Podcast
Questions and Answers
What is the most anterior structure of the heart?
What is the most anterior structure of the heart?
- Aorta
- Right ventricle (correct)
- Pulmonary artery
- Left ventricle
What is the term for the superior aspect of the heart at the valve plane?
What is the term for the superior aspect of the heart at the valve plane?
- Apex of the heart
- Right lateral margin
- Base of the heart (correct)
- Left lateral margin
Where is the apical impulse typically located?
Where is the apical impulse typically located?
- Sixth intercostal space
- Seventh intercostal space
- Fifth intercostal space (correct)
- Fourth intercostal space
What is the significance of a PMI >2.5 cm?
What is the significance of a PMI >2.5 cm?
What is the location of the cardiac apex?
What is the location of the cardiac apex?
What is the term for the point of maximal impulse?
What is the term for the point of maximal impulse?
What is the location of the thoracic duct in relation to the heart?
What is the location of the thoracic duct in relation to the heart?
What is the location of the inferior border of the right ventricle?
What is the location of the inferior border of the right ventricle?
What occurs when the pressure in the left ventricle exceeds the pressure in the aorta?
What occurs when the pressure in the left ventricle exceeds the pressure in the aorta?
What is the normal correlation between maximal left ventricular pressure and systolic blood pressure?
What is the normal correlation between maximal left ventricular pressure and systolic blood pressure?
What produces the first heart sound, S1?
What produces the first heart sound, S1?
What is the result of the aortic valve closing?
What is the result of the aortic valve closing?
In which condition may an audible opening snap (OS) be heard?
In which condition may an audible opening snap (OS) be heard?
What may produce a third heart sound, S3, in children and young adults?
What may produce a third heart sound, S3, in children and young adults?
What is the significance of a fourth heart sound, S4?
What is the significance of a fourth heart sound, S4?
When does the tricuspid valve close?
When does the tricuspid valve close?
What is the term used to describe the mitral and tricuspid valves due to their location?
What is the term used to describe the mitral and tricuspid valves due to their location?
What is the shape of the valve leaflets of the aortic and pulmonic valves?
What is the shape of the valve leaflets of the aortic and pulmonic valves?
What is the significance of an S3 sound in a healthy adult?
What is the significance of an S3 sound in a healthy adult?
What occurs during ventricular relaxation?
What occurs during ventricular relaxation?
What is the cardiac cycle?
What is the cardiac cycle?
During systole, which valve is open and which valve is closed?
During systole, which valve is open and which valve is closed?
What corresponds to an abrupt deceleration of inflow across the mitral valve?
What corresponds to an abrupt deceleration of inflow across the mitral valve?
What corresponds to increased left ventricular end diastolic stiffness which decreases compliance?
What corresponds to increased left ventricular end diastolic stiffness which decreases compliance?
What is the primary cause of the second heart sound, S2?
What is the primary cause of the second heart sound, S2?
During which phase of respiration does the right ventricular ejection period increase?
During which phase of respiration does the right ventricular ejection period increase?
Which of the following factors contributes to the 'hangout time' that delays P2?
Which of the following factors contributes to the 'hangout time' that delays P2?
Which component of the S2 is normally louder?
Which component of the S2 is normally louder?
Where is the mitral sound of S1 best heard?
Where is the mitral sound of S1 best heard?
What is the result of the increased right heart filling time during inspiration?
What is the result of the increased right heart filling time during inspiration?
Where is the P2 component of the S2 best auscultated?
Where is the P2 component of the S2 best auscultated?
What is the result of the faster right ventricular ejection period during expiration?
What is the result of the faster right ventricular ejection period during expiration?
What is the characteristic of a stenotic valve?
What is the characteristic of a stenotic valve?
What is the location on the chest wall where you auscultate the pulmonic valve?
What is the location on the chest wall where you auscultate the pulmonic valve?
What is the term used to describe the murmur produced by blood leaking backward in a retrograde direction?
What is the term used to describe the murmur produced by blood leaking backward in a retrograde direction?
What is the typical origin of sounds at the cardiac apex?
What is the typical origin of sounds at the cardiac apex?
What is the term used to describe the characteristic sound of turbulent blood flow?
What is the term used to describe the characteristic sound of turbulent blood flow?
At which location on the chest wall do you auscultate the tricuspid valve?
At which location on the chest wall do you auscultate the tricuspid valve?
What is the effect of increased blood volume in a dilated right ventricle on preload?
What is the effect of increased blood volume in a dilated right ventricle on preload?
Which of the following decreases myocardial contractility?
Which of the following decreases myocardial contractility?
What is the primary source of resistance to ventricular contraction?
What is the primary source of resistance to ventricular contraction?
What is the term for the pathologic increase in preload?
What is the term for the pathologic increase in preload?
What is the result of pathologic increases in preload and afterload?
