Podcast
Questions and Answers
What is the most common route through which bacteria enter the cerebrospinal fluid (CSF)?
What is the most common route through which bacteria enter the cerebrospinal fluid (CSF)?
- Haematogenous spread (correct)
- Through a surgical procedure
- From an adjacent focus of infection
- Directly from the bloodstream
Which symptom is most likely associated with bacterial meningitis, as seen in the clinical case?
Which symptom is most likely associated with bacterial meningitis, as seen in the clinical case?
- Stiff neck
- Severe headache
- Petechial rash (correct)
- High fever
What is a key component in the management of a patient diagnosed with bacterial meningitis?
What is a key component in the management of a patient diagnosed with bacterial meningitis?
- Antibiotic therapy (correct)
- Intravenous hydration only
- Antiviral medications
- Surgical intervention
In discussing the prevention of bacterial meningitis, what should be emphasized?
In discussing the prevention of bacterial meningitis, what should be emphasized?
What differentiates meningitis from encephalitis based on their definitions?
What differentiates meningitis from encephalitis based on their definitions?
Which risk factor increases the likelihood of contracting Listeria monocytogenes during pregnancy?
Which risk factor increases the likelihood of contracting Listeria monocytogenes during pregnancy?
What specific population is most likely to asymptomatically carry Neisseria meningitidis?
What specific population is most likely to asymptomatically carry Neisseria meningitidis?
Which of the following is NOT a recognized risk factor for bacterial meningitis?
Which of the following is NOT a recognized risk factor for bacterial meningitis?
Which underlying condition increases a person's risk for invasive bacterial disease such as meningitis?
Which underlying condition increases a person's risk for invasive bacterial disease such as meningitis?
What factor is associated with a higher risk of infection for individuals traveling to sub-Saharan Africa?
What factor is associated with a higher risk of infection for individuals traveling to sub-Saharan Africa?
What is a common causative organism of meningitis in all age groups?
What is a common causative organism of meningitis in all age groups?
Which patient condition significantly increases the risk of severe infection with encapsulated bacteria?
Which patient condition significantly increases the risk of severe infection with encapsulated bacteria?
Which of the following organisms is commonly associated with meningitis in neonates?
Which of the following organisms is commonly associated with meningitis in neonates?
What is a rare cause of post-traumatic meningitis?
What is a rare cause of post-traumatic meningitis?
Which organism is considered uncommon and affects immunocompromised patients?
Which organism is considered uncommon and affects immunocompromised patients?
Diabetes mellitus has been linked to an increased risk of meningitis caused by which organism?
Diabetes mellitus has been linked to an increased risk of meningitis caused by which organism?
What is a typical feature of how bacteria cause meningitis after entering the CSF?
What is a typical feature of how bacteria cause meningitis after entering the CSF?
Which of the following factors is NOT associated with increased susceptibility to meningitis?
Which of the following factors is NOT associated with increased susceptibility to meningitis?
Which organism is commonly associated with otitis media, mastoiditis, and sinusitis?
Which organism is commonly associated with otitis media, mastoiditis, and sinusitis?
In a patient with neutropenia, which of the following organisms is least likely to be a concern?
In a patient with neutropenia, which of the following organisms is least likely to be a concern?
Which clinical feature is indicative of a brain abscess?
Which clinical feature is indicative of a brain abscess?
What non-bacterial pathogen is associated with poorly-controlled HIV infection?
What non-bacterial pathogen is associated with poorly-controlled HIV infection?
Which of the following is a sign of raised intracranial pressure?
Which of the following is a sign of raised intracranial pressure?
Which group of infections requires long-term prophylaxis with daily oral penicillin?
Which group of infections requires long-term prophylaxis with daily oral penicillin?
Which of the following is a common microbial etiology of brain abscesses from a hematogenous source?
Which of the following is a common microbial etiology of brain abscesses from a hematogenous source?
In the case of meningococcal meningitis, which prophylactic treatment is indicated for close contacts?
In the case of meningococcal meningitis, which prophylactic treatment is indicated for close contacts?
What is a key precaution when dealing with a patient suspected of having an infectious droplet spread illness?
