Podcast
Questions and Answers
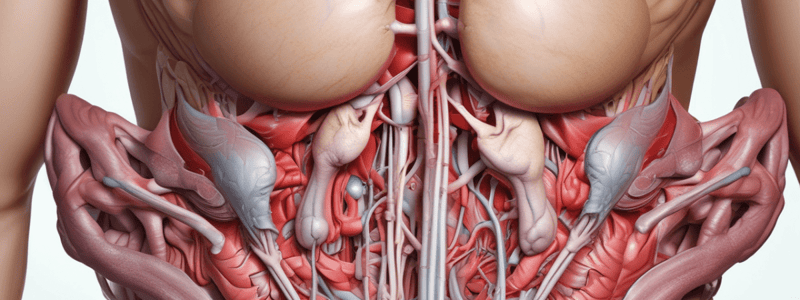
What is the location of the spermatic cord or round ligament of the uterus?
What is the location of the spermatic cord or round ligament of the uterus?
- Inguinal ring (correct)
- Pectineal line
- Pubic tubercle
- Iliac crest
What is the function of the internal oblique muscle?
What is the function of the internal oblique muscle?
- To attach to the iliac crest
- To form the inguinal ligament
- To radiate upward and forward (correct)
- To support the spermatic cord
What is the shape of the defect in the external oblique aponeurosis?
What is the shape of the defect in the external oblique aponeurosis?
- Triangular (correct)
- Circular
- Oval
- Rectangular
Where does the lowest part of the internal oblique muscle attach?
Where does the lowest part of the internal oblique muscle attach?
What is the function of the lacunar ligament?
What is the function of the lacunar ligament?
What is the purpose of the inguinal ligament?
What is the purpose of the inguinal ligament?
What is the relationship between the internal oblique muscle and the transversus abdominis?
What is the relationship between the internal oblique muscle and the transversus abdominis?
What is the location of the posterior free border of the internal oblique muscle?
What is the location of the posterior free border of the internal oblique muscle?
Which structure lies between the external oblique aponeurosis and the internal oblique aponeurosis?
Which structure lies between the external oblique aponeurosis and the internal oblique aponeurosis?
What is the name of the structure formed by the aponeuroses of the abdominal muscles?
What is the name of the structure formed by the aponeuroses of the abdominal muscles?
Which muscle is not involved in the formation of the rectus sheath?
Which muscle is not involved in the formation of the rectus sheath?
What is the name of the structure that connects the rectus abdominis muscle to the pubis?
What is the name of the structure that connects the rectus abdominis muscle to the pubis?
Which layer of the rectus sheath is in contact with the rectus abdominis muscle?
Which layer of the rectus sheath is in contact with the rectus abdominis muscle?
What is the name of the layer of fascia that lies deep to the rectus abdominis muscle?
What is the name of the layer of fascia that lies deep to the rectus abdominis muscle?
Which structure passes through the spermatic cord?
Which structure passes through the spermatic cord?
What is the name of the structure that forms the anterior wall of the rectus sheath?
What is the name of the structure that forms the anterior wall of the rectus sheath?
What is the likely consequence of a rupture of the penile urethra?
What is the likely consequence of a rupture of the penile urethra?
What is the purpose of a surgeon's continuous suture in closing abdominal wounds?
What is the purpose of a surgeon's continuous suture in closing abdominal wounds?
What is the function of the aponeuroses of the three sheets in the rectus abdominis muscle?
What is the function of the aponeuroses of the three sheets in the rectus abdominis muscle?
What is the small muscle that may be present in the lower part of the rectus sheath?
What is the small muscle that may be present in the lower part of the rectus sheath?
What is the anatomical landmark that marks the edge of the arcuate line?
What is the anatomical landmark that marks the edge of the arcuate line?
What is the purpose of the rectus abdominis muscle?
What is the purpose of the rectus abdominis muscle?
What is the relationship between the fascia and the thigh in a rupture of the penile urethra?
What is the relationship between the fascia and the thigh in a rupture of the penile urethra?
What is the function of the anterior abdominal wall muscles?
What is the function of the anterior abdominal wall muscles?
What is the term for the condition where the lower part of the anterior abdominal wall protrudes forward?
