Podcast
Questions and Answers
What is the primary purpose of hemostasis?
What is the primary purpose of hemostasis?
- To activate platelets excessively
- To keep the blood fluid and clot-free in normal vessels
- To rapidly form a plug in injured vessels (correct)
- To induce blood clotting throughout the body
Which type of thrombosis is mainly managed by antiplatelet agents?
Which type of thrombosis is mainly managed by antiplatelet agents?
- Atrial fibrillation induced thrombosis
- Arterial thrombosis (correct)
- Venous thrombosis
- Thrombosis associated with artificial mechanical heart valves
Thrombin is an enzyme that converts soluble fibrinogen to an insoluble fibrin polymer during hemostasis.
Thrombin is an enzyme that converts soluble fibrinogen to an insoluble fibrin polymer during hemostasis.
True (A)
The primary anticoagulant that inactivates thrombin and other coagulation factors is ________.
The primary anticoagulant that inactivates thrombin and other coagulation factors is ________.
Match the anticoagulants with their types of interference:
Match the anticoagulants with their types of interference:
Which type of heparin has more specific Anti-factor Xa activity?
Which type of heparin has more specific Anti-factor Xa activity?
LMW heparins have high non-specific binding to vascular endothelium and plasma proteins. Is this statement true or false?
LMW heparins have high non-specific binding to vascular endothelium and plasma proteins. Is this statement true or false?
Which type of heparin is associated with common thrombocytopenia?
Which type of heparin is associated with common thrombocytopenia?
Flashcards are hidden until you start studying
Study Notes
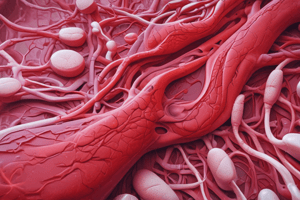
Hemostasis and Thrombosis
- Hemostasis: the process of forming a blood clot to prevent blood loss and promote healing
- Thrombosis: the unwanted formation of blood clots, which can lead to life-threatening conditions
- Types of thrombosis:
- Venous thrombosis: associated with stasis of blood, high risk of pulmonary embolism, and typically managed with anticoagulants
- Arterial thrombosis: formed at an atherosclerotic site, leading to myocardial infarction, ischemia, and infarction, and typically managed with antiplatelet agents
- Atrial fibrillation induced thrombosis: associated with stasis of blood and formation of thrombi in the left atria, leading to embolism of cerebral vessels
Phases of Blood Clot Formation
-
- Localized vasoconstriction: secretion of endothelin
-
- Primary hemostasis: formation of a primary hemostatic plug
- Platelet adhesion: enhanced by factor VIII and von Willebrand factor
- Release reaction: release of stored substances (ADP, 5-HT, fibrinogen) and newly synthesized substances (TXA2, PAF)
- Platelet aggregation: binding of fibrinogen to GPIIb–IIIa receptors on platelet membranes
-
- Secondary hemostasis (coagulation cascade): activation of thrombin and formation of a stable, permanent plug
- Endothelium and nearby cells express tissue factor, initiating the coagulation cascade
- Thrombin converts soluble fibrinogen to insoluble fibrin polymer, inducing platelet recruitment and activation
Natural Antithrombotic Mechanisms
- Antithrombin III: inactivates thrombin and other coagulation factors
- Protein C and protein S: slow the coagulation cascade by inactivating coagulation factors
- Plasmin: proteolytically cleaves fibrin into fibrin degradation products
- Tissue plasminogen activator (t-PA): activates the fibrinolytic system
- Prostacyclin (PGI2): inhibits platelet activation and vasoconstriction
- Surface heparin-like molecules: catalyze the inactivation of coagulation factors
Anticoagulants
- Interfere with coagulation factors and thrombus formation
- Examples: heparin, warfarin, fondaparinux
Heparin
- Indirect thrombin inhibitor
- Mechanism of action:
- Combines with antithrombin III, causing conformational changes that inactivate thrombin and other coagulation factors
- Pharmacological actions:
- Anticoagulant action: effective both in vitro and in vivo
- Plasma-clearing effect: stimulates lipoprotein lipase enzyme, decreasing serum triglycerides
- Pharmacokinetics:
- Immediate onset of action after IV injection, short duration (4-6 hours)
- 80% metabolized in the liver by heparinase enzyme, 20% excreted unchanged by the kidney
- Uses and routes of administration:
- Treatment of established thromboembolic disease
- Prophylaxis against thrombosis
- Adverse effects:
- Hemorrhage
- Hair loss (alopecia)
- Hematoma (if given by IM)
- Hypersensitivity
- Osteoporosis (on long-term use, especially in pregnancy)
- Hyperkalemia
- Heparin-induced thrombocytopenia (HIT)
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.