Podcast
Questions and Answers
What identifies a positive fluid wave test during ascites detection?
What identifies a positive fluid wave test during ascites detection?
- Feeling a wave on the opposite side of a tap (correct)
- Dullness in the right lower quadrant
- Presence of tympany on percussion
- A protuberant abdomen
Which clinical observation is most indicative of ascites?
Which clinical observation is most indicative of ascites?
- Flat abdominal contour
- Bulging flanks of the abdomen (correct)
- Increased bowel sounds
- Presence of pain in the right lower quadrant
What is the significance of tympany versus dullness in abdominal percussion?
What is the significance of tympany versus dullness in abdominal percussion?
- Neither tympany nor dullness is relevant
- Tympany suggests presence of gas, dullness suggests fluid (correct)
- Tympany indicates free fluid, dullness indicates solid mass
- Both signify normal abdominal findings
Which technique should be performed next to confirm free fluid after percussion?
Which technique should be performed next to confirm free fluid after percussion?
What is the correct anatomical location for McBurney point?
What is the correct anatomical location for McBurney point?
What does a positive rebound tenderness indicate during the appendicitis examination?
What does a positive rebound tenderness indicate during the appendicitis examination?
When pressing firmly at McBurney point, what signifies a higher likelihood of appendicitis?
When pressing firmly at McBurney point, what signifies a higher likelihood of appendicitis?
Which statement accurately describes the purpose of the shifting dullness test?
Which statement accurately describes the purpose of the shifting dullness test?
What indicates a positive rebound tenderness during an abdominal examination?
What indicates a positive rebound tenderness during an abdominal examination?
Which location is used to assess McBurney Point Tenderness?
Which location is used to assess McBurney Point Tenderness?
What is the purpose of Rovsing sign in appendicitis assessment?
What is the purpose of Rovsing sign in appendicitis assessment?
What indicates that a patient may have appendicitis during McBurney Point assessment?
What indicates that a patient may have appendicitis during McBurney Point assessment?
During the examination for appendicitis, what does a positive Rovsing sign indicate?
During the examination for appendicitis, what does a positive Rovsing sign indicate?
What technique is utilized during the assessment of McBurney Point Tenderness?
What technique is utilized during the assessment of McBurney Point Tenderness?
What is a key finding of a positive rebound tenderness assessment?
What is a key finding of a positive rebound tenderness assessment?
Which of the following findings would suggest a need for further diagnostic testing for appendicitis?
Which of the following findings would suggest a need for further diagnostic testing for appendicitis?
What does a positive fluid wave test indicate?
What does a positive fluid wave test indicate?
Which maneuver is used to assess McBurney Point Tenderness?
Which maneuver is used to assess McBurney Point Tenderness?
Which physical examination technique assesses for Rovsing’s sign?
Which physical examination technique assesses for Rovsing’s sign?
What is the procedure for the Psoas Sign?
What is the procedure for the Psoas Sign?
What does a sharp increase in pain during Murphy's sign indicate?
What does a sharp increase in pain during Murphy's sign indicate?
Which of the following is NOT a technique used to assess appendicitis?
Which of the following is NOT a technique used to assess appendicitis?
What does shifting dullness test in a physical examination signify?
What does shifting dullness test in a physical examination signify?
Which of the following tests would you perform to identify irritations of the obturator muscle?
Which of the following tests would you perform to identify irritations of the obturator muscle?
What is the definition of dysphagia?
What is the definition of dysphagia?
Which symptom indicates odynophagia?
Which symptom indicates odynophagia?
What is the term for vomiting of blood or material that resembles coffee grounds?
What is the term for vomiting of blood or material that resembles coffee grounds?
What best describes early satiety?
What best describes early satiety?
What is a common question to assess regurgitation?
What is a common question to assess regurgitation?
Retching is best described as which of the following?
Retching is best described as which of the following?
How would one best characterize anorexia?
How would one best characterize anorexia?
What is a relevant question to ask regarding emesis?
What is a relevant question to ask regarding emesis?
What does the presence of bile in vomit indicate?
What does the presence of bile in vomit indicate?
Which of these is a characteristic of visceral pain?
Which of these is a characteristic of visceral pain?
What is the primary indication of melena?
What is the primary indication of melena?
What characterizes parietal pain compared to visceral pain?
What characterizes parietal pain compared to visceral pain?
What is the significance of a patient's overall demeanor during an abdominal inspection?
What is the significance of a patient's overall demeanor during an abdominal inspection?
In which scenario would acholic stools typically be observed?
In which scenario would acholic stools typically be observed?
What should be the initial action in the order of abdominal examination?
What should be the initial action in the order of abdominal examination?
What is an abnormal finding that may indicate an umbilical hernia?
What is an abnormal finding that may indicate an umbilical hernia?
What does the term hematochezia refer to?
What does the term hematochezia refer to?
Which statement about referred pain is accurate?
Which statement about referred pain is accurate?
Flashcards are hidden until you start studying
Study Notes
Assessing for Appendicitis
-
Positive Rebound Tenderness: Indicates peritoneal irritation, commonly associated with appendicitis when pain increases after pressure is released.
-
McBurney Point Tenderness:
- Locate McBurney point: one-third distance from the anterior superior iliac spine (ASIS) to the umbilicus on the right side.
- Firm palpation at this point increases likelihood of appendicitis if tenderness is noted.
-
Rebound Tenderness:
- Apply firm pressure at McBurney point or right lower quadrant, then quickly release.
- Increased pain upon release suggests peritoneal irritation.
Rovsing Sign
-
Objective: Assess for appendicitis through referred tenderness.
-
Procedure:
- Palpate the left lower quadrant (LLQ) with firm, slow pressure before quickly releasing.
