Podcast
Questions and Answers
What is the initial process that occurs in peritonitis?
What is the initial process that occurs in peritonitis?
- Development of adhesions to wall off infection.
- Chemical irritation followed by bacterial infection. (correct)
- Fluid shifts into the abdomen causing edema.
- Bacterial infection leading to inflammation.
Which of the following is a primary cause of peritonitis?
Which of the following is a primary cause of peritonitis?
- Ruptured appendix.
- Blunt abdominal trauma.
- Perforated peptic ulcer.
- Blood borne organisms. (correct)
What is a universal sign that a patient is experiencing peritonitis?
What is a universal sign that a patient is experiencing peritonitis?
- Tenderness over the involved area. (correct)
- Muscular rigidity.
- Rebound tenderness.
- Fever.
Which finding during an abdominal x-ray may indicated peritonitis?
Which finding during an abdominal x-ray may indicated peritonitis?
What is the main goal of surgical intervention in a patient with peritonitis?
What is the main goal of surgical intervention in a patient with peritonitis?
Which laboratory result would be expected in a patient with peritonitis?
Which laboratory result would be expected in a patient with peritonitis?
Which clinical manifestation is associated with peritonitis?
Which clinical manifestation is associated with peritonitis?
What complication can occur if peritonitis is left untreated?
What complication can occur if peritonitis is left untreated?
During a physical assessment for peritonitis, what should the nurse assess regarding the patient's abdomen?
During a physical assessment for peritonitis, what should the nurse assess regarding the patient's abdomen?
Which nursing diagnosis is most appropriate for a patient experiencing peritonitis?
Which nursing diagnosis is most appropriate for a patient experiencing peritonitis?
What is the most common cause of appendicitis?
What is the most common cause of appendicitis?
Which of these signs is a classic symptom of appendicitis that is usually persistent in nature?
Which of these signs is a classic symptom of appendicitis that is usually persistent in nature?
Why are enemas and laxatives contraindicated in a patient with suspected appendicitis?
Why are enemas and laxatives contraindicated in a patient with suspected appendicitis?
What is the primary treatment for appendicitis?
What is the primary treatment for appendicitis?
What is the rationale for administering antibiotics and IV fluids prior to surgery in a patient with appendicitis?
What is the rationale for administering antibiotics and IV fluids prior to surgery in a patient with appendicitis?
Which of the following is a late complication if appendicitis is not treated promptly?
Which of the following is a late complication if appendicitis is not treated promptly?
Why is applying heat contraindicated for a patient with appendicitis?
Why is applying heat contraindicated for a patient with appendicitis?
Which of the following is a common diagnostic test used to rule out genitourinary conditions in patients with suspected appendicitis?
Which of the following is a common diagnostic test used to rule out genitourinary conditions in patients with suspected appendicitis?
What is the typical postoperative recovery time for a patient following an appendectomy?
What is the typical postoperative recovery time for a patient following an appendectomy?
What does the term 'peritonitis' refer to?
What does the term 'peritonitis' refer to?
A patient with suspected peritonitis is experiencing abdominal pain that worsens when the nurse releases pressure during palpation. This is best described as:
A patient with suspected peritonitis is experiencing abdominal pain that worsens when the nurse releases pressure during palpation. This is best described as:
Which of the following nursing interventions is MOST appropriate for a patient with peritonitis who is experiencing nausea and vomiting?
Which of the following nursing interventions is MOST appropriate for a patient with peritonitis who is experiencing nausea and vomiting?
Why is a patient with suspected peritonitis placed in a position with their knees flexed?
Why is a patient with suspected peritonitis placed in a position with their knees flexed?
A patient with peritonitis is at risk for hypovolemic shock. Which of the following assessment findings would be MOST indicative of this complication?
A patient with peritonitis is at risk for hypovolemic shock. Which of the following assessment findings would be MOST indicative of this complication?
A patient with suspected appendicitis presents with pain in the right lower quadrant. Which of these diagnostic signs is MOST likely to be elicited on assessment?
A patient with suspected appendicitis presents with pain in the right lower quadrant. Which of these diagnostic signs is MOST likely to be elicited on assessment?
A patient with a history of Crohn's disease is admitted with suspected peritonitis. What is the MOST likely cause of this complication?