What is a key precaution when dealing with a patient suspected of having an infectious droplet spread illness?
Which condition is NOT indicated for prophylaxis in contacts of a patient with pneumococcal meningitis?
Which condition is NOT indicated for prophylaxis in contacts of a patient with pneumococcal meningitis?
Which of the following is a likely diagnostic step for a patient presenting with confusion and seizures?
Which of the following is a likely diagnostic step for a patient presenting with confusion and seizures?
What type of exposure risk is considered for a patient with a dental abscess exhibiting neurologic symptoms?
What type of exposure risk is considered for a patient with a dental abscess exhibiting neurologic symptoms?
Which of the following best describes the microbial profile associated with anaerobic infections from a dental source?
Which of the following best describes the microbial profile associated with anaerobic infections from a dental source?
What is the main reason that lumbar puncture (LP) should be avoided in cases of brain infection?
What is the main reason that lumbar puncture (LP) should be avoided in cases of brain infection?
Which imaging modality is recommended for diagnosing brain infections?
Which imaging modality is recommended for diagnosing brain infections?
What is a common empirical antimicrobial regimen for treating brain abscess?
What is a common empirical antimicrobial regimen for treating brain abscess?
What should be done after obtaining culture and susceptibility results in a patient with a brain abscess?
What should be done after obtaining culture and susceptibility results in a patient with a brain abscess?
In cases of suspected meningococcal septicaemia, which specimen is NOT typically taken?
In cases of suspected meningococcal septicaemia, which specimen is NOT typically taken?
What is an important step in managing public health when a meningococcal infection is identified?
What is an important step in managing public health when a meningococcal infection is identified?
Identifying the source of a brain abscess is essential. What is the likely source in a patient with poor dental health?
Identifying the source of a brain abscess is essential. What is the likely source in a patient with poor dental health?
Following a brain surgery to drain an abscess, what type of specimens should be sent to the laboratory?
Following a brain surgery to drain an abscess, what type of specimens should be sent to the laboratory?
What is the primary mechanism through which bacteria commonly enter the cerebrospinal fluid (CSF)?
What is the primary mechanism through which bacteria commonly enter the cerebrospinal fluid (CSF)?
Which of the following conditions is primarily characterized by inflammation of the brain parenchyma?
Which of the following conditions is primarily characterized by inflammation of the brain parenchyma?
In which situation is prophylactic treatment for meningococcal meningitis most critical?
In which situation is prophylactic treatment for meningococcal meningitis most critical?
How should the management of a brain abscess change after the infection source has been identified?
How should the management of a brain abscess change after the infection source has been identified?
Which specimen is generally NOT collected during the initial workup for suspected meningococcal septicaemia?
Which specimen is generally NOT collected during the initial workup for suspected meningococcal septicaemia?
Which factor is associated with an increased risk of acquiring Listeria monocytogenes during pregnancy?
Which factor is associated with an increased risk of acquiring Listeria monocytogenes during pregnancy?
Which condition can increase susceptibility to bacterial meningitis due to compromised immune function?
Which condition can increase susceptibility to bacterial meningitis due to compromised immune function?
What is a common characteristic of Neisseria meningitidis in relation to certain populations?
What is a common characteristic of Neisseria meningitidis in relation to certain populations?
Which factor is unlikely to contribute to the risk of bacterial meningitis in communal living settings?
Which factor is unlikely to contribute to the risk of bacterial meningitis in communal living settings?
Which of the following is a recognized risk factor for invasive diseases such as meningitis?
Which of the following is a recognized risk factor for invasive diseases such as meningitis?
Which of the following organisms is least likely to be associated with a brain abscess following trauma or neurosurgery?
Which of the following organisms is least likely to be associated with a brain abscess following trauma or neurosurgery?
Which clinical feature is specifically indicative of an underlying infection that might lead to a brain abscess?
Which clinical feature is specifically indicative of an underlying infection that might lead to a brain abscess?
In a neutropenic patient, which of the following pathogens poses the highest risk for developing a brain abscess?
In a neutropenic patient, which of the following pathogens poses the highest risk for developing a brain abscess?
