Podcast
Questions and Answers
What is the primary characteristic of urge incontinence?
What is the primary characteristic of urge incontinence?
- Urine-associated with desire of micturition (correct)
- Acute retention with agonizing bladder pain
- Desire to void urine
- Obvious neurologic affection
What is the purpose of the methylene blue test?
What is the purpose of the methylene blue test?
- To assess bladder capacity
- To evaluate urinary incontinence
- To detect urinary tract infections
- To diagnose genitourinary fistula (correct)
What is the normal range for the first desire to void urine?
What is the normal range for the first desire to void urine?
- 250-300ml
- 200-250ml
- 150-200ml (correct)
- 100-150ml
What is the characteristic of genuine stress incontinence?
What is the characteristic of genuine stress incontinence?
What is the purpose of urodynamic studies?
What is the purpose of urodynamic studies?
What is the recommended management for menopausal females with genuine stress incontinence?
What is the recommended management for menopausal females with genuine stress incontinence?
What is the purpose of cystometry?
What is the purpose of cystometry?
What is the normal range for bladder capacity?
What is the normal range for bladder capacity?
What is the recommended preventive measure for genuine stress incontinence?
What is the recommended preventive measure for genuine stress incontinence?
What is the purpose of pretibial nerve stimulation?
What is the purpose of pretibial nerve stimulation?
Flashcards are hidden until you start studying
Study Notes
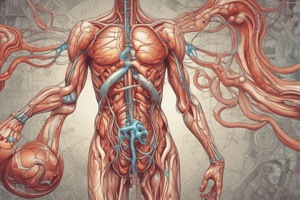
Anatomy of the Bladder
- The bladder is a hollow muscular organ situated behind the pubis symphysis.
- It is composed of a crisscross of smooth muscle fibers known as the Detrusor muscle.
- The Detrusor muscle has a rich cholinergic parasympathetic supply.
- Contraction of the Detrusor muscle results in simultaneous reduction of the bladder in all its diameters.
Anatomy of the Female Urethra
- The urethra is 3-5 cm in length and is a thin-walled muscular tube that drains urine from the bladder to outside the body.
- Beneath the epithelium is a rich vascular plexus that contributes up to 1/3 of the urethral pressure.
- The urethra has a minimal parasympathetic innervation, and its smooth muscles are innervated by sympathetic fibers.
- Stimulation of these sympathetic fibers produces urethral contraction via α-adrenergic receptors.
- β-adrenergic receptors produce Detrusor muscle relaxation.
Urethral Sphincters
- The internal urethral sphincter (involuntary) is a thickening of the Detrusor muscle at the bladder-urethral junction.
- The external urethral sphincter (voluntary) is a skeletal muscle that surrounds the urethra as it passes through the urogenital diaphragm.
- The urogenital diaphragm is part of the pelvic diaphragm, which is the muscular portion of the pelvic floor that provides a stable base on which the bladder neck and proximal urethra rest.
Mechanism of Continence
- The intra-urethral pressure at rest or with the stress of increased intra-abdominal pressure (IAP) remains higher than intra-vesical pressure by:
- Urethral mucosal resistance
- Periurethral vascular plexus pressure
- Resting intra-abdominal pressure
- Kinking of the urethra
- Contraction of the urogenital diaphragm
- Urinary continence is the ability to hold urine at all times except during micturition.
- Continence control is established via:
- Intraurethral pressure higher than intravesical pressure (neuromuscular)
- Fascial support around the urethra (anatomical position)
- Submucosal vascularity
Micturition
- As urine accumulates, the bladder stretches and stretch receptors are activated, causing a reflex that results in relaxation of the Detrusor muscle and contraction of the external urethral sphincter.
- When about 200 ml of urine has accumulated, impulses are sent to the brain and one begins to feel the urge to urinate.
- Activation of the micturition center in the pons signals parasympathetic neurons that stimulate contraction of the Detrusor and relaxation of the sphincters.
