Podcast
Questions and Answers
What percentage of the total human body mass does the GI tract constitute?
What percentage of the total human body mass does the GI tract constitute?
- 15%
- 5% (correct)
- 10%
- 1%
What is the primary function of the serous fluid secreted by the serosa?
What is the primary function of the serous fluid secreted by the serosa?
- To regulate blood flow to the gut
- To modulate gut motility
- To reduce friction between muscle movements (correct)
- To facilitate digestion
What is the function of the longitudinal muscle layer in the GI tract?
What is the function of the longitudinal muscle layer in the GI tract?
- To shorten the length of the intestinal segment (correct)
- To facilitate gut excretion
- To increase the diameter of the intestinal lumen
- To regulate gut absorption
What is the location of the myenteric (Auerbach) plexus in the GI tract?
What is the location of the myenteric (Auerbach) plexus in the GI tract?
What is the function of the submucosal (Meissner) plexus in the GI tract?
What is the function of the submucosal (Meissner) plexus in the GI tract?
What is the innermost layer of the GI tract wall?
What is the innermost layer of the GI tract wall?
What is the primary function of the muscularis mucosa in the mucosa?
What is the primary function of the muscularis mucosa in the mucosa?
Which part of the autonomic nervous system is primarily inhibitory to GI motility?
Which part of the autonomic nervous system is primarily inhibitory to GI motility?
What is the primary neurotransmitter of the parasympathetic nervous system in the GI tract?
What is the primary neurotransmitter of the parasympathetic nervous system in the GI tract?
Where do the preganglionic fibers of the sympathetic nervous system originate?
Where do the preganglionic fibers of the sympathetic nervous system originate?
Which nerve fibers innervate the second half of the large intestine, sigmoid, rectal, and anal regions?
Which nerve fibers innervate the second half of the large intestine, sigmoid, rectal, and anal regions?
What is the function of the lamina propria in the mucosa?
What is the function of the lamina propria in the mucosa?
What is the primary function of the myenteric plexus in the GI tract?
What is the primary function of the myenteric plexus in the GI tract?
What is the effect of sympathetic stimulation on the GI tract?
What is the effect of sympathetic stimulation on the GI tract?
What is the role of interstitial cells of Cajal in the GI tract?
What is the role of interstitial cells of Cajal in the GI tract?
How do sympathetic and parasympathetic stimulation affect the enteric nervous system?
How do sympathetic and parasympathetic stimulation affect the enteric nervous system?
What is the mechanism by which sympathetic stimulation inhibits the release of acetylcholine, increases the tone of the wall and contract the sphincter ?
What is the mechanism by which sympathetic stimulation inhibits the release of acetylcholine, increases the tone of the wall and contract the sphincter ?
What is the effect of parasympathetic stimulation on the GI tract?
What is the effect of parasympathetic stimulation on the GI tract?
What is the approximate length of the esophagus?
What is the approximate length of the esophagus?
Which region of the esophagus is approximately 4 to 5 cm long and is surrounded by the trachea anteriorly?
Which region of the esophagus is approximately 4 to 5 cm long and is surrounded by the trachea anteriorly?
In which region of the esophagus does it deviate to the right to allow room for the aortic arch?
In which region of the esophagus does it deviate to the right to allow room for the aortic arch?
What is the composition of the upper one-third of the esophagus?
What is the composition of the upper one-third of the esophagus?
What is the location of the upper esophageal sphincter (UES)?
What is the location of the upper esophageal sphincter (UES)?
What is the range of the resting tone of the upper esophageal sphincter (UES)?
What is the range of the resting tone of the upper esophageal sphincter (UES)?
What is the main component of the lower esophageal sphincter (LES)?
What is the main component of the lower esophageal sphincter (LES)?
What is the primary function of the upper esophageal sphincter (UES) in relation to food movement?
What is the primary function of the upper esophageal sphincter (UES) in relation to food movement?
What is the range of the resting tone of the lower esophageal sphincter (LES)?
What is the range of the resting tone of the lower esophageal sphincter (LES)?
Which muscles make up the upper esophageal sphincter (UES)?
Which muscles make up the upper esophageal sphincter (UES)?
What type of innervation does the lower esophageal sphincter (LES) have?
What type of innervation does the lower esophageal sphincter (LES) have?
What is the primary function of the proximal stomach?
What is the primary function of the proximal stomach?
What is the minimum particle size required for food to enter the small intestine?
What is the minimum particle size required for food to enter the small intestine?
Which cell type in the stomach produces hydrochloric acid?
Which cell type in the stomach produces hydrochloric acid?
What is the capacity of the stomach to store food?
What is the capacity of the stomach to store food?
What is the outcome of the stomach's digestive process on food?
What is the outcome of the stomach's digestive process on food?
What is the primary function of mucous cells in the stomach?
What is the primary function of mucous cells in the stomach?
What is the primary function of chief cells in the stomach?
What is the primary function of chief cells in the stomach?
What is the minimum particle size required for food to enter the small intestine?
What is the minimum particle size required for food to enter the small intestine?
Which cell type in the stomach secretes gastrin?
Which cell type in the stomach secretes gastrin?
What is the level of the vertebrae at which the esophagus extends from the hypopharynx?
What is the level of the vertebrae at which the esophagus extends from the hypopharynx?
What is the length of the cervical esophagus?
What is the length of the cervical esophagus?