What is the most likely cause of a brain abscess in a patient with poorly-controlled HIV infection?
What is the most likely cause of a brain abscess in a patient with poorly-controlled HIV infection?
Which of the following statements about the diagnosis of brain abscess is correct?
Which of the following statements about the diagnosis of brain abscess is correct?
Which organism is commonly associated with meningitis in the elderly population?
Which organism is commonly associated with meningitis in the elderly population?
What impact does asplenia have on susceptibility to bacterial meningitis?
What impact does asplenia have on susceptibility to bacterial meningitis?
What is a common causative organism of meningitis in neonates?
What is a common causative organism of meningitis in neonates?
What is a significant host factor contributing to the recurrent infection of Neisseria meningitidis?
What is a significant host factor contributing to the recurrent infection of Neisseria meningitidis?
Which factor is associated with an increased risk of contracting Listeria monocytogenes infection?
Which factor is associated with an increased risk of contracting Listeria monocytogenes infection?
What bacterial infection is most commonly linked to skull fractures and bony defects?
What bacterial infection is most commonly linked to skull fractures and bony defects?
What type of organism is Cryptococcus neoformans considered in relation to meningitis?
What type of organism is Cryptococcus neoformans considered in relation to meningitis?
What is a potential route for bacteria to enter the cerebrospinal fluid during trauma?
What is a potential route for bacteria to enter the cerebrospinal fluid during trauma?
Which of the following is true regarding the microbial etiology of brain abscesses from hematogenous sources?
Which of the following is true regarding the microbial etiology of brain abscesses from hematogenous sources?
In which case is long-term prophylaxis with daily oral penicillin indicated?
In which case is long-term prophylaxis with daily oral penicillin indicated?
What is NOT a recognized treatment option for contacts of a meningococcal meningitis case?
What is NOT a recognized treatment option for contacts of a meningococcal meningitis case?
Which of the following droplets precautions must be taken until effective antimicrobial treatment is initiated?
Which of the following droplets precautions must be taken until effective antimicrobial treatment is initiated?
Which scenario may lead to a brain abscess secondary to contiguous infection?
Which scenario may lead to a brain abscess secondary to contiguous infection?
What is the primary source of infection in patients presenting with confusion, low-grade fever, and seizures?
What is the primary source of infection in patients presenting with confusion, low-grade fever, and seizures?
Which of the following statements about the pneumococcal vaccine is false?
Which of the following statements about the pneumococcal vaccine is false?
Which microbial pathogen group has a significant role in the development of brain abscesses due to hematogenous spread?
Which microbial pathogen group has a significant role in the development of brain abscesses due to hematogenous spread?
What is the primary reason lumbar puncture (LP) should be avoided in cases of brain infection?
What is the primary reason lumbar puncture (LP) should be avoided in cases of brain infection?
Which medicinal regimen is commonly used for empiric treatment of a brain abscess?
Which medicinal regimen is commonly used for empiric treatment of a brain abscess?
When should antimicrobial therapy be rationalised in the management of a brain abscess?
When should antimicrobial therapy be rationalised in the management of a brain abscess?
What is essential to ensure after identifying a meningococcal infection?
What is essential to ensure after identifying a meningococcal infection?
For a patient with a suspected dental source leading to a brain abscess, which specimen should be prioritized for analysis?
For a patient with a suspected dental source leading to a brain abscess, which specimen should be prioritized for analysis?
Which imaging method is recommended for diagnosing brain infections?
Which imaging method is recommended for diagnosing brain infections?
What is a likely differential diagnosis for a patient presenting with confusion and seizures, suspected to have a brain abscess?
What is a likely differential diagnosis for a patient presenting with confusion and seizures, suspected to have a brain abscess?
What is the expected duration of treatment for a brain abscess depending on clinical response?
What is the expected duration of treatment for a brain abscess depending on clinical response?
Flashcards
Bacterial Meningitis Pathogenesis
Bacterial Meningitis Pathogenesis
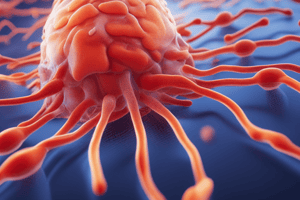
Meningitis is inflammation of the meninges (membrane covering the brain and spinal cord), often caused by bacteria that spread to the cerebrospinal fluid (CSF).