What is the term for the condition where the lower part of the anterior abdominal wall protrudes forward?
What is the term for the layer of fat that can accumulate in the superficial fascia?
What is the term for the layer of fat that can accumulate in the superficial fascia?
What is the term for the group of muscles that include the external and internal obliques?
What is the term for the group of muscles that include the external and internal obliques?
What is the location of the dermatome of T7?
What is the location of the dermatome of T7?
What fascia is deep to the muscles?
What fascia is deep to the muscles?
What is the skin loosely attached to, except at the umbilicus?
What is the skin loosely attached to, except at the umbilicus?
What are the natural lines of cleavage in the skin?
What are the natural lines of cleavage in the skin?
What is the umbilicus?
What is the umbilicus?
Which arteries supply the skin near the midline?
Which arteries supply the skin near the midline?
What is the cutaneous nerve supply to the anterolateral abdominal wall derived from?
What is the cutaneous nerve supply to the anterolateral abdominal wall derived from?
Where does venous drainage from the upper abdominal wall mainly pass into?
Where does venous drainage from the upper abdominal wall mainly pass into?
What is the function of the vas deferens?
What is the function of the vas deferens?
Which structure is located in the posterior aspect of the spermatic cord?
Which structure is located in the posterior aspect of the spermatic cord?
What is the origin of the testicular artery?
What is the origin of the testicular artery?
What is the function of the testicular veins?
What is the function of the testicular veins?
What forms the superficial inguinal ring?
What forms the superficial inguinal ring?
What is the name of the plexus formed by the testicular veins?
What is the name of the plexus formed by the testicular veins?
Which nerve is responsible for the autonomic innervation of the testes?
Which nerve is responsible for the autonomic innervation of the testes?
What is the function of testosterone in fetal development?
What is the function of testosterone in fetal development?
What is the name of the muscle formed from the lowest fibers of the internal oblique muscle?
What is the name of the muscle formed from the lowest fibers of the internal oblique muscle?
What is the function of the remains of the processus vaginalis?
What is the function of the remains of the processus vaginalis?
What structure passes through the layers of the lower part of the anterior abdominal wall?
What structure passes through the layers of the lower part of the anterior abdominal wall?
What is the location of the vas deferens in the scrotum?
What is the location of the vas deferens in the scrotum?
What is the name of the structure that forms the third tubular covering of the testis?
What is the name of the structure that forms the third tubular covering of the testis?
During what months of fetal life does the testis descend through the pelvis and inguinal canal?
During what months of fetal life does the testis descend through the pelvis and inguinal canal?
What is the name of the band of mesenchyme that extends from the developing gonad to the labioscrotal swelling?
What is the name of the band of mesenchyme that extends from the developing gonad to the labioscrotal swelling?
What is the name of the diverticulum that forms before the descent of the testis and ovary from their site of origin?
What is the name of the diverticulum that forms before the descent of the testis and ovary from their site of origin?
What is the purpose of the pampiniform plexus?
What is the purpose of the pampiniform plexus?
Where do the afferent sensory nerves that accompany the testicular artery originate from?
Where do the afferent sensory nerves that accompany the testicular artery originate from?
What is the fate of the processus vaginalis in both sexes?
What is the fate of the processus vaginalis in both sexes?
Where does the testicular vein drain into on the left side?
Where does the testicular vein drain into on the left side?
What is the course of the autonomic nerves that supply the testis?
What is the course of the autonomic nerves that supply the testis?
What is the purpose of the genitofemoral nerve?
What is the purpose of the genitofemoral nerve?
What is the destination of the testicular vein on the right side?
What is the destination of the testicular vein on the right side?
What is the primary function of the nerve that supplies the cremaster muscle?
What is the primary function of the nerve that supplies the cremaster muscle?
What is the fate of the round ligament of the uterus?
What is the fate of the round ligament of the uterus?
Through which canal do the testicular lymph vessels ascend?
Through which canal do the testicular lymph vessels ascend?
Where do the testicular lymph vessels ultimately drain?
Where do the testicular lymph vessels ultimately drain?
What is the level of the first lumbar vertebra in relation to the testicular lymph vessels?
