Podcast
Questions and Answers
How does blood contribute to the regulation of body temperature?
How does blood contribute to the regulation of body temperature?
- By releasing heat through sweat glands.
- By insulating the body with a layer of subcutaneous fat.
- By absorbing and redistributing heat generated by skeletal muscles. (correct)
- By constricting blood vessels to conserve heat.
Which characteristic of erythrocytes is most critical to their function of efficient gas exchange?
Which characteristic of erythrocytes is most critical to their function of efficient gas exchange?
- Their ability to consume oxygen.
- Their rapid rate of reproduction.
- Their biconcave disc shape. (correct)
- Their high concentration of glycogen.
Which sequence represents the correct ranking of white blood cells from most to least abundant in a normal differential count?
Which sequence represents the correct ranking of white blood cells from most to least abundant in a normal differential count?
- Lymphocytes, Neutrophils, Monocytes, Eosinophils, Basophils
- Neutrophils, Lymphocytes, Monocytes, Basophils, Eosinophils
- Neutrophils, Lymphocytes, Monocytes, Eosinophils, Basophils (correct)
- Neutrophils, Monocytes, Lymphocytes, Eosinophils, Basophils
Which process is directly associated with the production of formed elements?
Which process is directly associated with the production of formed elements?
How do basophils contribute to the inflammatory response at the site of an injury?
How do basophils contribute to the inflammatory response at the site of an injury?
What is the primary function of lymph nodes?
What is the primary function of lymph nodes?
Which feature is unique to lymphatic capillaries compared to blood capillaries, facilitating their role in fluid recovery?
Which feature is unique to lymphatic capillaries compared to blood capillaries, facilitating their role in fluid recovery?
What would be the most likely effect of a disease that significantly reduces the amount of albumin in the blood?
What would be the most likely effect of a disease that significantly reduces the amount of albumin in the blood?
What is the role of hemocytoblasts in the context of blood cell formation?
What is the role of hemocytoblasts in the context of blood cell formation?
What is one major functional difference between T cells and B cells?
What is one major functional difference between T cells and B cells?
Which clinical condition is characterized by a hematocrit level above 65%?
Which clinical condition is characterized by a hematocrit level above 65%?
What distinguishes granulocytes from agranulocytes?
What distinguishes granulocytes from agranulocytes?
What accounts for the viscosity of blood being approximately 5X that of water?
What accounts for the viscosity of blood being approximately 5X that of water?
Which component of haemoglobin directly participates in the binding of oxygen?
Which component of haemoglobin directly participates in the binding of oxygen?
What is the consequence of haemophilia regarding the clotting process?
What is the consequence of haemophilia regarding the clotting process?
If a patient has a blockage of lymphatic vessels, why would this lead to fluid accumulation and retention of proteins in the interstitial space?
If a patient has a blockage of lymphatic vessels, why would this lead to fluid accumulation and retention of proteins in the interstitial space?
Which structural feature ensures unidirectional lymph flow in lymphatic vessels?
Which structural feature ensures unidirectional lymph flow in lymphatic vessels?
What is the role of the spleen, beyond that of lymph nodes, in relation to blood?
What is the role of the spleen, beyond that of lymph nodes, in relation to blood?
How does inhalation aid in lymph flow?
How does inhalation aid in lymph flow?
What role do macrophages play in lymph nodes?
What role do macrophages play in lymph nodes?
What would be the primary effect of removing the thymus in an adult?
What would be the primary effect of removing the thymus in an adult?
Erythrocytes are responsible for the transport of oxygen. What is the most important structural feature that allows them to carry out their function?
Erythrocytes are responsible for the transport of oxygen. What is the most important structural feature that allows them to carry out their function?
How do the formed elements in blood relate to plasma?
How do the formed elements in blood relate to plasma?
What function is performed by the proteins dissolved in blood plasma?
What function is performed by the proteins dissolved in blood plasma?
What is the approximate blood volume of an average human?
What is the approximate blood volume of an average human?
Blood can be separated using what?
Blood can be separated using what?
In centrifuged blood, what component makes up the buffy coat?
In centrifuged blood, what component makes up the buffy coat?
In centrifuged blood, what percentage of total blood volume is Erythrocytes?
In centrifuged blood, what percentage of total blood volume is Erythrocytes?
Why do males typically have a higher blood haematocrit % compared to females?
Why do males typically have a higher blood haematocrit % compared to females?
What is the shape of an Erythrocyte?
What is the shape of an Erythrocyte?
Why does the red colour of haemoglobin change when it is exposed to oxygen?
Why does the red colour of haemoglobin change when it is exposed to oxygen?
Platelets are fragments shed from the cytoplasm of what?
Platelets are fragments shed from the cytoplasm of what?
