Podcast
Questions and Answers
What characteristic distinguishes fibrocartilage from other types of cartilage?
What characteristic distinguishes fibrocartilage from other types of cartilage?
- Alignment of chondrocytes in rows (correct)
- High cellular density in lacunae
- Presence of a perichondrium
- Absence of collagen fibers
What is the composition of the nucleus pulposus in intervertebral discs?
What is the composition of the nucleus pulposus in intervertebral discs?
- Composed mainly of elastic fibers
- Completely avascular
- Rich in type I collagen fibers
- Contains fluid rich in hyaluronic acid (correct)
What happens to the cells when the intercellular matrix becomes calcified?
What happens to the cells when the intercellular matrix becomes calcified?
- The cells survive indefinitely.
- The cells die due to a lack of nutrients. (correct)
- The cells become more active.
- The cells regenerate immediately.
What characterizes the transformation of cartilage into an asbestos-like consistency?
What characterizes the transformation of cartilage into an asbestos-like consistency?
How does the blood supply reach fibrocartilage?
How does the blood supply reach fibrocartilage?
What is the structure surrounding the nucleus pulposus called?
What is the structure surrounding the nucleus pulposus called?
What is primarily responsible for the regeneration of cartilage when it is injured?
What is primarily responsible for the regeneration of cartilage when it is injured?
What type of matrix is predominantly associated with fibrocartilage?
What type of matrix is predominantly associated with fibrocartilage?
What type of cartilage is primarily found in the developing embryo's skeletal system?
What type of cartilage is primarily found in the developing embryo's skeletal system?
Which statement about articular hyaline cartilage is correct?
Which statement about articular hyaline cartilage is correct?
What is the primary process involved in appositional (exogenous) growth of cartilage?
What is the primary process involved in appositional (exogenous) growth of cartilage?
Which component makes osseous tissue hard and brittle?
Which component makes osseous tissue hard and brittle?
Which of the following is NOT a function of bone?
Which of the following is NOT a function of bone?
What type of bone structure is characterized by a lattice of branching spicules?
What type of bone structure is characterized by a lattice of branching spicules?
In typical long bones, where is bone marrow (BM) primarily located?
In typical long bones, where is bone marrow (BM) primarily located?
What characterizes compact bone compared to cancellous bone?
What characterizes compact bone compared to cancellous bone?
Which term describes the increase in width of cartilage through cell enlargement?
Which term describes the increase in width of cartilage through cell enlargement?
What is the primary role of the perichondrium in cartilage growth?
What is the primary role of the perichondrium in cartilage growth?
What is the initial appearance of bone during periosteal ossification?
What is the initial appearance of bone during periosteal ossification?
Which of the following statements about endochondral ossification is true?
Which of the following statements about endochondral ossification is true?
What occurs during the appearance of ossification centers in long bones?
What occurs during the appearance of ossification centers in long bones?
What structure is formed around the middle of the shaft during endochondral ossification?
What structure is formed around the middle of the shaft during endochondral ossification?
What is the relationship between fetal perichondrium and the bone collar?
What is the relationship between fetal perichondrium and the bone collar?
What type of tissue differentiates into hemopoietic tissue during periosteal ossification?
What type of tissue differentiates into hemopoietic tissue during periosteal ossification?
What does the term 'diploe' refer to in the context of ossification?
What does the term 'diploe' refer to in the context of ossification?
What signals the establishment of a center of ossification?
What signals the establishment of a center of ossification?
What is the primary function of osteoclasts during the process of primary bone destruction?
What is the primary function of osteoclasts during the process of primary bone destruction?
What is formed as a result of continued bone destruction by osteoclasts in the long bones?
What is formed as a result of continued bone destruction by osteoclasts in the long bones?
What initiates periosteal ossification?
What initiates periosteal ossification?
What structure is formed by the longitudinal cavities within compact bone matrix?
What structure is formed by the longitudinal cavities within compact bone matrix?
What distinguishes the Haversian systems from the interstitial lamellae?
What distinguishes the Haversian systems from the interstitial lamellae?
What is the function of the periosteal bud within bone development?
What is the function of the periosteal bud within bone development?