Bacterial Meningitis Clinical Presentation
Bacterial Meningitis Clinical Presentation
Symptoms include fever, headache, stiff neck, and consciousness disturbances. A petechial rash may be a crucial indicator.
Bacterial Meningitis Diagnosis
Bacterial Meningitis Diagnosis
Diagnosis involves analyzing cerebrospinal fluid (CSF) for bacteria, including culture and other assessments.
Bacterial Meningitis Management
Bacterial Meningitis Management
Signup and view all the flashcards
Brain Abscess
Brain Abscess
Signup and view all the flashcards
Meningitis Causative Organisms
Meningitis Causative Organisms
Signup and view all the flashcards
Bacterial Meningitis
Bacterial Meningitis
Signup and view all the flashcards
Viral Meningitis
Viral Meningitis
Signup and view all the flashcards
Streptococcus pneumoniae
Streptococcus pneumoniae
Signup and view all the flashcards
Neisseria meningitidis
Neisseria meningitidis
Signup and view all the flashcards
Asplenia
Asplenia
Signup and view all the flashcards
Host Factors for Meningitis
Host Factors for Meningitis
Signup and view all the flashcards
Meningitis Transmission
Meningitis Transmission
Signup and view all the flashcards
Meningitis Risk during Pregnancy
Meningitis Risk during Pregnancy
Signup and view all the flashcards
Meningitis: Who's at Risk?
Meningitis: Who's at Risk?
Signup and view all the flashcards
Meningitis: Age Factors
Meningitis: Age Factors
Signup and view all the flashcards
Meningitis: Communal Living
Meningitis: Communal Living
Signup and view all the flashcards
Meningitis: Recent Infections
Meningitis: Recent Infections
Signup and view all the flashcards
Brain Abscess: What is it?
Brain Abscess: What is it?
Signup and view all the flashcards
Brain Abscess: Common Causes
Brain Abscess: Common Causes
Signup and view all the flashcards
Brain Abscess: Signs & Symptoms
Brain Abscess: Signs & Symptoms
Signup and view all the flashcards
Brain Abscess: Diagnosis
Brain Abscess: Diagnosis
Signup and view all the flashcards
Brain Abscess: Who's at Risk?
Brain Abscess: Who's at Risk?
Signup and view all the flashcards
Pneumococcal Vaccine Impact
Pneumococcal Vaccine Impact
Signup and view all the flashcards
Pneumococcal Infection Prophylaxis
Pneumococcal Infection Prophylaxis
Signup and view all the flashcards
Asplenia Prophylaxis
Asplenia Prophylaxis
Signup and view all the flashcards
Meningococcal Prophylaxis
Meningococcal Prophylaxis
Signup and view all the flashcards
Hib Prophylaxis
Hib Prophylaxis
Signup and view all the flashcards
Droplet Precautions
Droplet Precautions
Signup and view all the flashcards
Brain Abscess: Secondary Infection
Brain Abscess: Secondary Infection
Signup and view all the flashcards
Brain Abscess: Microbial Aetiology
Brain Abscess: Microbial Aetiology
Signup and view all the flashcards
Brain Abscess: Location
Brain Abscess: Location
Signup and view all the flashcards
LP for Brain Abscess?
LP for Brain Abscess?
Signup and view all the flashcards
Brain Abscess Diagnostic Samples
Brain Abscess Diagnostic Samples
Signup and view all the flashcards
Brain Abscess Microbiology Evaluation
Brain Abscess Microbiology Evaluation
Signup and view all the flashcards
Brain Abscess: Blood Culture
Brain Abscess: Blood Culture
Signup and view all the flashcards
Brain Abscess: Imaging
Brain Abscess: Imaging
Signup and view all the flashcards
Brain Abscess: Source Control
Brain Abscess: Source Control
Signup and view all the flashcards
Brain Abscess: Antibiotic Treatment
Brain Abscess: Antibiotic Treatment
Signup and view all the flashcards
How do bacteria get into the CSF?