What is the level of the first lumbar vertebra in relation to the testicular lymph vessels?
What is the relationship between the spermatic cord and the testis?
What is the relationship between the spermatic cord and the testis?
How many layers of fascia cover the spermatic cord?
How many layers of fascia cover the spermatic cord?
What is the name of the artery that supplies the testis?
What is the name of the artery that supplies the testis?
What is the name of the nerve that accompanies the testicular artery?
What is the name of the nerve that accompanies the testicular artery?
During which process does the covering of the spermatic cord acquire its layers?
During which process does the covering of the spermatic cord acquire its layers?
What is the significance of the presence of spermatozoa in the first few postoperative ejaculations after vasectomy?
What is the significance of the presence of spermatozoa in the first few postoperative ejaculations after vasectomy?
Which structure is attached to the margins of the deep inguinal ring?
Which structure is attached to the margins of the deep inguinal ring?
What is the purpose of ligating the vas deferens during vasectomy?
What is the purpose of ligating the vas deferens during vasectomy?
What is the composition of the seminal fluid after vasectomy?
What is the composition of the seminal fluid after vasectomy?
What is the location of the incision made during vasectomy?
What is the location of the incision made during vasectomy?
What is the origin of the external spermatic fascia?
What is the origin of the external spermatic fascia?
What is the attachment of the cremasteric fascia?
What is the attachment of the cremasteric fascia?
What is the term for the layer of muscle that fuses to form large sheets?
What is the term for the layer of muscle that fuses to form large sheets?
What is the significance of the tendinous intersections in the rectus abdominis?
What is the significance of the tendinous intersections in the rectus abdominis?
What is the embryonic structure that gives rise to the abdominal wall and peritoneal cavity?
What is the embryonic structure that gives rise to the abdominal wall and peritoneal cavity?
What is the fate of the segmental arrangement in the thorax?
What is the fate of the segmental arrangement in the thorax?
What is the term for the layer of mesoderm associated with ectoderm?
What is the term for the layer of mesoderm associated with ectoderm?
What is the term for the layer of mesoderm associated with entoderm?
What is the term for the layer of mesoderm associated with entoderm?
What is the structure that forms the boundary between the abdominal wall and the peritoneal cavity?
What is the structure that forms the boundary between the abdominal wall and the peritoneal cavity?
What is the term for the cavity that forms from the extra-embryonic coelom?
What is the term for the cavity that forms from the extra-embryonic coelom?
What is the result of the lateral folds of the embryo fusing in the midline?
What is the result of the lateral folds of the embryo fusing in the midline?
What is the direction of the fibers of the psoas muscle?
What is the direction of the fibers of the psoas muscle?
What is the function of the umbilical arteries?
What is the function of the umbilical arteries?
What is the structure that covers the anterior surface of the psoas muscle?
What is the structure that covers the anterior surface of the psoas muscle?
What is the result of the ventral mesentery breaking down?
What is the result of the ventral mesentery breaking down?
What is the location of the swelling in a psoas abscess?
What is the location of the swelling in a psoas abscess?
What is the function of Wharton's Jelly?
What is the function of Wharton's Jelly?
What is the result of the anterior body wall closing in the midline?
What is the result of the anterior body wall closing in the midline?
What is the term for the swelling that occurs in the right groin above and below the right inguinal ligament?
What is the term for the swelling that occurs in the right groin above and below the right inguinal ligament?
What is the purpose of the yolk sac?
What is the purpose of the yolk sac?
What is the result of the mesenchymal core of the cord forming?
What is the result of the mesenchymal core of the cord forming?
What is the muscle that forms the posterior abdominal wall?
What is the muscle that forms the posterior abdominal wall?
What is the structure that is thickened above to form the lateral arcuate ligament?
What is the structure that is thickened above to form the lateral arcuate ligament?
What is the function of the umbilical veins?
What is the function of the umbilical veins?
What is the condition that results in the swelling of the upper part of the thigh below the inguinal ligament?
What is the condition that results in the swelling of the upper part of the thigh below the inguinal ligament?
What is the origin of the iliacus muscle?
What is the origin of the iliacus muscle?
