Podcast
Questions and Answers
Which of the following is NOT listed as a risk factor for Benign Prostatic Hyperplasia (BPH)?
Which of the following is NOT listed as a risk factor for Benign Prostatic Hyperplasia (BPH)?
- Type 2 diabetes
- Family history of BPH
- Age 40 years and older
- Low body mass index (BMI) (correct)
What are the common urinary symptoms associated with Benign Prostatic Hyperplasia (BPH)?
What are the common urinary symptoms associated with Benign Prostatic Hyperplasia (BPH)?
Frequency, urgency, nocturia (waking up at night to urinate), and incontinence.
What potential long-term complications can arise from untreated Benign Prostatic Hyperplasia (BPH)?
What potential long-term complications can arise from untreated Benign Prostatic Hyperplasia (BPH)?
Bladder damage, kidney damage, and the formation of bladder stones.
What does a Postvoid Residual (PVR) volume test measure in the context of BPH diagnosis?
What does a Postvoid Residual (PVR) volume test measure in the context of BPH diagnosis?
An elevated Prostate-Specific Antigen (PSA) level definitively indicates prostate cancer.
An elevated Prostate-Specific Antigen (PSA) level definitively indicates prostate cancer.
Which surgical intervention for BPH involves the removal of prostate tissue through the urethra?
Which surgical intervention for BPH involves the removal of prostate tissue through the urethra?
What are key components of post-operative care following a TURP procedure?
What are key components of post-operative care following a TURP procedure?
What is the mechanism of action for Dutasteride in treating BPH?
What is the mechanism of action for Dutasteride in treating BPH?
Tamsulosin works by reducing the size of the prostate gland.
Tamsulosin works by reducing the size of the prostate gland.
What are potential adverse effects of Tamsulosin?
What are potential adverse effects of Tamsulosin?
Tadalafil should be used cautiously with Nitroglycerin (NTG).
Tadalafil should be used cautiously with Nitroglycerin (NTG).
What are the primary factors contributing to the formation of calcium oxalate kidney stones?
What are the primary factors contributing to the formation of calcium oxalate kidney stones?
Which type of kidney stone is often associated with urinary tract infections (UTIs)?
Which type of kidney stone is often associated with urinary tract infections (UTIs)?
What dietary recommendations are typically given to patients with uric acid kidney stones?
What dietary recommendations are typically given to patients with uric acid kidney stones?
What are common signs and symptoms (S/S) of renal stones?
What are common signs and symptoms (S/S) of renal stones?
Besides imaging like CT scans or ultrasound, what findings in lab tests might suggest the presence of renal stones?
Besides imaging like CT scans or ultrasound, what findings in lab tests might suggest the presence of renal stones?
What non-surgical management strategy is crucial for helping pass kidney stones and preventing future ones?
What non-surgical management strategy is crucial for helping pass kidney stones and preventing future ones?
What is the purpose of straining urine for a patient with suspected kidney stones?
What is the purpose of straining urine for a patient with suspected kidney stones?
Match the dietary component with the suggested advice for kidney stone prevention:
Match the dietary component with the suggested advice for kidney stone prevention:
What nursing interventions are important after a patient undergoes shock wave lithotripsy?
What nursing interventions are important after a patient undergoes shock wave lithotripsy?
What is percutaneous nephrolithotomy?
What is percutaneous nephrolithotomy?
Blood in the urine is an unexpected finding immediately after percutaneous nephrolithotomy and should be reported urgently.
Blood in the urine is an unexpected finding immediately after percutaneous nephrolithotomy and should be reported urgently.
What class of medication is Oxybutynin chloride, and what condition might it be used for in the context of urinary issues?
What class of medication is Oxybutynin chloride, and what condition might it be used for in the context of urinary issues?
How does Allopurinol help in the management of certain types of kidney stones?
How does Allopurinol help in the management of certain types of kidney stones?
Match the type of Acute Kidney Injury (AKI) with its potential cause:
Match the type of Acute Kidney Injury (AKI) with its potential cause:
Describe the typical urine output (UO) characteristics during the Oliguric phase of AKI.
Describe the typical urine output (UO) characteristics during the Oliguric phase of AKI.
What happens during the Diuretic phase of AKI?
What happens during the Diuretic phase of AKI?
Full recovery from Acute Kidney Injury (AKI) always occurs within a few weeks.
Full recovery from Acute Kidney Injury (AKI) always occurs within a few weeks.