How do bacteria get into the CSF?
Signup and view all the flashcards
Meningitis vs. Encephalitis: Where's the inflammation?
Meningitis vs. Encephalitis: Where's the inflammation?
Signup and view all the flashcards
What is the likely diagnosis? (Clinical Case 1)
What is the likely diagnosis? (Clinical Case 1)
Signup and view all the flashcards
What specimens would you take? (Clinical Case 1)
What specimens would you take? (Clinical Case 1)
Signup and view all the flashcards
What treatment does he need? (Clinical Case 1)
What treatment does he need? (Clinical Case 1)
Signup and view all the flashcards
Listeria Meningitis Risk
Listeria Meningitis Risk
Signup and view all the flashcards
Asplenia and Meningitis
Asplenia and Meningitis
Signup and view all the flashcards
Communal Living and Meningitis
Communal Living and Meningitis
Signup and view all the flashcards
Recent Infections and Meningitis
Recent Infections and Meningitis
Signup and view all the flashcards
Meningitis Spread
Meningitis Spread
Signup and view all the flashcards
Bacterial Meningitis - Subarachnoid Space
Bacterial Meningitis - Subarachnoid Space
Signup and view all the flashcards
Common Meningitis Pathogens
Common Meningitis Pathogens
Signup and view all the flashcards
Asplenia & Meningitis Risk
Asplenia & Meningitis Risk
Signup and view all the flashcards
Other Meningitis Risk Factors
Other Meningitis Risk Factors
Signup and view all the flashcards
Meningitis: Age-Related Differences
Meningitis: Age-Related Differences
Signup and view all the flashcards
Meningitis: Geographic Variations
Meningitis: Geographic Variations
Signup and view all the flashcards
What is an intracranial shunt used for?
What is an intracranial shunt used for?
Signup and view all the flashcards
What is asplenia?
What is asplenia?
Signup and view all the flashcards
What is the difference between contiguous and hematogenous spread of brain abscesses?
What is the difference between contiguous and hematogenous spread of brain abscesses?
Signup and view all the flashcards
What are some common bacteria responsible for brain abscesses?
What are some common bacteria responsible for brain abscesses?
Signup and view all the flashcards
Brain Abscess Treatment
Brain Abscess Treatment
Signup and view all the flashcards
Prophylaxis for Meningococcal disease
Prophylaxis for Meningococcal disease
Signup and view all the flashcards
Prophylaxis for Hib disease
Prophylaxis for Hib disease
Signup and view all the flashcards
Study Notes
RCSI Bacterial Meningitis & Brain Abscess Lecture Notes
- Topic: Bacterial Meningitis & Brain Abscess
- Lecturer: Professor Karen Burns
- Date: November 13, 2024
- Course: Undergraduate Medicine
- Class: Year 2, Semester 1
Learning Outcomes
- Discuss the pathogenesis of meningitis
- Describe the causes, clinical presentation, and complications of bacterial meningitis
- Discuss the diagnosis and management of bacterial meningitis
- Discuss the prevention of bacterial meningitis and the changing local and international epidemiology
- Describe the basic clinical and microbiological features of brain abscess and how to manage the infection
Clinical Case 1
- Patient: 18-year-old male, university engineering student
- Presentation: Unconscious, petechial rash
- Living Situation: Shares a house with 4 other students
- Likely Diagnosis: Meningococcal BSI (septicaemia)
- Recommended Tests: Blood cultures, CSF
- Treatment: Ceftriaxone/cefotaxime + vancomycin + steroids
- Other Necessary Actions: Inform public health, contact tracing, prophylaxis
Clinical Case 2
- Patient: 45-year-old male engineer
- Presentation: Low-grade temperature, confused, new-onset seizure
- Reason for Seeking Care: Suspected dental abscess
- Differential Diagnoses: Brain abscess, encephalitis, tumor, stroke
- Potential Source: Dental abscess
- Tests: Blood cultures, brain pus (microbiology and histology)
- Treatment: Ceftriaxone/cefotaxime + flucloxacillin + metronidazole
Where is the Inflammation?