What is the function of the quadratus lumborum muscle?
What is the function of the quadratus lumborum muscle?
What is the innervation of the abdominal wall muscles?
What is the innervation of the abdominal wall muscles?
What is the combined muscle formed by the iliacus and psoas major muscles?
What is the combined muscle formed by the iliacus and psoas major muscles?
What is the function of the iliopsoas muscle?
What is the function of the iliopsoas muscle?
What is the origin of the psoas major muscle?
What is the origin of the psoas major muscle?
What forms the posterior abdominal wall?
What forms the posterior abdominal wall?
What is the nerve supply of the iliacus muscle?
What is the nerve supply of the iliacus muscle?
What is the embryological origin of the abdominal wall muscles?
What is the embryological origin of the abdominal wall muscles?
What is the approximate length of the umbilical cord at the end of pregnancy?
What is the approximate length of the umbilical cord at the end of pregnancy?
What is the result of the amnion and chorion fusing?
What is the result of the amnion and chorion fusing?
What is the purpose of the ligature applied to the umbilical cord after birth?
What is the purpose of the ligature applied to the umbilical cord after birth?
What may be present as an umbilical hernia in the remains of the extraembryonic coelom?
What may be present as an umbilical hernia in the remains of the extraembryonic coelom?
What is the result of a congenital urethral obstruction in newborns?
What is the result of a congenital urethral obstruction in newborns?
What is the significance of the expansion of the amniotic cavity?
What is the significance of the expansion of the amniotic cavity?
What is the fate of the umbilical vessels after the application of the ligature?
What is the fate of the umbilical vessels after the application of the ligature?
What is the location of the allantois in relation to the umbilical cord?
What is the location of the allantois in relation to the umbilical cord?
What is the order of anatomic structures penetrated to reach the parietal peritoneum?
What is the order of anatomic structures penetrated to reach the parietal peritoneum?
What is the purpose of peritoneal lavage?
What is the purpose of peritoneal lavage?
What structure is located between the skin and the fatty layer?
What structure is located between the skin and the fatty layer?
What is the name of the artery located inferior to the fatty layer?
What is the name of the artery located inferior to the fatty layer?
What is the purpose of the catheter in peritoneal lavage?
What is the purpose of the catheter in peritoneal lavage?
What is the name of the layer that is penetrated first during peritoneal lavage?
What is the name of the layer that is penetrated first during peritoneal lavage?
What is the primary disadvantage of the incision described in the text?
What is the primary disadvantage of the incision described in the text?
What structure is pushed away by the cannula during paracentesis?
What structure is pushed away by the cannula during paracentesis?
What is the primary advantage of endoscopic surgery on the gallbladder, bile ducts, and appendix?
What is the primary advantage of endoscopic surgery on the gallbladder, bile ducts, and appendix?
What is the usual entry point of the cannula during paracentesis?
What is the usual entry point of the cannula during paracentesis?
Which anatomical structure is traversed during endoscopic surgery on the gallbladder, bile ducts, and appendix?
Which anatomical structure is traversed during endoscopic surgery on the gallbladder, bile ducts, and appendix?
What is the purpose of paracentesis?
What is the purpose of paracentesis?
What is the primary concern during endoscopic surgery on the gallbladder, bile ducts, and appendix?
What is the primary concern during endoscopic surgery on the gallbladder, bile ducts, and appendix?
What is the likely consequence of damaging multiple segmental nerves during an incision?
What is the likely consequence of damaging multiple segmental nerves during an incision?
What is the potential consequence of bleeding into the peritoneal cavity during surgery?
What is the potential consequence of bleeding into the peritoneal cavity during surgery?
Which structure is not damaged during paracentesis?
Which structure is not damaged during paracentesis?
What is the significance of securing superficial fascia during surgery?
What is the significance of securing superficial fascia during surgery?
Which blood vessels are encountered during endoscopic surgery on the gallbladder, bile ducts, and appendix?
Which blood vessels are encountered during endoscopic surgery on the gallbladder, bile ducts, and appendix?
What is the usual location of the incision mentioned in the text?
What is the usual location of the incision mentioned in the text?
What is the purpose of the cannula sheath during paracentesis?