A patient with a history of Crohn's disease is admitted with suspected peritonitis. What is the MOST likely cause of this complication?
Why is it important to monitor a patient with peritonitis for signs of fluid volume deficit?
Why is it important to monitor a patient with peritonitis for signs of fluid volume deficit?
Which of the following nursing interventions is MOST appropriate for a patient with peritonitis who is at risk for malnutrition?
Which of the following nursing interventions is MOST appropriate for a patient with peritonitis who is at risk for malnutrition?
What is the primary rationale for inserting a nasogastric (NG) tube in a patient with peritonitis?
What is the primary rationale for inserting a nasogastric (NG) tube in a patient with peritonitis?
Which of these signs is associated with appendicitis, but is not typically present in peritonitis?
Which of these signs is associated with appendicitis, but is not typically present in peritonitis?
Flashcards
Appendicitis
Appendicitis
Inflammation of the appendix, most common in young adults.
Causes of Appendicitis
Causes of Appendicitis
Commonly caused by obstruction of the lumen by fecaliths, foreign bodies, tumors, or lymphoid tissue growth.
McBurney’s Point
McBurney’s Point
The location in the right lower quadrant where pain from appendicitis is often felt.
Clinical Manifestations
Clinical Manifestations
Signup and view all the flashcards
Rovsing’s Sign
Rovsing’s Sign
Signup and view all the flashcards
Chemical Peritonitis
Chemical Peritonitis
Signup and view all the flashcards
Bacterial Peritonitis
Bacterial Peritonitis
Signup and view all the flashcards
Peritoneal Edema
Peritoneal Edema
Signup and view all the flashcards
Primary Causes
Primary Causes
Signup and view all the flashcards
Secondary Causes
Secondary Causes
Signup and view all the flashcards
Hypovolemic Shock
Hypovolemic Shock
Signup and view all the flashcards
Diagnostic Studies
Diagnostic Studies
Signup and view all the flashcards
Collaborative Care
Collaborative Care
Signup and view all the flashcards
Nursing Assessment
Nursing Assessment
Signup and view all the flashcards
Deficient fluid volume
Deficient fluid volume
Signup and view all the flashcards
Imbalanced nutrition
Imbalanced nutrition
Signup and view all the flashcards
Anxiety
Anxiety
Signup and view all the flashcards
Rovsing sign
Rovsing sign
Signup and view all the flashcards
Rebound tenderness
Rebound tenderness
Signup and view all the flashcards
Abdominal pain assessment
Abdominal pain assessment
Signup and view all the flashcards
Fluid replacement
Fluid replacement
Signup and view all the flashcards
NPO
NPO
Signup and view all the flashcards
Antiemetics
Antiemetics
Signup and view all the flashcards
Post-surgical drains
Post-surgical drains
Signup and view all the flashcards
Study Notes
Appendicitis
- Inflammation of the appendix
- Most common in young adults
- Morbidity and mortality rates higher in patients over 70
Etiology and Pathophysiology
- Most common cause is obstruction of the lumen by:
- Fecalith (accumulated feces)
- Foreign bodies
- Tumor of the cecum or appendix
- Excessive growth of lymphoid tissue
- Obstruction often results in:
- Distention
- Venous engorgement
- Gangrene and perforation
Clinical Manifestations
- Periumbilical pain, right lower quadrant at McBurney's point
- Persistent and continuous pain
- Anorexia
- Nausea and vomiting
- Localized or rebound tenderness
- Muscle guarding
- Pain upon sneezing, coughing, or deep inhalation
- Rovsing's sign
- Possible fever
Diagnostic Studies
- History and physical examination (palpation)
- Differential WBC count (elevated)
- Urinalysis
- Rule out genitourinary conditions
- CT scan
- Ultrasound
Complications and Treatment
- If diagnosis and treatment are delayed, complications may occur:
- Ruptured appendix
- Peritonitis
- Abscess
- Sepsis and dehydration.
- Treatment: Immediate surgical removal (appendectomy)
- Antibiotics and parenteral fluids given 6-8 hours before surgery to prevent sepsis and dehydration.
Nursing Management
- Keep patient NPO until seen by a healthcare provider
- Administer antibiotics and fluid resuscitation before surgery
- Apply ice to the area (do not use heat)
- Enemas and laxatives are not recommended, as increased peristalsis may cause perforation of appendix.
