Podcast
Questions and Answers
What is the primary function of the smooth muscle tone in arterioles?
What is the primary function of the smooth muscle tone in arterioles?
- To contribute to the propagation of blood flow
- To determine systemic vascular resistance (correct)
- To facilitate diffusion of oxygen and carbon dioxide
- To regulate blood pressure
What is the characteristic of the endothelial lining in capillaries?
What is the characteristic of the endothelial lining in capillaries?
- It facilitates rapid diffusion of oxygen and carbon dioxide (correct)
- It has a diameter of 20 to 100 μm
- It has a thick layer of smooth muscle
- It is highly elastic
What is the result of anastomoses between branching networks of smaller arteries when an artery is obstructed?
What is the result of anastomoses between branching networks of smaller arteries when an artery is obstructed?
- Formation of collateral circulation (correct)
- Formation of new capillaries
- Increased blood pressure
- Reduced blood flow to the affected area
What is the diameter of capillaries?
What is the diameter of capillaries?
What type of arteries are the coronary and renal arteries?
What type of arteries are the coronary and renal arteries?
What is the primary function of the elastic recoil in large- and medium-sized arteries?
What is the primary function of the elastic recoil in large- and medium-sized arteries?
What is the function of the vasa vasorum in the media layer of an artery?
What is the function of the vasa vasorum in the media layer of an artery?
What is the initial step in the development of atherosclerosis?
What is the initial step in the development of atherosclerosis?
What is the function of the adventitia in an artery?
What is the function of the adventitia in an artery?
What occurs when atheromatous plaque forms in the coronary arteries?
What occurs when atheromatous plaque forms in the coronary arteries?
What is the role of mononuclear phagocytes in the development of atherosclerosis?
What is the role of mononuclear phagocytes in the development of atherosclerosis?
What is the purpose of the internal elastic membrane?
What is the purpose of the internal elastic membrane?
What is the composition of the media layer of an artery?
What is the composition of the media layer of an artery?
What is the consequence of atheromatous plaque formation in the carotid arteries?
What is the consequence of atheromatous plaque formation in the carotid arteries?
Where is the femoral artery palpable in the legs?
Where is the femoral artery palpable in the legs?
What is the posterior tibial artery protected by?
What is the posterior tibial artery protected by?
What is a potentially life-threatening condition that can result from occlusion of the mesenteric arteries?
What is a potentially life-threatening condition that can result from occlusion of the mesenteric arteries?
Where is the popliteal artery located?
Where is the popliteal artery located?
Where is the dorsalis pedis artery located?
Where is the dorsalis pedis artery located?
Where is the brachial artery located in the arm?
Where is the brachial artery located in the arm?
Which artery is not palpable in the abdomen?
Which artery is not palpable in the abdomen?
What is the primary function of the celiac trunk?
What is the primary function of the celiac trunk?
Which artery perfuses the jejunum and ileum?
Which artery perfuses the jejunum and ileum?
What is the purpose of the two vascular arches in the hand?
What is the purpose of the two vascular arches in the hand?
Which part of the large intestine is perfused by the inferior mesenteric artery?
Which part of the large intestine is perfused by the inferior mesenteric artery?
What percentage of circulating blood flow can veins contain?
What percentage of circulating blood flow can veins contain?
What is the function of the unidirectional valves in peripheral veins?
What is the function of the unidirectional valves in peripheral veins?
Which veins drain into the portal vein?
Which veins drain into the portal vein?
What is the consequence of the weaker wall structure of leg veins?
What is the consequence of the weaker wall structure of leg veins?
What is the role of the hepatic artery in the liver?
What is the role of the hepatic artery in the liver?
Where do veins from the arms, upper trunk, and head drain?
Where do veins from the arms, upper trunk, and head drain?
What percentage of venous return from the lower extremities is carried by the deep veins?
What percentage of venous return from the lower extremities is carried by the deep veins?
Which superficial vein originates on the lateral side of the foot?
Which superficial vein originates on the lateral side of the foot?
What is the function of the one-way valves in the deep, superficial, and perforating veins?
What is the function of the one-way valves in the deep, superficial, and perforating veins?
Which lymphatic duct drains fluid from the right side of the head, neck, thorax, and right upper limb?
Which lymphatic duct drains fluid from the right side of the head, neck, thorax, and right upper limb?
What is the primary function of the lymphatic system?
What is the primary function of the lymphatic system?
Where do the superficial veins receive relatively poor tissue support?
Where do the superficial veins receive relatively poor tissue support?
What is the name of the vein that joins the femoral vein of the deep venous system below the inguinal ligament?
What is the name of the vein that joins the femoral vein of the deep venous system below the inguinal ligament?
What helps to propel blood upward against gravity in the venous system?
What helps to propel blood upward against gravity in the venous system?
Flashcards are hidden until you start studying
Study Notes
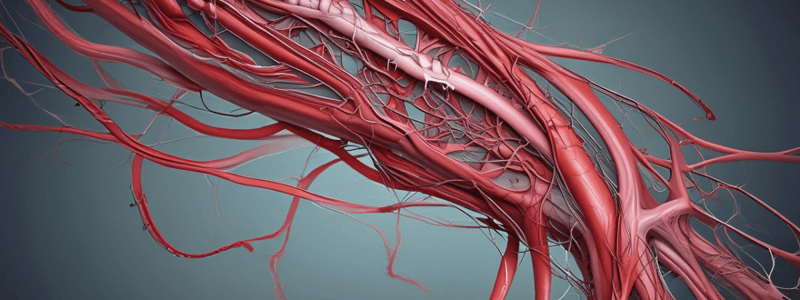
Structure of Arteries
- Arteries consist of three concentric layers of tissue: intima, media, and adventitia.