What is the purpose of the cannula sheath during paracentesis?
What is the benefit of minimal disruption to the anatomic features of the anterior abdominal wall during endoscopic surgery?
What is the benefit of minimal disruption to the anatomic features of the anterior abdominal wall during endoscopic surgery?
What is the primary layer of fascia encountered during endoscopic surgery on the gallbladder, bile ducts, and appendix?
What is the primary layer of fascia encountered during endoscopic surgery on the gallbladder, bile ducts, and appendix?
What is the main disadvantage of the McBurney's incision?
What is the main disadvantage of the McBurney's incision?
What is the purpose of incising the transversalis fascia and the peritoneum?
What is the purpose of incising the transversalis fascia and the peritoneum?
Why is an infraumbilical right paramedian incision used instead of the McBurney's incision?
Why is an infraumbilical right paramedian incision used instead of the McBurney's incision?
What is the significance of the anatomic structures penetrated during peritoneal lavage?
What is the significance of the anatomic structures penetrated during peritoneal lavage?
What is the result of dividing one or more segmental nerves to the rectus abdominis muscle?
What is the result of dividing one or more segmental nerves to the rectus abdominis muscle?
What is the location of the inferior epigastric artery?
What is the location of the inferior epigastric artery?
What is the purpose of the peritoneal lavage procedure?
What is the purpose of the peritoneal lavage procedure?
What is the advantage of using the paramedian incision?
What is the advantage of using the paramedian incision?
What is the purpose of retracting the rectus muscle medially?
What is the purpose of retracting the rectus muscle medially?
What is the layer of fascia that lies deep to the rectus abdominis muscle?
What is the layer of fascia that lies deep to the rectus abdominis muscle?
What is the consequence of not suturing the cut ends of the rectus muscles?
What is the consequence of not suturing the cut ends of the rectus muscles?
What is the consequence of perforating the gut during peritoneal lavage?
What is the consequence of perforating the gut during peritoneal lavage?
What is the significance of the lines alba in peritoneal lavage?
What is the significance of the lines alba in peritoneal lavage?
What is the purpose of incising the posterior wall of the rectus sheath?
What is the purpose of incising the posterior wall of the rectus sheath?
What is the purpose of the paraumbilical incision technique?
What is the purpose of the paraumbilical incision technique?
What is the consequence of bleeding from the epigastric vessels during peritoneal lavage?
What is the consequence of bleeding from the epigastric vessels during peritoneal lavage?
What is the likely route of infection spread from the peritoneum to the pleura?
What is the likely route of infection spread from the peritoneum to the pleura?
Why is it common to find local pus in a pleural space in a patient with a subphrenic abscess?
Why is it common to find local pus in a pleural space in a patient with a subphrenic abscess?
What is the purpose of sitting a patient up in bed at an angle of 45 degrees?
What is the purpose of sitting a patient up in bed at an angle of 45 degrees?
What is the role of the greater omentum in surgery?
What is the role of the greater omentum in surgery?
What is the term for the twisting of the greater omentum?
What is the term for the twisting of the greater omentum?
What is the ligament that connects the stomach to the hilum of the spleen?
What is the ligament that connects the stomach to the hilum of the spleen?
Which structure lies inferior to the liver?
Which structure lies inferior to the liver?
What nerves supply the parietal peritoneum lining the anterior abdominal wall?
What nerves supply the parietal peritoneum lining the anterior abdominal wall?
What is the name of the pocket-like pouches of peritoneum close to the duodenojejunal junction?
What is the name of the pocket-like pouches of peritoneum close to the duodenojejunal junction?
Why does a patient with a subphrenic abscess often complain of pain over the shoulder?
Why does a patient with a subphrenic abscess often complain of pain over the shoulder?
What is the term for the lower six thoracic nerves and the first lumbar nerve?
What is the term for the lower six thoracic nerves and the first lumbar nerve?
What lies anteriorly to the right lobe of the liver?
What lies anteriorly to the right lobe of the liver?
What is the name of the ligament that connects the liver to the anterior abdominal wall?
What is the name of the ligament that connects the liver to the anterior abdominal wall?
What lies superiorly to the liver?
What lies superiorly to the liver?
