Podcast
Questions and Answers
Which factor deficiency is most likely indicated by an elevated aPTT of 58 seconds?
Which factor deficiency is most likely indicated by an elevated aPTT of 58 seconds?
- Factor XII
- Factor IX (correct)
- Factor II
- Factor VII
What does a prothrombin time (PT) of 20.4 seconds suggest in a patient’s coagulation profile?
What does a prothrombin time (PT) of 20.4 seconds suggest in a patient’s coagulation profile?
- Platelet dysfunction
- Normal coagulation function
- Deficiency in Vitamin K-dependent factors (correct)
- Fibrinogen deficiency
Which anticoagulant is a direct thrombin inhibitor and does not require INR monitoring?
Which anticoagulant is a direct thrombin inhibitor and does not require INR monitoring?
- Rivaroxaban
- Dabigatran (correct)
- Warfarin
- Enoxaparin
Which of the following anticoagulants is classified as a low molecular weight heparin?
Which of the following anticoagulants is classified as a low molecular weight heparin?
In patients with chronic kidney disease, which anticoagulant is generally preferred to avoid excessive bleeding risk?
In patients with chronic kidney disease, which anticoagulant is generally preferred to avoid excessive bleeding risk?
Which mechanism explains the action of Vitamin K antagonists like warfarin?
Which mechanism explains the action of Vitamin K antagonists like warfarin?
What is the reference range for aPTT in seconds?
What is the reference range for aPTT in seconds?
Which anticoagulant might be the best choice for Jane Doe, who is terrified of needles?
Which anticoagulant might be the best choice for Jane Doe, who is terrified of needles?
Which factor is most likely to be deficient if both PT and aPTT are prolonged?
Which factor is most likely to be deficient if both PT and aPTT are prolonged?
What is the primary laboratory test used to monitor anticoagulation with warfarin?
What is the primary laboratory test used to monitor anticoagulation with warfarin?
What is the primary goal of thrombolytics like alteplase?
What is the primary goal of thrombolytics like alteplase?
Which of the following anticoagulants is administered solely via IV formulation?
Which of the following anticoagulants is administered solely via IV formulation?
What potential risk is significantly heightened when using thrombolytics?
What potential risk is significantly heightened when using thrombolytics?
In patients requiring anticoagulation, which factor is least likely to be a concern for those on warfarin?
In patients requiring anticoagulation, which factor is least likely to be a concern for those on warfarin?
Which laboratory test is primarily used to monitor patients on unfractionated heparin?
Which laboratory test is primarily used to monitor patients on unfractionated heparin?
In the case of a patient with prolonged PT and aPTT, which factor deficiency is most likely involved if only a single factor deficiency is suspected?
In the case of a patient with prolonged PT and aPTT, which factor deficiency is most likely involved if only a single factor deficiency is suspected?
Which statement correctly describes the mechanism of action of Vitamin K antagonists like Warfarin?
Which statement correctly describes the mechanism of action of Vitamin K antagonists like Warfarin?
Which class of anticoagulants directly inhibits Factor IIa (thrombin)?
Which class of anticoagulants directly inhibits Factor IIa (thrombin)?
What is the therapeutic use of anticoagulants such as Warfarin?
What is the therapeutic use of anticoagulants such as Warfarin?
How does the aPTT test primarily relate to the coagulation cascade?
How does the aPTT test primarily relate to the coagulation cascade?
What happens to a patient when starting Warfarin therapy?
What happens to a patient when starting Warfarin therapy?
Which statement is true regarding the reversal agents for Warfarin?
Which statement is true regarding the reversal agents for Warfarin?
Which factor is important for the common pathway and has a longer half-life than others?
Which factor is important for the common pathway and has a longer half-life than others?
Which outcome is observed when initiating anticoagulation therapy with agents that affect the intrinsic pathway?
Which outcome is observed when initiating anticoagulation therapy with agents that affect the intrinsic pathway?
Which of the following agents is a synthetic pentasaccharide anticoagulant?
Which of the following agents is a synthetic pentasaccharide anticoagulant?
What does the activated partial thromboplastin time (aPTT) primarily measure?
What does the activated partial thromboplastin time (aPTT) primarily measure?