- During micturition:
- Relaxation of pelvic striated muscle (pudendal nerve inhibition)
- Relaxation of the fascial support (parasympathetic effect)
- Descent of the bladder neck
- Funnelling of the urethra
- Increase of urethro-vesical angle → 180°
- Increase of urethral pubic angle → 45°
- Contraction of the Detrusor muscle (parasympathetic effect)
Urinary Incontinence
- Urinary incontinence is the involuntary leakage of urine.
- Classification:
- (A) Extra urethral incontinence: Genito-urinary fistula
- (B) Urethral incontinence:
- Genuine stress incontinence (urodynamic incontinence)
- Urge incontinence (detrusor instability)
- Mixed type
- Retention with overflow
- Nocturnal enuresis
Stress Incontinence
- Definition: Involuntary leakage on effort, exertion, sneezing, or coughing.
- Etiology: Intra-abdominal pressure exceeds the muscular strength of the sphincter.
- Impaired urethral support, intrinsic sphincter deficiency, and weakness of the musculo-fascial support of the urethro-vesical junction.
Why is Incontinence Important?
- Social stigmata; leads to restricted activities and depression
- Medical complications: ulcers, increased urinary tract infections
- UI is the second leading cause of nursing home placement
- Only 10-20% seek medical care
- Millions of pounds spent annually on incontinence products
Etiology of Stress Incontinence
- Weakness of the musculo-fascial support of the urethro-vesical junction
- Descent of the urethro-vesical junction so that the upper urethra is not situated above the urogenital diaphragm
- Damage to either the pelvic floor musculature (levator ani) or pubourethral ligaments
Bonney's Test
- The bladder neck is elevated by 2 fingers placed in the vagina on each side of the urethra without compressing it.
- If no urine escapes during coughing, then bladder neck descent is the cause, and surgical repair will be successful.
- If urine escapes on coughing, then weakness of the bladder neck will be the cause.
Urge Incontinence
- Definition: Involuntary leakage associated with a strong urge to pass urine that cannot be held back.
- Etiology: Overlap of detrusor overactivity and impaired urethral sphincter function.
Mixed Incontinence
- Definition: Involuntary leakage associated with urgency as well as exertion, effort, sneezing, or coughing.
- Etiology: Overlap of detrusor overactivity and impaired urethral sphincter function.
Vesicovaginal Fistula
- Congenital or traumatic
- Surgical trauma: The commonest cause, mostly surgical nowadays.
- Obstetric trauma: It occurs in 2 types:
- Necrotic obstetric trauma
- Direct obstetric trauma
- Inflammatory: Non-specific infections, pelvic abscess that opens in the bladder and vagina, specific infections (T.B. or bilharziasis), and neoplastic (e.g., advanced cases of cancer cervix, bladder, or vagina).
Investigations for a Case of Urinary Incontinence
- History and examination:
- Genito-urinary fistula: continuous (day and night) urine dripping
- Genuine stress incontinence: only drops of urine, not associated with the desire of micturition, usually on sudden cough or sneeze
- Urge incontinence: more than drops of urine, associated with the desire of micturition
- Retention with overflow: obvious neurologic affection or agonizing bladder pain with acute retention
- Nocturnal enuresis: only by night, may be psychological disorders
- Specific investigations:
- Cases suspected to be genitor-urinary fistula: Methylene blue test
- Midstream urine to detect infection with pus cells
- Culture and sensitivity may be needed
- Urodynamic studies: Differentiate genuine stress incontinence from urge incontinence and diagnose mixed cases.
Management of Urinary Incontinence
- Genuine stress incontinence:
- Preventive: Avoid obstetric trauma, advise postnatal pelvic exercises, and replace therapy for menopausal females.
- Behavioral therapy: Restrict fluid, lose weight, treat constipation, and stop smoking.
- Repeated pelvic floor exercises (Kegel's exercises or passive by electric stimulation)
- Minimally invasive therapies: Pretibial nerve stimulation (PTN) and surgery.
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.