Podcast
Questions and Answers
What is the definition of low back pain?
What is the definition of low back pain?
- Pain and discomfort localized below the inferior gluteals folds and above the costal margins
- Pain and discomfort localized below the costal margins and above the inferior gluteals folds (correct)
- Pain and discomfort localized in the thoracic region
- Pain and discomfort localized above the costal margins and below the lumbar spine
What is radicular syndrome?
What is radicular syndrome?
- A type of osteoporosis that affects the spine
- A type of infection that affects the spine
- A type of cancer that affects the spine
- Pain that arises from compression or irritation of the nerve roots (correct)
What is a red flag for low back pain?
What is a red flag for low back pain?
- History of cancer (correct)
- Age over 60
- Previous back injury
- Family history of low back pain
What is the estimated sensitivity of the sacroiliac joint pain tests?
What is the estimated sensitivity of the sacroiliac joint pain tests?
What is the percentage of patients with low back pain who have discogenic pain?
What is the percentage of patients with low back pain who have discogenic pain?
What is centralization of symptoms?
What is centralization of symptoms?
What is the name of the test that suggests sacroiliac joint pain when 3 or more of 6 positive tests are present?
What is the name of the test that suggests sacroiliac joint pain when 3 or more of 6 positive tests are present?
What is the definition of neuropathic pain?
What is the definition of neuropathic pain?
Which of the following is a characteristic of mechanical low back pain?
Which of the following is a characteristic of mechanical low back pain?
What is a key feature of discogenic pain?
What is a key feature of discogenic pain?
Which of the following is NOT a red flag for low back pain?
Which of the following is NOT a red flag for low back pain?
What is the significance of centralization of symptoms in low back pain?
What is the significance of centralization of symptoms in low back pain?
Which of the following tests is used to suggest sacroiliac joint pain?
Which of the following tests is used to suggest sacroiliac joint pain?
What is the estimated specificity of the sacroiliac joint pain tests?
What is the estimated specificity of the sacroiliac joint pain tests?
Which of the following is a characteristic of radicular syndrome?
Which of the following is a characteristic of radicular syndrome?
What is the significance of nerve roots disorders in low back pain?
What is the significance of nerve roots disorders in low back pain?
What is a characteristic of myofascial pain?
What is a characteristic of myofascial pain?
What is the result of clinical instability in the spine?
What is the result of clinical instability in the spine?
Which of the following is associated with functional instability?
Which of the following is associated with functional instability?
What is the purpose of the positive passive lumbar extension test?
What is the purpose of the positive passive lumbar extension test?
What is the result of centralization in low back pain?
What is the result of centralization in low back pain?
What is a contributing factor to other sources of low back pain or a primary cause by itself?
What is a contributing factor to other sources of low back pain or a primary cause by itself?
What is the definition of clinical instability?
What is the definition of clinical instability?
What type of pain is characterized by the presence of trigger points?
What type of pain is characterized by the presence of trigger points?
What is the purpose of the positive passive lumbar extension test?
What is the purpose of the positive passive lumbar extension test?
What is associated with an increase in the size of the neutral zone?
What is associated with an increase in the size of the neutral zone?
Flashcards are hidden until you start studying
Study Notes
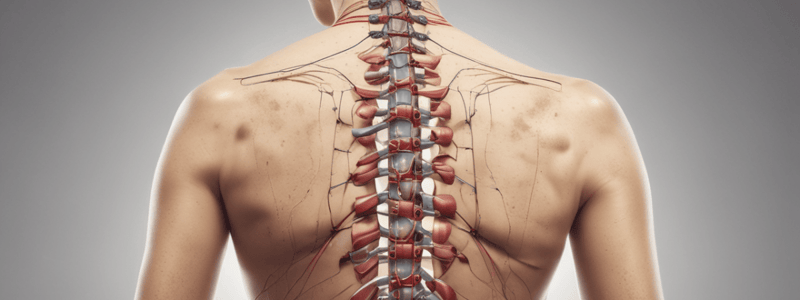
Low Back Pain
- Pain and discomfort localized below the costal margins and above the inferior gluteal folds, with or without referred leg pain.
Global Diagnostic Triage (International Guidelines)
- Serious pathology (red flags) prioritized over radicular syndrome and non-specific/mechanical low back pain.
Non-Specific/Mechanical Low Back Pain
- Not attributable to a objectively recognizable, known specific pathology (e.g., infection, tumor, osteoporosis).
- Different underlying causes, including:
- Myofascial
- Discogenic
- Sacroiliac
Red Flags
Spinal Fractures
- Major trauma
- Osteoporotic fracture
- Osteoporosis
Cancer
- History of cancer
- Multiple cancer risk factors
- Strong clinical suspicion
Infection
- Immunocompromised status
- Urinary tract infection
- Intravenous drug use
Neurophatic Pain
- Pain arising from injury or disease directly affecting the nerve roots that innervate the spine and lower limbs.