What is the normal value range for prothrombin time (PT)?
What is the normal value range for prothrombin time (PT)?
Which of the following anticoagulants works primarily by inhibiting the vitamin K dependent clotting factors?
Which of the following anticoagulants works primarily by inhibiting the vitamin K dependent clotting factors?
Which of the following is NOT a common indication for the use of anticoagulants?
Which of the following is NOT a common indication for the use of anticoagulants?
Which of the following factors is NOT part of the intrinsic pathway in the clotting cascade?
Which of the following factors is NOT part of the intrinsic pathway in the clotting cascade?
Which anticoagulant is primarily monitored by the aPTT?
Which anticoagulant is primarily monitored by the aPTT?
What is the primary role of antithrombin III in the coagulation cascade?
What is the primary role of antithrombin III in the coagulation cascade?
What type of thrombus is typically associated with myocardial infarction?
What type of thrombus is typically associated with myocardial infarction?
Flashcards
Thrombosis
Thrombosis
The most common abnormality of hemostasis, where blood clots form inside blood vessels.
Virchow's Triad
Virchow's Triad
Three factors that contribute to blood clot formation (thrombosis) : Circulatory Stasis, Hypercoagulability, and Endothelial Injury.
Clotting cascade
Clotting cascade
A series of reactions involving proteins that lead to the formation of a blood clot.
Intrinsic Pathway (aPTT)
Intrinsic Pathway (aPTT)
Signup and view all the flashcards
Extrinsic Pathway (PT)
Extrinsic Pathway (PT)
Signup and view all the flashcards
aPTT (Activated Partial Thromboplastin Time)
aPTT (Activated Partial Thromboplastin Time)
Signup and view all the flashcards
PT (Prothrombin Time)
PT (Prothrombin Time)
Signup and view all the flashcards
Hemostasis
Hemostasis
Signup and view all the flashcards
Prolonged aPTT
Prolonged aPTT
Signup and view all the flashcards
Prolonged PT
Prolonged PT
Signup and view all the flashcards
Factor VII deficiency
Factor VII deficiency
Signup and view all the flashcards
Dabigatran
Dabigatran
Signup and view all the flashcards
Enoxaparin
Enoxaparin
Signup and view all the flashcards
Fondaparinux
Fondaparinux
Signup and view all the flashcards
Rivaroxaban
Rivaroxaban
Signup and view all the flashcards
Warfarin
Warfarin
Signup and view all the flashcards
Patient concerns
Patient concerns
Signup and view all the flashcards
Chronic kidney disease (CKD)
Chronic kidney disease (CKD)
Signup and view all the flashcards
Normal INR
Normal INR
Signup and view all the flashcards
Thrombolytic Pathway
Thrombolytic Pathway
Signup and view all the flashcards
Thrombolytics (e.g., Alteplase)
Thrombolytics (e.g., Alteplase)
Signup and view all the flashcards
aPTT Elevated
aPTT Elevated
Signup and view all the flashcards
PT Elevated
PT Elevated
Signup and view all the flashcards
Alteplase Mechanism
Alteplase Mechanism
Signup and view all the flashcards
Thrombolytic Adverse Effect
Thrombolytic Adverse Effect
Signup and view all the flashcards
Anticoagulant use in Atrial Fibrillation
Anticoagulant use in Atrial Fibrillation
Signup and view all the flashcards
Vitamin K Antagonists
Vitamin K Antagonists
Signup and view all the flashcards
Warfarin's Mechanism
Warfarin's Mechanism
Signup and view all the flashcards
Warfarin Therapeutic Use
Warfarin Therapeutic Use