Postoperative Care
- Patient will receive a laparotomy
- Observe for signs of peritonitis
- Ambulation begins as early as the day of surgery or the first postoperative day
- Advance diet as tolerated
- Short recovery
- Discharge 1-2 days postoperative
- Normal activities resumed in 2-3 weeks
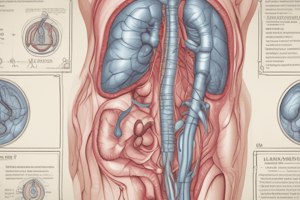
Peritonitis
- Inflammation of the peritoneum
- Occurs when intestinal contents and/or bacteria irritate the normally sterile peritoneum
- Initially chemical peritonitis followed by bacterial peritonitis
- Inflammatory response results in massive fluid shifts (peritoneal edema) and adhesions as the body attempts to wall off the infection
- Primary and secondary causes:
- Primary: Blood-borne organisms, genital tract organisms, cirrhosis with ascites
- Secondary: Appendicitis with rupture, diverticulosis with rupture, blunt/penetrating trauma to abdominal organs, ischemic bowel disorders, pancreatitis, perforated intestine (peptic ulcer), postoperative complications (e.g., anastomosis breakage)
Peritonitis Clinical Manifestations
- Abdominal pain with tenderness over involved area (universal sign)
- Rebound tenderness
- Muscular rigidity and spasms
- Shallow breaths and lack of movement
- Abdominal distention or ascites
- Fever
- Tachycardia
- Tachypnea
- Nausea and vomiting
- Altered bowel habits
Peritonitis Complications
- Hypovolemic shock
- Sepsis
- Intra-abdominal abscess formation
- Paralytic ileus
- Acute respiratory distress
- Fatal if treatment is delayed
Peritonitis Diagnostic Studies
- CBC (elevated WBCs)
- Hemoconcentration (increased concentration of cells & solids)
- Analyze fluid in peritoneal cavity via peritoneal aspiration
- X-ray of abdomen (dilated loops of bowel, free air, or air and fluid levels)
- Ultrasound
- CT scan
- Peritoneoscopy (direct examination with biopsy)
Peritonitis Collaborative Care
- Surgery: Locate cause of inflammation, drain purulent fluid, repair damage
- Antibiotics
- NG suction
- Analgesics
- IV fluid administration
Nursing Assessments(Peritonitis)
- Patient's pain (location, level, length of time)
- Bowel sounds
- Presence and quality of abdominal guarding
- Appearance of abdomen
- Nausea
- Fever
- Manifestations of hypovolemic shock
Nursing Diagnoses (Peritonitis)
- Acute pain related to inflammation of the peritoneum and abdominal distention
- Risk for deficient fluid volume related to fluid shifts into the peritoneal cavity secondary to trauma, infection, or ischemia.
- Imbalanced nutrition: less than body requirements related to anorexia, nausea, and vomiting
- Anxiety related to uncertainty of cause, outcome of condition and pain
Planning (Peritonitis)
- Nursing goals: Resolution of inflammation, relief of abdominal pain, freedom from complications (especially hypovolemic shock), and normal nutritional status
Nursing Implementation (Peritonitis)
- IV line insertion and fluid replacement
- Access for antibiotics
- Monitor patient for pain and analgesic response
- Position patient with knees flexed for comfort
- Antiemetics to decrease nausea, vomiting, and resulting fluid and electrolyte loss
- NPO and possible NG tube insertion to decrease gastric distention and further leakage of contents
- Post-surgical patient will need drains in order to remove purulent drainage for surgical patients.
NCLEX Questions and Answers
- Question 1: A patient presents with acute abdominal pain, nausea, and vomiting. A nurse palpates the patient's left lower quadrant, causing pain in the right lower quadrant. Which of the following diagnostic signs of appendicitis is this?
- Answer 1: Rovsing's sign
- Question 2: A patient with acute appendicitis. When assessing the abdomen, the nurse would expect to find rebound tenderness in which location?
- Answer 2: Right lower quadrant
- Question 3: A male client had abdominal surgery and the nurse suspects peritonitis. Which assessment data support the diagnosis of peritonitis? -Answer 3: Hard, rigid abdomen and elevated white blood cell count (22,000/mm³).
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.