- No gold-standard approach for diagnosis.
- Distribution of pain and associated sensory or motor signs, including:
- Sensory loss
- Hyperalgesia, allodynia
- Weakness
- Numbness, tingling, electricity type pain
Nerve Roots Disorders
- Dorsal flexion worsens pain, plantar flexion makes it better.
- Flexion of head worsens pain, extension relieves it.
Mechanical Low Back Pain
- Sacroiliac joint pain suggested when 3 or more of 6 positive tests (Gaenslen's left and right, thigh thrust, sacral thrust, distraction, and iliac compression).
- Estimated sensitivity of 93.8%, specificity of 78.1%.
- Discogenic pain:
- 26%-42% of patients with low back pain
- Annular disruption and inflammatory response
- Centralization of symptoms: progressive resolution, reduction, or retreat of pain toward midline
Low Back Pain
- Pain and discomfort localized below the costal margins and above the inferior gluteal folds, with or without referred leg pain.
Global Diagnostic Triage (International Guidelines)
- Serious pathology (red flags) prioritized over radicular syndrome and non-specific/mechanical low back pain.
Non-Specific/Mechanical Low Back Pain
- Not attributable to a objectively recognizable, known specific pathology (e.g., infection, tumor, osteoporosis).
- Different underlying causes, including:
- Myofascial
- Discogenic
- Sacroiliac
Red Flags
Spinal Fractures
- Major trauma
- Osteoporotic fracture
- Osteoporosis
Cancer
- History of cancer
- Multiple cancer risk factors
- Strong clinical suspicion
Infection
- Immunocompromised status
- Urinary tract infection
- Intravenous drug use
Neurophatic Pain
- Pain arising from injury or disease directly affecting the nerve roots that innervate the spine and lower limbs.
- No gold-standard approach for diagnosis.
- Distribution of pain and associated sensory or motor signs, including:
- Sensory loss
- Hyperalgesia, allodynia
- Weakness
- Numbness, tingling, electricity type pain
Nerve Roots Disorders
- Dorsal flexion worsens pain, plantar flexion makes it better.
- Flexion of head worsens pain, extension relieves it.
Mechanical Low Back Pain
- Sacroiliac joint pain suggested when 3 or more of 6 positive tests (Gaenslen's left and right, thigh thrust, sacral thrust, distraction, and iliac compression).
- Estimated sensitivity of 93.8%, specificity of 78.1%.
- Discogenic pain:
- 26%-42% of patients with low back pain
- Annular disruption and inflammatory response
- Centralization of symptoms: progressive resolution, reduction, or retreat of pain toward midline
Centralization
- Defined as the phenomenon where a movement or position leads to the abolition of pain or the migration of symptoms from a more distal or lateral area in the buttocks and lower extremity to a more proximal location near the midline of the lumbar spine.
- Indicates a good prognosis.
Myofascial Pain
- Can be a contributing factor to other sources of low back pain (LBP) or a primary cause in itself.
- No gold standard for evaluating myofascial pain.
- Characterized by the presence of trigger points.
Lumbopelvic Instability
- Results from dysfunction in one or more of the stabilizing subsystems, leading to an increase in the size of the neutral zone.
- Comprises three subsystems:
- Passive subsystem
- Active subsystem
- Clinical instability is defined as the clinical signs and symptoms created by dysfunction of one or more of the stabilizing subsystems of the spine.
Functional Instability
- Associated with altered intervertebral discs and ligamentous support of the spine.
- Can be identified using the positive passive lumbar extension test (also known as the Prone instability test).
Centralization
- Defined as the phenomenon where a movement or position leads to the abolition of pain or the migration of symptoms from a more distal or lateral area in the buttocks and lower extremity to a more proximal location near the midline of the lumbar spine.
- Indicates a good prognosis.
Myofascial Pain
- Can be a contributing factor to other sources of low back pain (LBP) or a primary cause in itself.
- No gold standard for evaluating myofascial pain.
- Characterized by the presence of trigger points.
Lumbopelvic Instability
- Results from dysfunction in one or more of the stabilizing subsystems, leading to an increase in the size of the neutral zone.
- Comprises three subsystems:
- Passive subsystem
- Active subsystem
- Clinical instability is defined as the clinical signs and symptoms created by dysfunction of one or more of the stabilizing subsystems of the spine.
Functional Instability
- Associated with altered intervertebral discs and ligamentous support of the spine.
- Can be identified using the positive passive lumbar extension test (also known as the Prone instability test).
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.