Where does the thoracic esophagus lie in relation to the trachea?
Where does the thoracic esophagus lie in relation to the trachea?
What is the level of the vertebrae at which the esophagus runs anterior to the aorta?
What is the level of the vertebrae at which the esophagus runs anterior to the aorta?
What is the name of the junction where the esophagus ends?
What is the name of the junction where the esophagus ends?
Where do the digestive enzymes from the pancreas, liver, and gallbladder enter the small intestine?
Where do the digestive enzymes from the pancreas, liver, and gallbladder enter the small intestine?
What percentage of available nutrients are absorbed by the jejunum ?
What percentage of available nutrients are absorbed by the jejunum ?
What is the primary function of the jejunum in the small intestine?
What is the primary function of the jejunum in the small intestine?
What is the purpose of the ileocecal valve?
What is the purpose of the ileocecal valve?
How does the jejunum increase its surface area for absorption?
How does the jejunum increase its surface area for absorption?
absorbtion of vitamin B12 occur mainly in ?
absorbtion of vitamin B12 occur mainly in ?
What is the primary function of the cecum in the large intestine?
What is the primary function of the cecum in the large intestine?
What is the function of the contractions of the transverse colon?
What is the function of the contractions of the transverse colon?
What is the primary function of the sigmoid colon?
What is the primary function of the sigmoid colon?
What happens when fecal matter accumulates in the rectum?
What happens when fecal matter accumulates in the rectum?
What is the role of the ascending colon in the large intestine?
What is the role of the ascending colon in the large intestine?
What happens to the fecal matter in the transverse colon?
What happens to the fecal matter in the transverse colon?
Study Notes
- The esophagus is a muscular tube that connects the pharynx to the stomach, measuring approximately 18-25 cm in length.
- The esophagus extends from the level of the hypopharynx at the C6 vertebrae down to the gastroesophageal (GE) junction at the T11 level.
- The esophagus has three regions: cervical, thoracic, and abdominal, with the cervical esophagus being approximately 4-5 cm long and surrounded by the trachea, vertebral column, carotid sheaths, and thyroid gland.
- The upper one-third of the esophagus is composed of striated muscle, and the remaining two-thirds is smooth muscle.
- There are two areas of high pressure in the esophagus: the upper esophageal sphincter (UES) and the lower esophageal sphincter (LES), with resting tone ranging from 30-200 mm Hg for the UES and 10-45 mm Hg for the LES.
- The stomach is a J-shaped dilation of the alimentary tract, divided into four regions: the cardia, fundus, body or corpus, and antrum.
- The stomach has three main functions: storing large quantities of food, mixing food with gastric secretions to form chyme, and slowing emptying into the small intestine.
- Notable cell types in the stomach that aid in digestion include mucous cells, parietal cells, chief cells, and G cells, which together break down and partially digest food into chyme.
- The duodenum is the first and smallest section of the small intestine, measuring between 25-30 cm long, and forms a C-shaped loop around the pancreas.
- The duodenum's main function is to chemically digest the chyme received from the stomach in preparation for absorption, with the pancreas, liver, and gallbladder secreting digestive enzymes through the ampulla of Vater.
- The jejunum is the second section of the small intestine, and its primary function is to absorb nutrients, with the walls of the jejunum folded many times over to increase its surface area for maximal absorption.
- The ileum is the final section of the small intestine, serving to absorb vitamin B12 and other products of digestion that were not previously absorbed in the jejunum.
- The large intestine is composed of the cecum, appendix, ascending colon, transverse colon, descending colon, sigmoid colon, and rectum.
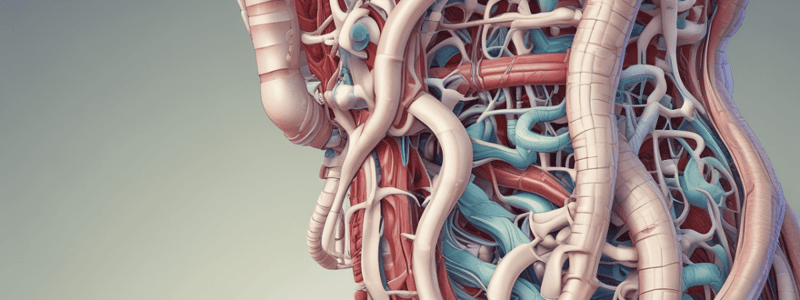
- The GI tract constitutes approximately 5% of the total human body mass, with its main functions being motility, digestion, absorption, excretion, and circulation.
- The layers of the GI tract wall, from outermost to innermost, are the serosa, longitudinal muscle layer, circular muscle layer, submucosa, and mucosa.
- The autonomic nervous system innervates the GI tract, composed of the extrinsic nervous system (with sympathetic and parasympathetic components) and the enteric nervous system.
- The extrinsic sympathetic nervous system is primarily inhibitory, with stimulation decreasing or ceasing GI motility, while the extrinsic parasympathetic nervous system is primarily excitatory, activating GI motility and function.
- The enteric nervous system is the independent nervous system of the GI tract, controlling motility, secretion, and blood flow, with two plexuses: the myenteric (Auerbach) plexus and the submucosal (Meissner) plexus.
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.
Description
Test your knowledge of the structure and functions of the gastrointestinal tract, including its layers and main functions. Learn about the different parts of the GI tract and their roles in digestion, absorption, and excretion. Challenge yourself with this quiz!