Which of the following best describes the formation of Volkmann’s canals?
Which of the following best describes the formation of Volkmann’s canals?
What primarily controls the growth in width of bone during periosteal ossification?
What primarily controls the growth in width of bone during periosteal ossification?
Flashcards are hidden until you start studying
Study Notes
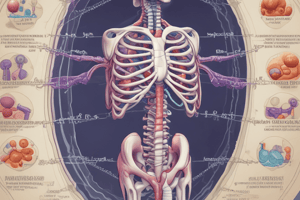
Cartilage Calcification and Transformation
- Calcium phosphate and calcium carbonate granules deposit in intercellular substances, initially near cells and later in the matrix.
- Calcification of intercellular matrix leads to cell death due to lack of nutrient diffusion.
- Transformation of cartilage can result in an asbestos-like consistency with densely packed, non-collagenous fibers, causing matrix softening or cavity formation.
Regeneration and Autografts
- Cartilage regeneration is slow, primarily involving the activity of perichondrium, essential for healing after injury.
- Autografts containing living cells can survive if adequately nourished; homografts involve similar principles of survival.
Articular Hyaline Cartilage
- Present between articulating surfaces, lacking a perichondrium where bones make contact.
- Chondrocytes, larger and centrally located, form cell families within an avascular matrix that is nourished by synovial fluid and nearby blood vessels.
Fetal Hyaline Cartilage
- Found throughout the fetal skeletal system, except in flat bones of the skull and face.
- Initially forms the skeleton from hyaline cartilage, supported by a fetal perichondrium containing numerous blood vessels and active cell division.
Fibrocartilage Structure
- Chondrocytes are dispersed singularly, in pairs, or in rows among type I collagen fibers.
- Matrix is scanty, thin, and basophilic around lacunae; blood supply comes from surrounding tissues.
Intervertebral Discs Composition
- Comprised mainly of fibrocartilage connecting the vertebrae, featuring a central gelatinous nucleus pulposus, a remnant of the embryonic notochord.
- The annulus fibrosus surrounds the nucleus, composed of concentric collagen lamellae.
- Herniation of the nucleus pulposus can cause severe pain and neurological symptoms.
Appositional Growth of Cartilage
- New cartilage layers form at the periphery from the inner chondrogenetic layer of the perichondrium, leading to increased width and cell hypertrophy.
Bone and Ossification Overview
- Bone is a rigid form of connective tissue made of cells, fibers, and a calcified extracellular matrix rich in hydroxyapatite (Ca10[PO4]6[OH]2).
- Provides internal support, protects vital organs, serves as a muscle lever system, stores minerals like calcium and phosphorus, and is involved in blood formation (hematopoiesis).
Macroscopic Structure of Bones
- Two forms of bone: cancellous (or spongy) bone, which has a lattice structure with marrow spaces, and compact bone, which appears solid until viewed microscopically.
- Long bones, like the humerus and femur, feature a thick-walled diaphysis housing a medullary cavity filled with bone marrow.
Ossification Processes
- Periosteal ossification adds layers of calcified matrix, initially forming spongy bone, which matures into compact bone.
- Intracartilaginous (endochondral) ossification involves replacing cartilage models with bone, critical for long bone development, primarily in the skeletal system.
Stages of Endochondral Ossification
- Fetal Hyaline Cartilage Formation: Begins with a mesenchymal template shaped like future bone; active cell division in perichondrium.
- Ossification Centers Appearance: In long bones, three centers typically form, including one in the shaft (diaphysis) and one in each epiphysis.
- Periosteal Band Formation: Activation of osteogenic cells in perichondrium leads to bone collar formation around the shaft.
Primary Bone Destruction and Medullary Cavity Formation
- Osteoclasts, which arise from periosteal or osteogenic buds, begin to absorb primary bone, forming a central medullary cavity lined with endosteum, containing hemopoietic elements.
Periosteal Ossification and Haversian System Formation
- Osteoblasts deposit concentric bony tissue beneath the periosteum, leading to increased bone width while osteoclasts remodel structure.
- Formation of Haversian canals and systems within compact bone, and interstitial lamellae between these structures contribute to the mature architecture of bones, facilitating blood vessel passage.
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.