Signup and view all the flashcards
Warfarin Pharmacokinetics
Warfarin Pharmacokinetics
Signup and view all the flashcards
Warfarin Reversal
Warfarin Reversal
Signup and view all the flashcards
Fondaparinux Mechanism
Fondaparinux Mechanism
Signup and view all the flashcards
Study Notes
Lecture 27: Anticoagulant Pharmacology
- Instructor: Brian Skinner, PharmD, BCPS, Associate Professor of Internal Medicine, Marian University – College of Osteopathic Medicine, BMS 551 Med Phys Pharm
- Course: Fall 2024
Objectives
- Define hemostasis, clinical manifestations, and general therapeutic strategies for treatment
- Recall the three components of Virchow's Triad, and examples of each
- Diagram the clotting cascade and how anticoagulants disrupt the cascade
- Describe the roles of Antithrombin III, Protein C, and Protein S in the clotting cascade
- Relate how changes in aPTT, PT, and INR reflect in the clotting cascade, and how these are utilized for therapeutic drug monitoring
- Identify the mechanism of action, dosage form, adverse events, and contraindications for various anticoagulants and thrombolytics
- Recall the drug of choice for treatment and prophylaxis of blood clots in pregnant patients
- Identify the antidotes associated with warfarin, heparin, factor Xa inhibitors, and directed thrombin inhibitors, and how they work
- Predict the impact of Antithrombin III deficiency on pharmacotherapeutic selection
- Recommend the most appropriate pharmacotherapeutic strategy given a simplified patient case
Drug List
- Information listed in a table format regarding drug name, mechanism of action, how supplied, adverse effects/contraindications, therapeutic indications, and reversal agent(s) for several medications (Heparin, Enoxaparin, Apixaban, Rivaroxaban, Fondaparinux, Argatroban, Bivalirudin, Dabigatran, Warfarin, Alteplase). Note: information regarding Contraindications, and Safety in Pregnancy provided in table.
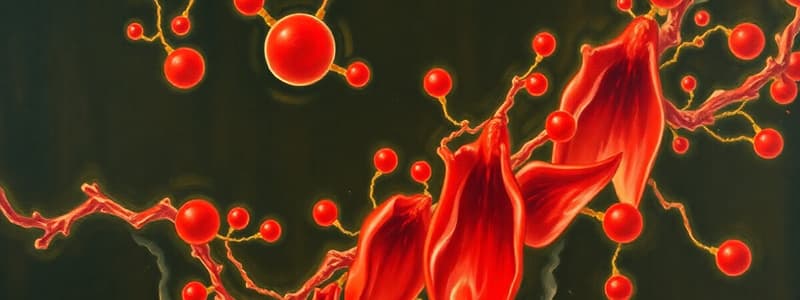
Hemostasis and Thrombosis
- Hemostasis: The stopping of blood flow
- Thrombosis: The most common abnormality of hemostasis
- Platelet-rich clots (white thrombus): Myocardial Infarction (MI), Transient Ischemic Attacks (TIAs), Peripheral Arterial Clots
- Fibrin-rich clots (red thrombus): Cardioembolic strokes from atrial fibrillation, Deep Vein Thrombosis (DVT), Pulmonary Embolism (PE)
Virchow's Triad
- Circulatory Stasis: Immobility, venous obstruction (obesity, pregnancy, tumor), varicose veins, atrial fibrillation, Cellulitis, Atherosclerosis, Venepuncture
- Endothelial Injury: Trauma
- Hypercoagulability: Surgery, malignancy, pregnancy, estrogen therapy, inherited thrombophilia
Clotting Cascade: Simplified
- Diagram of the intrinsic pathway (aPTT), extrinsic pathway (PT), and common pathway, and how different factors interconnect, leading to fibrin clot formation. Separate diagrams demonstrating inclusion of Antithrombin III and Protein C & S
Understanding Bleeding Times
- Activated Partial Thromboplastin Time (aPTT): Pathways measured, normal values (30-40 seconds), pharmacological uses
- Prothrombin Time (PT): Pathways measured, normal values (11-13.5 seconds), pharmacological uses
Comprehension Check #1
- A patient with a prolonged aPTT and a PT within normal range is likely to have an Antithrombin III deficiency or a deficiency of other particular clotting factors involved in the pathway (dependent on testing).