- Assess if this causes pain in the right lower quadrant (RLQ) indicating possible appendicitis.
-
Positive Rovsing Sign: Tenderness or rebound tenderness in the RLQ upon LLQ palpation suggests appendicitis.
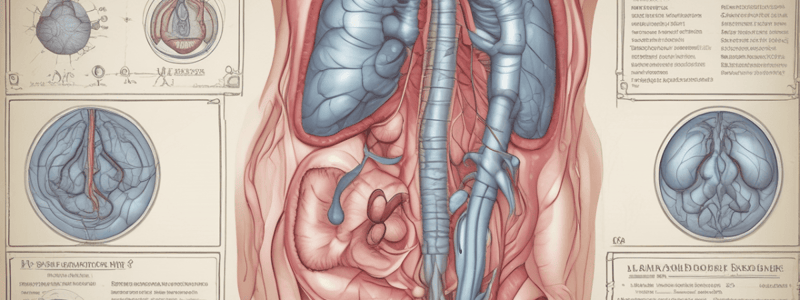
Assessing for Ascites
-
Fluid Wave Test:
- Have a hand placed on the midline of the abdomen, then tap one side while feeling for a wave on the opposite side.
- A fluid wave indicates ascites.
-
Clinical Observation: Check for a protuberant abdomen with bulging flanks.
-
Percussion:
- Perform percussion to identify areas of tympany (anterior) and dullness (lateral flanks).
-
Shifting Dullness Test: Confirms free fluid presence along with the fluid wave test.
Additional Appendicitis Signs
-
Psoas Sign:
- Patient lies on the left side and extends the right leg at the hip.
- Pain in the right lower quadrant suggests inflamed appendix irritates the psoas muscle.
-
Obturator Test:
- With the patient on their back, flex the right hip and knee, then internally rotate the hip.
- Pain in the RLQ indicates irritation of the obturator muscle by an inflamed appendix.
Assessing for Acute Cholecystitis
- Murphy's Sign:
- Place hand at the right costal margin in the mid-clavicular line.
- Patient takes a deep breath while pressure is applied; sharp pain increase or stopped inhalation due to pain suggests acute cholecystitis.
Summary of Techniques
- Ascites: Utilize shifting dullness and fluid wave tests.
- Appendicitis: Assess with McBurney point tenderness, Rovsing’s sign, Psoas sign, and Obturator test.
Upper GI Tract Terminology
- Anorexia: Lack of appetite; inquire about changes in appetite and onset.
- Early Satiety: Feeling full prematurely or general abdominal fullness; ask about fullness experience during meals.
- Dysphagia: Difficulty swallowing; check if it's painful or if food feels stuck.
- Odynophagia: Pain during swallowing; locate pain when swallowing.
- Regurgitation: Reflux of food/stomach acid; assess for sour taste and reflux instances.
- Retching: Non-productive spasmodic movements resembling vomiting; document experiences of dry heaving.
- Emesis: Vomiting; inquire about frequency, quantity, and characteristics of vomit.
- Hematemesis: Vomiting blood or coffee-ground-like material; determine appearance of vomit.
- Assess the quantity and frequency of vomiting and the type of vomit to evaluate severity and potential causes.
Lower GI Terminology
- Diarrhea: Characterized by soft or watery stools.
- Constipation: Hard stools that are difficult to pass.
- Hematochezia: Presence of fresh, bright red blood in stool.
- Melena: Black, tarry stools often indicating an upper GI bleed.
- Acholic: Pale or grey stools due to lack of bile from liver or gallbladder issues.
Abdominal Pain Characteristics
Visceral Pain
- Description: Gnawing, cramping, or aching; hard to localize.
- Causes:
- Hollow Organs: Pain from stomach or colon during contraction/distention.
- Solid Organs: Pain from swelling of liver or spleen against their capsules.
Parietal Pain
- Description: More severe and easily localized; common in appendicitis.
- Causes: Inflammation affecting parietal peritoneum from hollow/solid organs.
Referred Pain
- Description: Pain felt in different areas that share innervation.
- Example: Gallbladder pain may refer to the shoulder.
Abdominal Examination Preparation
- Room Environment: Keep the room warm with good lighting.
- Patient Preparation: Ensure bladder is empty; position patient supine with knees bent.
- Tools and Examiner Preparation: Warm stethoscope and keep nails short for patient comfort.
- Pain Consideration: Identify pain areas and examine them last.
- Order of Examination:
- Inspection
- Auscultation
- Percussion
- Palpation (to accurately assess bowel sounds).
Abdominal Inspection
- Demeanor: Observe for signs of discomfort or distress.
- Contour: Assess the abdomen's shape (flat, rounded, protuberant, scaphoid) and symmetry.
- Skin: Inspect for scars, rashes, or lesions.
- Hair Distribution: Note hair patterns on the abdomen.
- Pulsation or Movement: Look for normal aortic pulse; increased amplitude may indicate an aneurysm.
- Umbilicus: Check for bulging that may suggest an umbilical hernia and signs of inflammation.
Abnormal Findings: Umbilical Hernia
- Risk Factors:
- Infancy: Common in newborns, especially premature.
- Obesity: Increased abdominal pressure from excess weight.
- Multiple Pregnancies: Increased abdominal pressure from stretching.
- Chronic Cough or Constipation: Persistent straining raises intra-abdominal pressure.
- Previous Abdominal Surgery: Weakened abdominal wall from surgical incisions.
- Ascites: Fluid accumulation raises abdominal pressure.
- Heavy Lifting: Frequent lifting increases intra-abdominal pressure.
- Aging: Loss of muscle tone and strength in abdominal muscles.
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.