What is the result of pathologic increases in preload and afterload?
What is the effect of exhalation on right ventricular preload?
What is the effect of exhalation on right ventricular preload?
What is the normal range of times that the sinus node automatically discharges an impulse in one minute?
What is the normal range of times that the sinus node automatically discharges an impulse in one minute?
What is the percentage of ventricular volume ejected during each heartbeat in a normal heart?
What is the percentage of ventricular volume ejected during each heartbeat in a normal heart?
What is the term for the load that stretches the cardiac muscle before contraction?
What is the term for the load that stretches the cardiac muscle before contraction?
What is the result of increasing venous return to the right heart?
What is the result of increasing venous return to the right heart?
What is the term for the classification of heart failure based on the ejection fraction?
What is the term for the classification of heart failure based on the ejection fraction?
What is the pathway of the electrical impulse in the heart?
What is the pathway of the electrical impulse in the heart?
What is the product of heart rate and stroke volume?
What is the product of heart rate and stroke volume?
What is the muscle that the electrical conduction system stimulates and coordinates the contraction of?
What is the muscle that the electrical conduction system stimulates and coordinates the contraction of?
Flashcards are hidden until you start studying
Study Notes
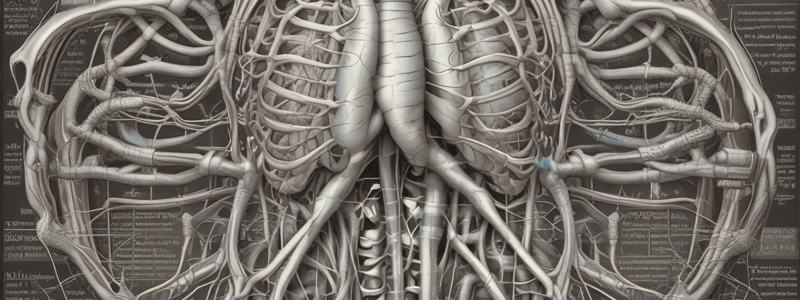
Mediastinum Structure
- Located centrally in the thoracic cavity
- Bordered by lungs on either side, sternum anteriorly, and thoracic vertebral bodies posteriorly
- Houses heart, great vessels, esophagus, trachea, thoracic duct, and thoracic lymph nodes
Heart Structure
- Right ventricle (RV) is the most anterior structure of the heart
- RV forms a wedge-like structure behind and to the left of the sternum
- Inferior border of RV lies below the junction of the sternum and the xiphoid process
- RV narrows superiorly and joins the pulmonary artery at the level of the sternal angle
- Left ventricle (LV) forms the left lateral margin of the heart
- Tapered inferior tip of LV is the cardiac apex
- Cardiac apex produces the apical impulse
Clinical Importance
- Point of maximal impulse (PMI) locates the left border of the heart
- PMI is normally found in the fifth intercostal space at or just medial to the left midclavicular line
- PMI >2.5 cm is evidence of left ventricular hypertrophy (LVH)
- Displacement of PMI lateral to the midclavicular line or >10 cm lateral to the midsternal line occurs in LVH and ventricular dilatation
- In chronic obstructive pulmonary disease (COPD), the most prominent palpable impulse may be in the xiphoid or epigastric area due to right ventricular hypertrophy
Aorta and Vena Cavae
- Aorta curves upward from the left ventricle to the level of the sternal angle
- Aorta arches posteriorly to the left and then downward
- Superior and inferior venae cavae channel venous blood from the upper and lower portions of the body into the right atrium
Cardiac Chambers, Valves, and Blood Flow
- The cardiac chambers include the left and right atria, and the left and right ventricles.
- The valves include the mitral, tricuspid, aortic, and pulmonic valves.
- The mitral and tricuspid valves are also known as atrioventricular (AV) valves.
- The aortic and pulmonic valves are also known as semilunar valves.
- Blood flows from the atria to the ventricles through the open AV valves during diastole.
- Blood flows from the ventricles to the aorta and pulmonary artery through the open aortic and pulmonic valves during systole.
Heart Sounds
- The heart sounds of S1 and S2 arise from the vibrations of the valve leaflets, adjacent cardiac structures, and the flow of blood.
- S1 corresponds to the closure of the mitral and tricuspid valves.
- S2 corresponds to the closure of the aortic and pulmonic valves.
- S3 corresponds to an abrupt deceleration of inflow across the mitral valve.
- S4 corresponds to increased left ventricular end diastolic stiffness which decreases compliance.
Cardiac Cycle
- The cardiac cycle describes the complete movement of the heart and includes the period from the beginning of one heartbeat to the beginning of the next one.
- Systole is the period of ventricular contraction when the left ventricle ejects blood into the aorta.
- Diastole is the period of ventricular relaxation when the ventricle fills with blood from the atrium.
- During systole, the aortic valve is open, and the mitral valve is closed.