What are the typical normal ranges for Serum Creatinine and Blood Urea Nitrogen (BUN)?
What are the typical normal ranges for Serum Creatinine and Blood Urea Nitrogen (BUN)?
Which electrolyte imbalance is a common and potentially life-threatening complication of AKI?
Which electrolyte imbalance is a common and potentially life-threatening complication of AKI?
Why might anemia occur in patients with kidney injury?
Why might anemia occur in patients with kidney injury?
How might dietary recommendations differ between the Oliguric and Diuretic phases of AKI?
How might dietary recommendations differ between the Oliguric and Diuretic phases of AKI?
What is the purpose of administering Erythropoietin Stimulating Agents (ESAs) like Epoetin alfa or Darbepoetin in kidney disease?
What is the purpose of administering Erythropoietin Stimulating Agents (ESAs) like Epoetin alfa or Darbepoetin in kidney disease?
What are common risk factors for developing Chronic Kidney Disease (CKD)?
What are common risk factors for developing Chronic Kidney Disease (CKD)?
Match the stage of Chronic Kidney Disease (CKD) with its corresponding Glomerular Filtration Rate (GFR) range (in mL/min/1.73m²):
Match the stage of Chronic Kidney Disease (CKD) with its corresponding Glomerular Filtration Rate (GFR) range (in mL/min/1.73m²):
What stage of CKD typically corresponds with End-Stage Renal Disease (ESRD) requiring dialysis?
What stage of CKD typically corresponds with End-Stage Renal Disease (ESRD) requiring dialysis?
Besides electrolyte imbalances (hyperkalemia, hyperphosphatemia, altered sodium), what are other common signs/symptoms of advanced CKD?
Besides electrolyte imbalances (hyperkalemia, hyperphosphatemia, altered sodium), what are other common signs/symptoms of advanced CKD?
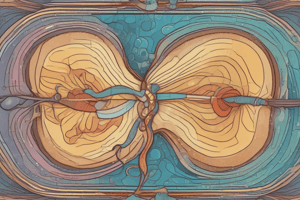
What are the two main types of dialysis used to manage ESRD?
What are the two main types of dialysis used to manage ESRD?
What is the difference between an Arteriovenous (AV) fistula and an AV graft for hemodialysis access?
What is the difference between an Arteriovenous (AV) fistula and an AV graft for hemodialysis access?
Why is it important to weigh hemodialysis patients before and after their treatment?
Why is it important to weigh hemodialysis patients before and after their treatment?
It is generally safe to administer all scheduled medications immediately before a hemodialysis session.
It is generally safe to administer all scheduled medications immediately before a hemodialysis session.
What acts as the semipermeable membrane during peritoneal dialysis?
What acts as the semipermeable membrane during peritoneal dialysis?
What are the basic steps involved in a peritoneal dialysis exchange?
What are the basic steps involved in a peritoneal dialysis exchange?
Flashcards
Benign Prostatic Hyperplasia (BPH)
Benign Prostatic Hyperplasia (BPH)
Non-cancerous enlargement of the prostate gland; common in aging men.
BPH Risk Factors
BPH Risk Factors
Risk factors include age over 40, family history, obesity, heart disease, type 2 diabetes, lack of exercise, and erectile dysfunction.
BPH Symptoms
BPH Symptoms
Symptoms include frequent urination, urgency, nocturia (nighttime urination), and incontinence.