- Meningitis: Inflammation of the meninges (tissue surrounding the brain and spinal cord)
- Encephalitis: Inflammation of the brain parenchyma (the actual brain tissue)
- Meningoencephalitis: Inflammation of both the meninges and the brain parenchyma
How Bacteria Enter the CSF
- Haematogenous Spread (most common): From the nasopharynx or other infection site
- Spread from Adjacent Focus: Sinusitis, Mastoiditis
- Spread from Nasopharynx via Bony Defect or Head Injury: Cribriform plate (rarely)
Causative Organisms of Meningitis
- Bacteria: Severe illness, geographical and age-related differences in common organisms
- Viruses: Usually a milder illness. Referred to in other lectures.
- Fungi: Uncommon, immunocompromised patients (e.g., Cryptococcus neoformans)
- Amoebae: Very uncommon
Typical Pathogens (non-viral)
- All ages: Streptococcus pneumoniae, Neisseria meningitidis, Haemophilus influenzae type b (Hib), Group B streptococcus, E. coli, other aerobic gram-negative bacilli, Listeria monocytogenes
- Neonates: Group B streptococcus, E. coli, other aerobic gram-negative bacilli, Listeria monocytogenes
- Elderly: Streptococcus pneumoniae, Listeria monocytogenes
Host Factors Increasing Meningitis Susceptibility
- Asplenia: Increased risk of severe infection with encapsulated bacteria (Hib, S. pneumoniae, N. meningitidis)
- Diabetes Mellitus & Alcohol Abuse: Increased risk with S. pneumoniae
- Altered Cell-Mediated Immunity (Immunosuppression): Increased risk of Listeria monocytogenes,Cryptococcus neoformans
- Skull Fracture/Bony Defect: Increased risk of recurrent S. pneumoniae
- Inherited Defects in Late Complement Components: Recurrent invasive Neisseria meningitidis infection
- Pregnancy: Increased risk of invasive disease, including meningitis if Listeria monocytogenes is acquired
Risk Factors for Bacterial Meningitis
- Unvaccinated: Against Hib, MenC, MenB, MenACWY, PCV13, and PPV23 vaccination
- Age: All ages, but risk factors vary by age group and specific microorganisms
- Living in a Communal Setting: Increases risk. Examples include college dorms or military bases
- Compromised Immune System: HIV, alcohol abuse, diabetes, immunosuppressant drugs, asplenia
- Pregnancy: Increases the risk of Listeria monocytogenes infection if exposed via contaminated food
- Recent History of Infection (especially Respiratory or Ear Infection): Increased risk
- Contact with Someone with Bacterial Meningitis: Increased risk
- Head Trauma: Increased risk
- CSF Otorrhea or Rhinorrhea: Increased risk
- Travel History: Certain geographical areas have high penicillin resistance in S. pneumoniae
- Complement Pathway Deficiency, Base of Skull Fracture,
Causative Organisms: Recap
- Nisseria meningitidis: Asymptomatic carriage in nasopharynx, highest in 15-20 years. Small minority develop invasive infection. Incubation period typically 1-10 days. Person-to-person transmission.
- Streptococcus pneumoniae: Normal upper respiratory tract flora. Leading cause of meningitis in adults. May reach the CNS through bloodstream infection, chronic ear or sinus infection, after head trauma, or bony defect at the base of the skull.
- Haemophilus influenzae type b (Hib): Historically, a major cause of meningitis and epiglottitis in early childhood but vaccination has created a large impact. Still seen in poorly resourced healthcare systems
- Listeria monocytogenes: Zoonotic. Acquired by ingesting contaminated meat, meat products, vegetables, or dairy products. Pregnant women, neonates, and the elderly are at higher risk.
- Cryptococcus neoformans: Encapsulated yeast. Soil, bird droppings. Inhaled into the lungs-generally no symptoms; however may cause meningitis when the immune system is compromised, especially in those with HIV infection. Acute bacterial meningitis presentation differences- gradual onset, headache.