- Intima is the innermost layer, a single continuous lining of endothelial cells.
- Media is composed of smooth muscle cells with elastic properties.
- Adventitia is the outer layer, containing connective tissue, nerve fibers, and vasa vasorum.
Atherosclerosis
- Atherosclerosis is a chronic inflammatory disease initiated by injury to vascular endothelial cells.
- Injury leads to atheromatous plaque formation, triggered by circulating cholesterol particles (LDLs) and proteoglycans from the extracellular matrix.
- LDLs undergo oxidative modification, leading to a local inflammatory response and attracting mononuclear phagocytes.
- Phagocytes mature into macrophages, ingest lipids, and become foam cells that develop into fatty streaks.
Effects of Atherosclerosis
- Thrombi in coronary arteries can result in acute myocardial infarction.
- Thrombi in carotid arteries can dislodge and travel to the brain, resulting in stroke.
Arterial Branching
- Arteries vary in size and anatomy according to their distance from the heart.
- Large, highly elastic arteries (e.g., aorta, common carotid, and iliac arteries) course into medium-sized muscular arteries (e.g., coronary and renal arteries).
- Medium-sized arteries divide into small arteries (<2 mm in diameter) and arterioles (20-100 μm in diameter).
- Arterioles are responsible for systemic vascular resistance, a major component of blood pressure.
Capillaries
- Capillaries are the smallest blood vessels, with a diameter of a single red blood cell (7-8 μm).
- Capillaries have an endothelial cell lining, but no media, facilitating rapid diffusion of oxygen and carbon dioxide.
- Anastomoses between branching networks of smaller arteries can increase in size to form collateral circulation, perfusing structures distal to an occlusion.
Arterial Pulses
- Arterial pulses are palpable in arteries close to the body surface.
Pulses in the Arms and Hands
- Locate pulsations in the brachial artery at the bend of the elbow just medial to the biceps tendon.
- Find pulsations in the radial artery on the lateral flexor surface.
- Identify pulsations in the ulnar artery on the medial flexor surface (although overlying tissues may obscure pulsations).
- Two vascular arches within the hand interconnect the radial and ulnar arteries, protecting circulation to the hand and fingers from arterial occlusion.
Pulses in the Abdomen
- Locate pulsations of the aorta in the epigastrium.
- Celiac trunk supplies blood to the esophagus, stomach, proximal duodenum, liver, gallbladder, pancreas, and spleen (foregut).
- Superior mesenteric artery supplies blood to the small intestine (jejunum, ileum, cecum), large intestine (ascending and transverse colon, right splenic flexure) (midgut).
- Inferior mesenteric artery supplies blood to the large intestine (descending and sigmoid colon, proximal rectum) (hindgut).
Pulses in the Legs
- Palpate pulsations in the femoral artery just below the inguinal ligament, midway between the anterior superior iliac spine and the symphysis pubis.
- Find pulsations in the popliteal artery, an extension of the femoral artery that passes medially behind the femur, palpable just behind and deep in the knee.
- Identify pulsations in the posterior tibial (PT) artery, which lies behind the medial malleolus of the ankle.
- Locate pulsations in the dorsalis pedis (DP) artery on the dorsum of the foot just lateral to the extensor tendon of the big toe.
Importance of Arterial Pulses
- Despite a rich collateral network, occlusion of the mesenteric arteries can result in acute mesenteric ischemia, a potentially life-threatening condition.
Characteristics of Veins
- Thin-walled and highly distensible, allowing them to contain up to two-thirds of circulating blood flow
- Nonthrombogenic endothelium in the venous intima
- Unidirectional valves in peripheral veins promote venous return to the heart
- Media contains circumferential rings of elastic tissue and smooth muscle that change vein caliber in response to minor changes in venous pressure
Venous Return
- Veins from the arms, upper trunk, and head and neck drain into the superior vena cava
- Veins from the abdominal wall, liver, lower trunk, and legs drain into the inferior vena cava
- Veins from the abdominal viscera drain into the portal vein, which supplies ~75% of blood flow to the liver
- Blood from the portal vein flows into the hepatic sinusoids, then drains into the hepatic veins that empty into the inferior vena cava
Leg Veins
- Susceptible to irregular dilatation, compression, ulceration, and invasion by tumors due to weaker wall structure
- Require special attention due to their vulnerability
Venous System
- Deep veins of the legs carry approximately 90% of the venous return from the lower extremities and are well supported by surrounding tissues.
- Superficial veins are subcutaneous and have relatively poor tissue support.
- The great saphenous vein originates on the dorsum of the foot, passes anterior to the medial malleolus, and joins the femoral vein below the inguinal ligament.
- The small saphenous vein begins on the lateral side of the foot, passes upward along the posterior calf, and joins the deep venous system in the popliteal fossa.
Blood Flow and Valves
- Competent one-way valves in the deep, superficial, and perforating veins propel blood toward the heart, preventing pooling, venous stasis, and backward flow.
- Contraction of the calf muscles during walking serves as a venous pump, propelling blood upward against gravity.
Lymphatic System
- The lymphatic system is an extensive vascular network that drains lymph fluid from body tissues and returns it to the venous circulation.
- Lymphatic capillaries originate in extracellular spaces, collecting tissue fluid, plasma proteins, cells, and cellular debris via their porous endothelium.
- The right lymphatic duct drains fluid from the right side of the head, neck, thorax, and right upper limb, emptying into the junction of the right internal jugular and subclavian veins.
- The thoracic duct collects lymph fluid from the rest of the body, emptying into the junction of the left internal jugular and subclavian veins.
- Lymph fluid is filtered through lymph nodes interposed along the way.
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.