Long-Term BPH Complications
Long-Term BPH Complications
Signup and view all the flashcards
BPH Diagnostic Tests
BPH Diagnostic Tests
Signup and view all the flashcards
BPH Management Strategies
BPH Management Strategies
Signup and view all the flashcards
Surgical Interventions for BPH
Surgical Interventions for BPH
Signup and view all the flashcards
Post-Op BPH Care
Post-Op BPH Care
Signup and view all the flashcards
BPH Medications
BPH Medications
Signup and view all the flashcards
Dutasteride
Dutasteride
Signup and view all the flashcards
Tamsulosin
Tamsulosin
Signup and view all the flashcards
Tadalafil
Tadalafil
Signup and view all the flashcards
Renal Stones
Renal Stones
Signup and view all the flashcards
Types of Kidney Stones
Types of Kidney Stones
Signup and view all the flashcards
Risk Factors for Renal Stones
Risk Factors for Renal Stones
Signup and view all the flashcards
Renal Stone Symptoms
Renal Stone Symptoms
Signup and view all the flashcards
Diagnosing Renal Stones
Diagnosing Renal Stones
Signup and view all the flashcards
Renal Stone Management
Renal Stone Management
Signup and view all the flashcards
Foods to Limit (Oxalate)
Foods to Limit (Oxalate)
Signup and view all the flashcards
Foods to Limit (Purine)
Foods to Limit (Purine)
Signup and view all the flashcards
Calcium Recommendations
Calcium Recommendations
Signup and view all the flashcards
Shock Wave Lithotripsy
Shock Wave Lithotripsy
Signup and view all the flashcards
Post-Lithotripsy Care
Post-Lithotripsy Care
Signup and view all the flashcards
Percutaneous Nephrolithotomy
Percutaneous Nephrolithotomy
Signup and view all the flashcards
Post-Op Nephrolithotomy Care
Post-Op Nephrolithotomy Care
Signup and view all the flashcards
Renal Stone Medications
Renal Stone Medications
Signup and view all the flashcards
Oxybutynin Chloride
Oxybutynin Chloride
Signup and view all the flashcards
Allopurinol
Allopurinol
Signup and view all the flashcards
Acute Kidney Injury (AKI)
Acute Kidney Injury (AKI)
Signup and view all the flashcards
AKI Pathophysiology
AKI Pathophysiology
Signup and view all the flashcards
Prerenal AKI Causes
Prerenal AKI Causes
Signup and view all the flashcards
Intrarenal AKI Causes
Intrarenal AKI Causes
Signup and view all the flashcards
Postrenal AKI Causes
Postrenal AKI Causes
Signup and view all the flashcards
Phases of AKI
Phases of AKI
Signup and view all the flashcards
Normal Kidney Lab Values
Normal Kidney Lab Values
Signup and view all the flashcards
Signs/Symptoms of AKI
Signs/Symptoms of AKI
Signup and view all the flashcards
Managing AKI
Managing AKI
Signup and view all the flashcards
AKI Medications
AKI Medications
Signup and view all the flashcards
Chronic Kidney Disease (CKD)
Chronic Kidney Disease (CKD)
Signup and view all the flashcards
CKD Pathophysiology
CKD Pathophysiology
Signup and view all the flashcards
Risk Factors for CKD
Risk Factors for CKD
Signup and view all the flashcards
Study Notes
Benign Prostatic Hyperplasia (BPH)
- Risk factors include being 40 years or older, a family history of BPH, obesity, heart disease, type 2 diabetes, lack of physical exercise, and erectile dysfunction.
- Symptoms of BPH include changes in urination, frequency, urgency, nocturia, and incontinence.
- Long-term effects stemming from BPH include bladder damage, kidney damage, and stones.
- Diagnosing BPH involves a urine flow test, postvoid residual volume test, 24-hour voiding diary, prostate-specific antigen (PSA) test, and renal labs.
- Management for BPH involves incontinence care, exercise, adequate sleep, decreased stress, good nutrition, surgery, and medications.
- Surgical interventions for BPH include transurethral resection of the prostate (TURP), transurethral incision of the prostate (TUIP), and laser photoselective vaporization of the prostate (PVP).
- Post-operative care includes a diligent bowel regimen, encouraging fluids, indwelling catheter use, and continuous irrigation.
- Medications for BPH include Dutasteride, Tamsulosin, and Tadalafil.
- Dutasteride is an antiandrogen that can take months to decrease prostate size, decreasing libido and causing gynecomastia; it has a long half-life (5 weeks).
Tamsulosin and Tadalafil
- Tamsulosin is an alpha-adrenergic blocker that relaxes smooth muscle that can take 2 weeks to see effects, adverse effects dizziness, hypotension, headache, and nausea.
- Tadalafil is a smooth muscle relaxer; adverse effects are hypotension and headache, use with NTG needs to be done carefully.
Renal Stones
- Also known as renal calculi, nephrolithiasis, or urolithiasis.
- Calcium oxalate stones are often caused by dehydration, high sodium/oxalate/protein intake, and immobility.
- Calcium phosphate stones are often caused by dehydration, high sodium/protein intake, and hyperparathyroidism.
- Uric acid stones can be caused by high purine intake and/or gout.
- Struvite stones are associated with UTIs, while cystine stones are related to genetics.
- Symptoms of renal stones include blood in urine, pain with urination, flank pain, abdominal pain, and pain radiating down the leg.
- Diagnosis involves labs for blood, albumin, or calcium in urine, as well as a CT scan or ultrasound.