- Leptospira interrogans Zoonotic. Clinical features of leptospirosis which can include meningitis, lymphopcytis in CSF, consideration for renal, or hepatic failure. Clinical clues: occupation
Clinical Signs in Meningitis
- Kernig Sign: Pain or limiting extension of the leg when also flexed at the knee and hip
- Brudzinski Sign: Involuntary flexion of legs when the head/neck is flexed
Rash Associated With Meningococcal Sepsis
- Purpuric: Rash of tiny "pin pricks" transforming into purple bruising
- Non-blanching: Does not fade under pressure. DO THE GLASS TEST!
What is Sepsis?
- Infection: triggers
- Host Response:
- Organ Dysfunction:
Complications of Bacterial Meningitis
- CNS: Hearing loss, subdural abscess, cranial nerve palsies, intellectual problems, hydrocephalus, increased intracranial pressure
- Outside the CNS: Dissemination and its consequences (e.g., bloodstream infection (BSI), septic shock)
Antimicrobials Urgently
- IV antimicrobials, not oral
- Do not delay! Needed to penetrate the blood-brain barrier (BBB)
- IV steroids
Diagnosing Meningitis
- Clinical Assessment: Mainstay
- Laboratory Testing: Confirmation of clinical impression
- Lumbar Puncture (LP) to get CSF microscopy, Gram stain, culture, PCR
- Blood cultures
- Blood for PCR
Radiology
- Role in Meningitis Diagnosis: Imaging is not usually used for primary diagnosis of meningitis; its findings are not sensitive or specific. Important to consider imaging if LP is unsafe or to see if complication like abscess or ventriculitis exist.
- When Radiography is Useful: When there is concern about the safety of an LP, to assess for complications such as abscess or ventriculitis, or other intracranial issues.
Lumbar Puncture (LP)
- Contraindications: Signs of increased intracranial pressure (ICP), coagulopathy
- CSF Characteristics: Normal CSF is clear and colourless. Cloudy or turbid CSF suggests bacterial infection.
Laboratory Diagnosis of Bacterial Meningitis
- CSF Microscopy: White Blood Cell Count (WCC) and Differential WCC, Gram stain
- CSF Inoculation: Onto blood and chocolate agar plates: Identification of bacterial growth
- Blood Cultures: Incubated
- PCR: Directly on blood and CSF, results are quickly available
CSF Characteristics in Meningitis
- Bacterial Meningitis: Very elevated protein, low glucose, raised white cells (primarily neutrophils), specific micro-organisms detected by gram stain and culture and PCR.
- Viral Meningitis: Elevated protein, normal glucose, raised white cells (lymphocytes), specific virus detected by PCR or other virological tests.
- Tuberculous Meningitis: Elevated protein, low glucose, raised white cells (primarily lymphocytes), specific bacterium detected by PCR or other microbiological tests.
Treatment of Bacterial Meningitis
- Source Control: Surgical drainage (e.g., craniotomy or burr hole)
- Empiric Antimicrobials: Local guidelines, often including ceftriaxone/cefotaxime, vancomycin, and flucloxacillin in combination with metronidazole.
- Duration of Therapy: Varies based on the causative microorganism according to microbiology result
- Steroids: With/before initiation of antibiotics. May reduce complications. Specific studies show this to be particularly important in cases of Hib or Pneumococcal meningitis
Prevention of Bacterial Meningitis:
- Vaccination: Highly important. Vaccines are available for N. meningitidis, H. influenzae type b (Hib), and Streptococcus pneumoniae
- Prophylaxis: Long-term daily oral penicillin is indicated in those with underlying conditions like asplenia and immunosuppression. Prophylaxis is useful for their close contacts also. May also includes rifampicin or ciprofloxacin.
Summary
- Bacterial meningitis: Medical emergency; rapid diagnosis is critical
- Empiric antimicrobials: With steroids and resuscitation, and ICU care where necessary, for patients with meningitis
- Clinical assessment: Cell count, CSF for microscopy, biochemistry, culture and PCR testing are necessary to assess diagnosis
- Blood cultures: Necessary for diagnosis
- Vaccination: Highly effective in preventing bacterial meningitis (e.g., N. meningitidis, H. influenzae type b, Streptococcus pneumoniae).
- Brain abscess: May mimic tumor or stroke
- Source control: Surgical drainage is essential when infections in brain parenchyma occur.
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.