Anticoagulants
- Used for treating and preventing thrombotic disease
- Four main classes: Vitamin K antagonists, heparin and heparin-derived products, Factor Xa inhibitors, Direct Thrombin inhibitors
- Goal of Therapy: Prevent clot formation and allow the body to naturally break down clots over 3-6 months
Vitamin K Antagonists: Warfarin
- Inhibition of vitamin K-dependent clotting factors (II, VII, IX, X along with Protein C & S)
- Mnemonic: 2+7=9, not 10 (regarding vitamin K dependent factors)
- Reduces clotting factor production by 10-40% (due to lack of y-carboxyglutamyl side chains)
- Therapeutic Use: Treatment and prevention of DVT, PE, and cardioembolic stroke from atrial fibrillation and/or prosthetic heart valves
- Monitoring: Goal INR, is between 2 and 3 for most patients
- Adverse effects: Bleeding and Warfarin-induced skin necrosis
- Teratogenic, contraindicated in pregnancy
- Mechanism of Action: Warfarin inhibits vitamin K-dependent clotting factors, and reduces clotting factor production by 10–40% due to lack of y-carboxyglutamyl side chains.
- Reversal agent: Vitamin K1 (phytonadione), 4F-PCC, FFP (Fresh frozen plasma)
Heparin Products: Unfractionated Heparin & LMWHs (enoxaparin)
-
Antithrombin III: Responsible for inactivating Factor IIa and Xa, along with IXa, XIa, and XIIa
-
Unfractionated Heparin: Mixture of sulfated, variable length glycosaminoglycans. Acidic, Injectable ONLY
-
Prophylaxis: Subcutaneous every 8-12 hours; Lab monitoring not required
-
Used in Treatment: IV infusion to maintain aPTT 1.5-2x normal
-
LMWHs (Enoxaparin): Smaller than heparin (~4,500 daltons), available ONLY as subcutaneous injection.
-
Mechanism of action: Binding via pentasaccharide complex to antithrombin III (minimal effect on thrombin.)
-
Adverse events: Bleeding, Heparin-induced thrombocytopenia (HIT)
Fondaparinux
- Synthetically derived pentasaccharide
- Injectable formulation (subcutaneous) only
- Mechanism: Prevents activation of Factor Xa and possibly thrombin indirectly.
- Contraindicated in End Stage Renal Disease.
"Indirect" Factor Xa Inhibitors: Fondaparinux
- Mechanism: Inhibition of factor Xa via antithrombin III binding
- Indications: Treatment and prevention of DVT and PE
- Side effects: Bleeding, but NO risk for HIT. Substance renal elimination
- Contraindicated in patients with severe renal impairment
- Reversal Agent: No available agent approved for fondaparinux reversal
"Direct" Factor Xa Inhibitors: Rivaroxaban and Apixaban
- Mechanism of Action: Inhibition of factor Xa independent of antithrombin III activity
- How Supplied: Oral tablets
- Indications: Treatment and prevention of DVT, PE, and cardioembolic stroke from atrial fibrillation
- Side effects: Bleeding (risk greater with rivaroxaban), Increased risk of treatment failure in patients with empty stomach (Rivaroxaban only)
Reversal Agent: Andexanet alfa
- Dosing based on the factor Xa inhibitor dose and last dose timing
- Andexanet alfa is a truncated, inactive form of human factor Xa, with serine 149 replaced with alanine
- Removal of membrane-binding domains (y-carboxyglutamic acid)
- Binds to and sequesters factor Xa inhibitors
Direct Thrombin Inhibitors: Dabigatran etexilate
- Mechanism: Prodrug converted to dabigatran in the bloodstream
- How Supplied: Oral tablets
- Indications: Treatment and prevention of DVT, PE, and cardioembolic stroke from atrial fibrillation
- Side effects: Bleeding (higher risk than rivaroxaban and apixaban)
- Contraindicated in patients with renal dysfunction
Reversal agent: Idarucizumab
- Humanized monoclonal antibody fragment (Fab)
- Binds to and sequesters dabigatran in minutes.
Thrombolytics – Alteplase
- Treatment goal: Acutely eliminate an already-formed clot
- Reserved for high-risk patients: Acute ischemic stroke, high-risk pulmonary embolism, STEMI
- Low-dose also used for catheter clearance
- Available as an IV formulation only
- Mechanism: Initiates fibrinolysis by binding to fibrin and converting plasminogen to plasmin
- Adverse effects: INCREDIBLY HIGH risk of bleeding
- Contraindications listed
Comprehension Check #2
- Best initial treatment for a patient with CKD and atrial fibrillation should be a drug with minimal renal impact
Additional Questions
- Specific Questions Regarding Treatment Options for Patients with History of HIT.
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.