- Management includes pain control, hydration, nutrition, straining urine, lithotripsy, and percutaneous nephrolithotomy.
- Diet recommendations include avoiding leafy greens, nuts, chocolate, strawberries, dried fruit, and sweet potatoes (oxalates), organ meat, gravy, red wine, sardines, and shellfish (purine); calcium intake should be at 1200mg/day.
- Post-op care includes straining urine, 3-4 L daily fluid intake, pain control, and monitoring changes in blood in urine.
- Medications include pain control- NSAIDs or opioids, oxybutynin chloride, tamsulosin, and allopurinol.
- Oxybutynin chloride adverse effects are dry mouth, constipation, nausea, dizziness/drowsiness, tachycardia, and dry eyes; avoid ETOH.
- Allopurinol inhibits uric acid production and is helpful for uric acid stones; caution with heart failure, renal failure, bone marrow depression.
Acute Kidney Injury (AKI)
- Prerenal causes: shock, heart failure, renal artery stenosis, sepsis, respiratory failure.
- Intrarenal causes: nephrotoxins, acute tubular necrosis (ATN), nephritis.
- Postrenal causes: obstruction (stones or stricture), cervical cancer, bladder atony, BPH.
- All causes lead to decreased oxygenation/perfusion and/or direct damage to renal tissue.
- Phases include onset (hours to days, normal UO), oliguric (>10-14 days, oliguria, increased BUN/Creatinine and electrolytes).
- Patients in the diuretic phase have increased UO, but it is not concentrated appropriately and labs are usually still abnormal.
- Patients in the recovery phase, can take up to 1 year for full recovery and will sometimes sustain permanent damage.
- Normal lab values include a Glomerular Filtration Rate (GFR) of > 90 mL/min/1.73m², serum creatinine of 0.8-1.2 mg/dL, Blood Urea Nitrogen (BUN) of 7-20 mg/dL, Na+ of 135-145 mEq/L, K+ of 3.5-5.0 mmol/L, and PO₄ of 3.0-4.5 mg/dL.
- Symptoms include low or no urine output, hyperkalemia, anemia, hyperphosphatemia, GI upset, mental status changes, and bleeding.
- Management involves fluid management, hemodialysis, electrolyte correction, VS monitoring, diligent I/O, and diet.
- Oliguric patients should limit salt, fluids, potassium, and phosphorous; diuretic patients may still limit salt, potassium, and phosphorous.
- Medications used are Erythropoietin stimulating agents, Epoetin alpha, Darbepoetin, Methoxy polyethylene glycol-epoetin beta, Furosemide, Spironolactone, and Hydrochlorothiazide.
Chronic Kidney Disease (CKD)
- CKD may be permanent dysfunction from AKI or may be slow onset due to vascular damage or nephrotoxic medications.
- Risk factors: diabetes, hypertension, hyperlipidemia, heart failure, SLE, sickle cell anemia, cirrhosis.
- Stages of CKD are based on GFR and lab values.
- Stage 1 is GFR > 90, with normal labs.
- Stage 2 is GFR 60-89, indicating renal insufficiency.
- Stage 3 has a GFR of 30-59, with BUN and creatinine elevated, edema, headaches, nausea, fatigue, and lower UO.
- Stage 4 has a GFR of 15-30, with elevated BUN and creatinine, anemia, potential dialysis, hypertension, and nausea/vomiting.
- Stage 5 has a GFR < 15 and definitely requires dialysis, indicating End-Stage Renal Disease (ESRD).
- Symptoms include lethargy, mental status changes, hyperkalemia, changes in phosphorous and sodium levels, pruritis, edema, and hypertension.
- Management includes hemodialysis, peritoneal dialysis, diet restrictions, fluid management, medications, symptom management, and electrolyte management.
- Medications include erythropoietin alfa, lactulose, ACEIs, ARBs, and diuretics.
- Hemodialysis involves weights before and after HD for comparison, holding medications until after HD is complete, monitoring for bleeding, and maintaining updated I/O.
- Peritoneal dialysis involves a Tenckhoff catheter, fluid warmer; it is considered more gentle than HD, and still requires VS, electrolyte, and fluid status monitoring.
- Peritoneal dialysis exchange requires sterile access, draining indwelling fluid, filling with new fluid, dwelling for a prescribed length of time.
- Four to six exchanges per day are typical either through continuous ambulatory peritoneal dialysis (CAPD) or automated peritoneal dialysis.
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.