis
Natriuresis
Signup and view all the flashcards
Cholesterol
Cholesterol
Signup and view all the flashcards
High-Density Lipoprotein (HDL)
High-Density Lipoprotein (HDL)
Signup and view all the flashcards
Low-Density Lipoprotein (LDL)
Low-Density Lipoprotein (LDL)
Signup and view all the flashcards
Study Notes
- Baroreceptors sense a drop in blood pressure due to stretch in the arterial walls, which sends signals to the brain
- Baroreceptors notify the Sympathetic Nervous System (SNS) to respond
- The sympathetic nervous system responds by increasing heart rate and causing vasoconstriction to increase blood pressure
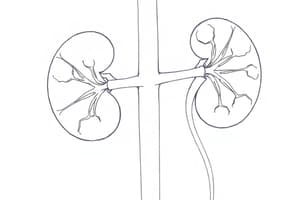
- Decreased renal perfusion (blood flow) can cause damage and dysfunction
- The kidney secretes renin, which turns angiotensinogen (from the liver) into angiotensin I
- Angiotensin I gets converted to angiotensin II by ACE (in the lungs)
- Angiotensin II causes vasoconstriction to increase blood pressure
- Angiotensin II causes the release of aldosterone to retain sodium and water, and the release of antidiuretic hormone to retain water
- Overall, angiotensin II leads to increased blood volume and vasoconstriction
- Poor perfusion sensed by the posterior pituitary gland leads to increased blood pressure and an increased concentration of sodium
- Release of ADH (vasopressin) leads to retention of water
- Nephrons filter blood, remove waste, and regulate blood pressure, therefore increased water reabsorption at the collecting duct
- Overall, this leads to increased blood volume and pressure
Baroreceptors
- Baroreceptors function in short-term regulation, adjust with standing or exercising and detect drops in blood pressure
- Regulation: Pons/medulla receives the signal and notifies the autonomic nervous system
- Parasympathetic (vagus nerve): decrease HR
- Sympathetic: increase HR, vasoconstriction, strengthen contractions (rapid increase)
- Location: Arterial walls (carotid/aortic arch)
- Age: decreased sensitivity
Naturesis
- Naturesis occurs when the heart gets rid of excess water in blood, when there is too much water, the ventricle stretches and therefore releases BNP/ANP
- BNP/ANP acts on kidneys to release extra water into the urine, along with sodium
- Overall, this decreases blood pressure and volume
Lipids
- Lipids are fats in the blood, which make up the cell membrane, and are composed of cholesterol (from food or the liver)
- Cholesterol is good for cell membranes, making bile acids/hormones/Vitamin D
- It comes from animal products (meat, milk), is insoluble in blood, so carried by lipoproteins
- HDL removes cholesterol from the body (good)
- LDL builds up on arterial walls, causing plaque formation (atherosclerosis)
Glucose
- Increased amounts of glucose lead to blood vessel harm/plaque build up
- Glucose narrows blood vessels, which increases the risk of heart attack/stroke
Free Radicals
- Free radicals damage blood vessel walls and inflammation can lead to plaque build up
Nicotine
- Nicotine tightens walls, especially around the heart
- Increased blood pressure/heart rate hours after nicotine ingestion increases the risk for heart disease
Homocysteine
- Homocysteine is an amino acid that damages vessel walls and decreases Vitamin B
- It is linked to blood clots and heart disease
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.