How does the distribution of leukocytes compare between the bloodstream and connective tissue or lymphoid organs?
How does the distribution of leukocytes compare between the bloodstream and connective tissue or lymphoid organs?
Which of the following phrases describes Granulocytes?
Which of the following phrases describes Granulocytes?
Once monocytes circulate in blood for two days, what do they mature into?
Once monocytes circulate in blood for two days, what do they mature into?
What is a function of Lymphocytes?
What is a function of Lymphocytes?
What are tonsils?
What are tonsils?
Compared to veins, what do lymphatic vessels consist of?
Compared to veins, what do lymphatic vessels consist of?
Compared to blood capillaries, how do lymphatic capillaries differ?
Compared to blood capillaries, how do lymphatic capillaries differ?
What structure present in the Thymus separates lobes into lobules?
What structure present in the Thymus separates lobes into lobules?
What is the function of the spleen?
What is the function of the spleen?
Flashcards
Liquid Connective Tissue
Liquid Connective Tissue
Liquid connective tissue includes blood and lymph.
Blood Components
Blood Components
Blood components include erythrocytes, leukocytes and platelets.
Fun Facts about Blood
Fun Facts about Blood
38 degrees, 5X viscosity water, PH average 7.4 slightly alkaline (expand here) & 4-5L.
Formed Elements
Formed Elements
Signup and view all the flashcards
Blood's Transport Function
Blood's Transport Function
Signup and view all the flashcards
Blood's Regulation Function
Blood's Regulation Function
Signup and view all the flashcards
Blood's Restriction Function
Blood's Restriction Function
Signup and view all the flashcards
Blood's Defence Function
Blood's Defence Function
Signup and view all the flashcards
Blood's Temperature Regulation
Blood's Temperature Regulation
Signup and view all the flashcards
Plasma Proteins
Plasma Proteins
Signup and view all the flashcards
Blood Haematocrit
Blood Haematocrit
Signup and view all the flashcards
Anaemia & Hematocrit
Anaemia & Hematocrit
Signup and view all the flashcards
Polycythemia & Hematocrit
Polycythemia & Hematocrit
Signup and view all the flashcards
RBC
RBC
Signup and view all the flashcards
Haemoglobin
Haemoglobin
Signup and view all the flashcards
Cell source of Platelets
Cell source of Platelets
Signup and view all the flashcards
Sickle cell anaemia
Sickle cell anaemia
Signup and view all the flashcards
Leucocytes (WBC)
Leucocytes (WBC)
Signup and view all the flashcards
GRANULOCYTES
GRANULOCYTES
Signup and view all the flashcards
AGRANULOCYTES
AGRANULOCYTES
Signup and view all the flashcards
Ranking white blood cells (normal)
Ranking white blood cells (normal)
Signup and view all the flashcards
Granulocytes- Basophils
Granulocytes- Basophils
Signup and view all the flashcards
Agranulocytes- Lymphocytes
Agranulocytes- Lymphocytes
Signup and view all the flashcards
Leukaemia
Leukaemia
Signup and view all the flashcards
Haemophilia
Haemophilia
Signup and view all the flashcards
Lymphocyte producers
Lymphocyte producers
Signup and view all the flashcards
Lymph
Lymph
Signup and view all the flashcards
Lymphatic vessels
Lymphatic vessels
Signup and view all the flashcards
Lymphocyte producers
Lymphocyte producers
Signup and view all the flashcards
Study Notes
- Liquid connective tissues include blood and lymph.
- Lecture summary includes blood components, blood function, the immune system and the lymphatic system.
Classification of Adult Connective Tissue
- Connective tissues can be divided into connective tissue proper and fluid connective tissues.
- Connective tissue proper: Loose connective tissues have fibers creating a loose, open framework, including areolar, adipose, and reticular tissue where dense connective tissues have densely packed fibers including dense regular, dense irregular and elastic tissues
- Fluid connective tissues: Blood is contained in the cardiovascular system where Lymph is contained in the lymphatic system
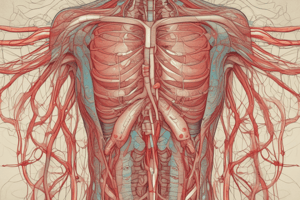
Components of Blood
- Erythrocytes (red blood cells)
- Leukocytes (white blood cells), including: Monocytes, Lymphocytes, Eosinophil, Basophil, and Neutrophil
- Platelets
Blood Facts
- Temperature of blood is 38 degrees Celcius.
- Blood is 5 times more viscous than water, with dissolved proteins and formed elements.
- Average blood pH is 7.4, slightly alkaline.
- Blood volume is aproximately 4-5 liters.
