Podcast
Questions and Answers
What is the primary cause of autonomic dysreflexia in individuals with spinal cord lesions above T6?
What is the primary cause of autonomic dysreflexia in individuals with spinal cord lesions above T6?
- Direct injury to the spinal cord
- Inadequate hydration levels in the body
- Excessive physical activity after the injury
- Extreme stimulation of the sympathetic nervous system (correct)
Which symptom is primarily associated with the stimulation of the sympathetic nervous system during an episode of autonomic dysreflexia?
Which symptom is primarily associated with the stimulation of the sympathetic nervous system during an episode of autonomic dysreflexia?
- Bradycardia
- Blurry vision (correct)
- Flushed face
- Nasal congestion
When managing a client experiencing autonomic dysreflexia, which action should be prioritized?
When managing a client experiencing autonomic dysreflexia, which action should be prioritized?
- Assess for potential causes of dysreflexia (correct)
- Administer antihypertensives immediately
- Put the client in a standing position
- Limit fluid intake to avoid exacerbating symptoms
Which of the following factors is most commonly identified as a trigger for autonomic dysreflexia?
Which of the following factors is most commonly identified as a trigger for autonomic dysreflexia?
What is an appropriate nursing action when a client with a spinal cord lesion exhibits signs of autonomic dysreflexia?
What is an appropriate nursing action when a client with a spinal cord lesion exhibits signs of autonomic dysreflexia?
Flashcards
Autonomic Dysreflexia
Autonomic Dysreflexia
A sudden, severe increase in blood pressure, often triggered in individuals with spinal cord injuries above T6, due to stimulation in the lower body.
Cause of Dysreflexia
Cause of Dysreflexia
Often a distended bladder (blocked catheter), fecal impaction, or other lower body stimulus.
Symptoms of Dysreflexia
Symptoms of Dysreflexia
High blood pressure, severe headache, pallor below the lesion, blurred vision, sweating, and restlessness.
Nursing Action for Dysreflexia
Nursing Action for Dysreflexia
Signup and view all the flashcards
Prevention of Dysreflexia
Prevention of Dysreflexia
Signup and view all the flashcards
Study Notes
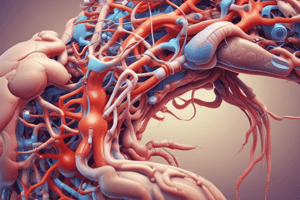
Autonomic Dysreflexia
- Occurs when the sympathetic nervous system is stimulated, but the parasympathetic system doesn't adequately respond.
- Lesions below T6 prevent dysreflexia as the parasympathetic system counteracts the sympathetic response.
- Triggers are usually stimuli from below the lesion's dermatome level.
- Symptoms include:
- Extreme hypertension
- Severe headache
- Pallor below the spinal cord lesion's dermatome
- Blurred vision
- Diaphoresis (sweating)
- Restlessness
- Nausea
- Piloerection (goosebumps)
- Parasympathetic response:
- Bradycardia
- Flushing above the spinal cord lesion's dermatome (e.g., face, neck)
- Nasal stuffiness
Nursing Actions
- Position: Sit the client upright to reduce blood pressure from postural hypotension.
- Notification: Alert the healthcare provider immediately.
- Cause Identification & Treatment: Determine and address the underlying cause.
- Distended Bladder: Common cause, address by:
- Inserting a catheter (using anesthetics)
- Checking for kinks/blockages in the catheter
- Irrigation if needed
- Fecal Impaction: Address by removing the impaction (using anesthetics).
- Environment: Adjust room temperature and block drafts. Remove tight clothing. Assess for injuries (e.g., fractures, infections).
- Monitoring: Continuous monitoring of vital signs for high blood pressure and bradycardia.
- Medication: Antihypertensives (e.g., nitrates, hydralazine) may be administered.
Client Education
- Understanding and preventing potential causes (e.g., blocked catheter, constipation) is key.
- Spreading fluid intake throughout the day is important if intake is increased, rather than drinking it all at once.
- Develop a personal action plan for episodes of dysreflexia.
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.