- During diastole, the aortic valve is closed, and the mitral valve is open.
Valve Function
- The mitral valve opens during diastole, allowing blood to flow from the left atrium to the left ventricle.
- The mitral valve closes during systole, preventing blood from regurgitating back into the left atrium.
- The aortic valve opens during systole, allowing blood to flow from the left ventricle into the aorta.
- The aortic valve closes during diastole, preventing blood from regurgitating back into the left ventricle.
Pathological Heart Sounds
- An S3 gallop often indicates pathology in older adults.
- An S4 marks atrial contraction and can reflect a pathologic ventricular stiffness, as seen in hypertension or an acute myocardial infarction.
Heart Sounds
- Right ventricular and pulmonary arterial pressures are significantly lower than corresponding pressures on the left side of the heart.
Right-Sided Cardiac Events
- Right-sided cardiac events usually occur slightly later than those on the left side.
- During inspiration, right heart filling time is increased, which increases right ventricular stroke volume and the duration of right ventricular ejection.
Splitting of S2
- The second heart sound, S2, is caused primarily by closure of the aortic and pulmonic valves.
- S2 has two components: A2 (aortic valve closure) and P2 (pulmonic valve closure).
- During inspiration, S2 splits into its two audible components due to delayed closure of the pulmonic valve, P2.
- During expiration, A2 and P2 fuse into a single sound, S2.
- A2 is normally louder due to high pressure in the aorta and is heard throughout the precordium.
- P2 is relatively soft due to lower pressure in the pulmonary artery and is best auscultated near its anatomic location, the second and third left intercostal spaces close to the sternum.
Splitting of S1
- S1 also has two components: an earlier mitral sound and a later tricuspid sound.
- The mitral sound can be heard throughout the precordium and is loudest at the cardiac apex.
- The softer tricuspid component is heard best at the lower left sternal border.
- Splitting of S1 does not vary with respiration.
- The earlier louder mitral component may mask the tricuspid sound, so splitting is not always detectable.
Heart Murmurs
- Heart murmurs are distinct sounds produced by the heart, characterized by their pitch and longer duration.
- They are caused by turbulent blood flow and often indicate valvular heart disease.
Types of Heart Murmurs
- Stenotic murmurs occur when a valve has an abnormally narrowed orifice, obstructing blood flow (e.g., aortic stenosis).
- Regurgitant murmurs occur when a valve closes abnormally, allowing blood to leak backward in a retrograde direction.
Auscultation of Heart Sounds and Murmurs
- The location on the chest wall where heart sounds and murmurs are auscultated helps identify the valve or chamber where they originate.
Chest Wall Location and Valve Association
- Right second intercostal space or cardiac apex: Aortic valve
- Left second and third intercostal spaces close to the sternum: Pulmonic valve
- At or near the lower left sternal border: Tricuspid valve
- At and around the cardiac apex: Mitral valve
Electrical Conduction System
- The electrical conduction system stimulates and coordinates the contraction of cardiac muscle.
- The sinus node, a group of specialized cardiac cells, acts as the cardiac pacemaker, automatically discharging an impulse 60-100 times per minute.
Impulse Conduction
- The impulse travels through both atria to the AV node, a specialized group of cells located low in the atrial septum.
- The impulse is delayed at the AV node before passing down the bundle of His and its branches to the ventricular myocardium.
- Muscular contraction follows: first the atria, then the ventricles.
Cardiac Output and Stroke Volume
- Cardiac output is the volume of blood ejected from each ventricle in 1 minute.
- Cardiac output is the product of heart rate and stroke volume.
- Stroke volume is the volume of blood ejected with each heartbeat.
- Stroke volume is dependent on preload, myocardial contractility, and afterload.
Ejection Fraction
- The ejection fraction (EF) is the percentage of ventricular volume ejected during each heartbeat.
- The normal EF is 60%.
- Heart failure is classified into two distinct clinical entities based on the EF: heart failure with preserved EF and heart failure with reduced EF.
Preload, Myocardial Contractility, and Afterload
- Preload refers to the load that stretches the cardiac muscle before contraction.
- Right ventricular preload is the volume of blood in the RV at the end of diastole.
- Physiologic causes of increased right ventricular preload include inspiration and increased volume of blood flow from exercising muscles.
- Causes of decreased right ventricular preload include exhalation, dehydration, and pooling of blood in the capillary bed or the venous system.
- Myocardial contractility refers to the ability of the cardiac muscle to shorten when given a load.
- Contractility increases with sympathetic nervous system stimulation and decreases with impaired blood flow or oxygen delivery to the myocardium.
- Afterload refers to the degree of vascular resistance to ventricular contraction.
- Sources of afterload include the tone in the walls of the aorta, the large arteries, and the peripheral vascular tree, as well as the volume of blood already in the aorta.
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.