Formed Elements
- Blood cells and cell fragments suspended in plasma are formed elements.
- Red blood cells (RBCs), white blood cells (WBCs), and platelets are formed elements.
- Formed elements are produced through hematopoiesis.
- Hemocytoblasts (PSCs) differentiate into myeloid stem cells or lymphoid stem cells.
Blood Transportation in the Cardiovascular System
- Blood flows from arteries to arterioles and then to capillaries where diffusion between capillaries and interstitial fluid occurs.
- Blood flows from capillaries to venules to veins.
- Oxygenated blood flows through arteries and deoxygenated blood flows through veins.
Capillaries
- If all capillaries were aligned end to end, they would circle the earth.
Blood Function
- Blood is responsible for the transport of dissolved gases, nutrients, hormones, and metabolic waste.
- Participates in the regulation of pH and ion composition of interstitial fluid, by regulating ion levels and eliminating acid buildup
- Restricts fluid loss with enzymes that respond to breaks in vessels allowing for clotting
- Defends against pathogens and toxins with WBCs, antibodies, and specialized proteins, creating stable body temperatures by absorbing generated heat from skeletal muscles
Plasma Proteins
- Proteins in solution.
- Similar to interstitial fluid.
- Plasma contains 7.6g per 100ml of plasma.
- Interstitial fluid has five times less proteins.
- Three protein classes are Albumins, Globulins, and Fibrinogen.
- Albumins make up 60%, contribute to osmotic pressure and act as transporters.
- Globulins make up 35%, are antibodies/immuno and transport globulins.
- Fibrinogen assists in clotting and molecules interact making insoluble fibrin strands, which are a framework for a blood clot.
- 1% are other proteins with specialized functions.
Blood Hematocrit
- Blood haematocrit is the % of whole blood occupied by red blood cells.
- Females average 42%.
- Males average 46%.
- Male sex hormones (androgens) stimulate red blood cell production.
- Blood can be separated out by centrifugation.
Centrifuged Blood
- Centrifuged blood separates into Plasma (55% of total blood), Buffy Coat (leukocytes & platelets, <1% of total blood), and Erythrocytes (45% of total blood).
Clinical Relevance regarding Blood Hematocrit
- Anemia: Decreased hematocrit.
- Polycythemia: Increased hematocrit (>65%).
Red Blood Cells (RBC)
- 99% of formed element
- Contain red pigment – haemoglobin – binds O2/CO2
- 4-6 million RBC/ul
- Biconcave disc
- Large SA:volume - efficient gas exchange (total 3800 sqm)
- Very flexible
- Stack and flow
Haemoglobin
- Hemoglobin is 95% of RBC protein.
- Grams of Hb per 100ml of whole blood.
- Composed of two alpha and two beta polypeptides.
- Each Hb chain has a haem (pigment) and binds O2 - shade difference.
Blood Histology Wright's Stain or Giemsa
- Includes Erythrocytes, Neutrophils, Platelets, Basophilic myelocyte, Medium lymphocyte, Basophilic Erythroblast, Plasma cell, Small lymphocyte, Neutrophilic myelocytes and Eosinophil.
Erythropoiesis
- Erythropoiesis refers to the formation of RBCs.
- Occurs in red bone marrow.
- In extreme situations, yellow marrow converts to red marrow.
Blood Production - Haematopoiesis
- Early differentiation separates myeloid stem cells from the lymphoid stem cells.
- Multipotent stem cells in red bone marrow divide to produce specific stem cells.
- Myeloblasts, Monoblasts, and Lymphoblasts produce the White blood cells.
Clinical Relevance in Blood Production
- Sickle cell anemia: An autosomal recessive disorder.
- A mutant Hb gene leads to mutant Hb protein Hb-S.
- When Hb-S gives up O2, it forms rodlike structures.
- Results in 'Crisis'- pain and damage due to blocked capillaries.
White Blood Cells (Leukocytes)
- Role in immune system and removal of foreign and defective cells.
- Contains a nucleus.
- 6-9000/ul.
- Larger than RBC.
- Located in connective tissue proper or lymph organs.
Leukocytes
- Granulocytes include Neutrophils, Eosinophils, and basophils that contain granules that are vesicles and lysosomes
- Agranulocytes = are Monocytes and Lymphocytes that are non-granular
Ranking white blood cells
- Ranking in order = Never Let Monkeys Eat Bananas
- Neutrophils (60-70%) ; Lymphocytes (20-40%); Monocytes (3-10%); Eosinophils (1-4%); Basophils (~1%)
Granulocytes- Neutrophils
- Most common- (50-70% of WBC)
- 10-12µm diameter
- 2-5 lobed nucleus
- Lysosomal and bactericidal granules
- First to injury site AND are Cell scavengers/Phagocytes
Granulocytes- Eosinophils
- Eosin +ve granules
- Rare (2-4% of WBC)
- 10-12µM
- Exocytosis of toxic compounds AND attack antibody coated objects
- Increased in allergic conditions and internal parasitic infections
Granulocytes- Basophils
- 0-5-1% (most rare!)
- 8-10µm diameter
- migrate to injury site
- Release histamine which dilates blood vessels and heparin which prevents blood clotting
Agranulocytes- Monocytes
- 12-2µm diameter and the largest WBC
- 3-8% of WBC with a Kidney shaped nucleus
- Circulate in Blood for 2 days, then mature in tissues with a Cell-mediated immunity
- Mature into macrophages
Agranulocytes- Lymphocytes
- Smallest WBC diameter 8-10μm
- 20-30% of WBC aith a large nucleus
- B-cells - that differentiate into plasma cells (antibody production)
- T-cells - CD4 and CD8
- NK (natural killer) – immune surveillance and destruction of abnormal tissue (cancer)
Clinical Significance of WBC abnormality
- Abnormal WBC multiply uncontrollably
- Decreased normal blood cell production
Platelets
- Can look spindle shaped in smear
- Are Fragments shed from cytoplasm of megakaryocytes
- In BM, slowly sheds cytoplasm in membrane enclosed packages
- Around !4000!
- 2-4µm diameter
- Role in blood clotting – they make clotting factors which include (III, IV, V, VIII and XIII)
- Lifespan of 9-12 days
- Removed in spleen by phagocytes
Clinical Significance of Clotting
- Hereditary disorder mostly affects males
- Clotting factor formation is inadequate (factor VIII)
- Delayed clot formation can lead to hemorrhage
The Lymphatic System
- Lymphatic capillaries and vessels
- Lymphocyte producers like Lymphoid tissue and Lymphoid organs produce and distribute lymphocytes
Comparison of a small Vein and Lymphatic vessel
- Valveless Vein is filled with Erythrocytes
- Lymphatic vessel that has a Valve-like structure is filled with Lymphatic
Characteristics of Lymph
- Blood plasma components pass through capillary walls into interstitial fluid
- Concentration gradient prevents flow from interstitial fluid to blood
- Passes into permeable lymph capillaries
Collecting drainage - Lymphatic capillaries
- Capillaries deliver more liquid to tissues than they carry away and residual liquid 15% is returned via lymphatic system which Helps distribute lymphocytes, hormones, nutrients from Interstitial fluid
Characteristics of Lymphatic capillaries
- Branch through peripheral tissues but are Not present in CNS, BM or cornea
- Originate in blind pockets cul-de-sac with a Large diameter and thin endothelial walls
- Absent/incomplete basement membrane with a un-tight valve structure creating a one directional flow of Iymph
Lymphatic Vessels
- Vessels always have valves ensuring flow from trunk to thoracic cavity
- Present in almost tissue and Plasma fills interstitial fluid which flows through the lymphatic system
Lymphoid Tissue - The Tonsils
- Connective tissue that is dominated by lymphocytes that is located are large nodules in pharynx wall
- Germinal centers in area contain dividing lymphocytes.
Lymphoid Organs
- A fibrous connective tissue capsule separates these organs which include Lymph nodes, the thymus and the spleen.
Lymph Nodes
- Are shaped like Kidney beans and are Small, oval, 1-2mm
- Collagen fibers extend in the organ
- Helium is where blood attachment
- Afferent lymphatics - carry in
- Efferent lymphatics - carry lymph away
Lymph Node function
- Acts like Kitchen water filter Purifying lymph before it is sent to the venous system Removing 99% antigens
- Macrophages phagocytose AND Antigen is presented to lymphocytes which Strategically positioned to avoid infection
Thymus
- The organ is divided into Right and left lobes
- Septa separate out the lobes into lobules
- Contains many lymphocytes
- ProducesThymosin
Spleen
- Largest collection of tissue acting like lymph nodes but also performing certain function for blood.
Spleen Function
- Recycles red blood cells and Initiates of immune responses
Spleen Function Continued
- 12cm
- Contains a Capsule made of collagen and elastin and the organ is filled with Trabecula of blood vessels
- Consists of Red pulp which is blood+ fixed macrophages in network of reticular fibers
- White pulp has rich variety of immune cells
Lymph Flow
- What aids lymph flow?
- Smooth muscle contraction
- Skeletal muscle contraction
- Inhalation
Clinical significance
- Blockage of lymph vessels that causes fluid to accumulates interstitially and retain proteins leading
- Filarisis from Nematodes infecting lymph nodes which can ultimately turn into Elephantiatis
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.