What is the name of the folds of peritoneum close to the cecum?
What is the name of the folds of peritoneum close to the cecum?
What is the name of the peritoneal reflection that connects the liver to the anterior abdominal wall?
What is the name of the peritoneal reflection that connects the liver to the anterior abdominal wall?
What is the location of the cecum in the abdominal cavity?
What is the location of the cecum in the abdominal cavity?
Which part of the large intestine is located at the periphery of the abdominal cavity?
Which part of the large intestine is located at the periphery of the abdominal cavity?
What is the relationship between the large intestine and the small intestine in the abdominal cavity?
What is the relationship between the large intestine and the small intestine in the abdominal cavity?
What is the function of the peritoneal fluid?
What is the function of the peritoneal fluid?
What is the location of the pancreas in the abdominal cavity?
What is the location of the pancreas in the abdominal cavity?
What is the shape of the appendix?
What is the shape of the appendix?
What is the effect of infection on the peritoneal coverings of the intestine?
What is the effect of infection on the peritoneal coverings of the intestine?
What is the characteristic of the peritoneal fluid?
What is the characteristic of the peritoneal fluid?
What is the direction of the large intestine as it leaves the pelvis?
What is the direction of the large intestine as it leaves the pelvis?
What is the continuity of the large intestine as it leaves the pelvis?
What is the continuity of the large intestine as it leaves the pelvis?
What is the location of the inferior mesenteric vein?
What is the location of the inferior mesenteric vein?
What is the position of the coils of the small intestine in the abdominal cavity?
What is the position of the coils of the small intestine in the abdominal cavity?
What is the purpose of the peritoneal recesses?
What is the purpose of the peritoneal recesses?
What is the effect of the movements of the diaphragm and abdominal muscles on the peritoneal fluid?
What is the effect of the movements of the diaphragm and abdominal muscles on the peritoneal fluid?
What is the name of the structure that forms the paraduodenal recess?
What is the name of the structure that forms the paraduodenal recess?
What is the location of the sigmoid mesocolon?
What is the location of the sigmoid mesocolon?
What is the purpose of the peritoneal ligaments, omenta, and mesenteries?
What is the purpose of the peritoneal ligaments, omenta, and mesenteries?
What is the location of the lesser sac?
What is the location of the lesser sac?
What are the mesenteries?
What are the mesenteries?
What is the function of the mesentery of the small intestine?
What is the function of the mesentery of the small intestine?
What is the relationship between the lesser omentum and the lesser sac?
What is the relationship between the lesser omentum and the lesser sac?
What is the significance of studying the transverse and sagittal sections of the abdomen?
What is the significance of studying the transverse and sagittal sections of the abdomen?
What is the location of the ligamentum teres?
What is the location of the ligamentum teres?
What is the relationship between the right lobe and the left lobe of the liver?
What is the relationship between the right lobe and the left lobe of the liver?
Study Notes
Abdominal Wall
- The linea alba is a tendinous raphe that runs down the midline of the abdominal wall
- The external oblique aponeurosis forms the anterior wall of the rectus sheath
- The internal oblique muscle is a broad, thin, muscular sheet that lies deep to the external oblique
- The internal oblique has a lower free border that arches over the spermatic cord (or round ligament of the uterus)
Rectus Sheath
- The rectus sheath is formed by the aponeuroses of the three flat muscles (external oblique, internal oblique, and transversus abdominis)
- The rectus abdominis muscle is enclosed by the rectus sheath
- The lower part of the rectus sheath may contain a small muscle called the pyramidalis
Inguinal Region
- The inguinal ligament is formed by the fibrous fold of the external oblique aponeurosis
- The spermatic cord (or round ligament of the uterus) passes through the superficial inguinal ring and attaches to the pubic crest and pectineal line
- The conjoint tendon is formed by the tendinous fibers of the internal oblique and transversus abdominis muscles
Fascia and Ligaments
- The fascia transversalis is the deep fascia of the thigh
- The iliac fascia is attached to the inferior rounded border of the inguinal ligament
- The pectineal ligament extends from the pubic tubercle to the pectineal line
Muscles
- The rectus abdominis muscle is a paired muscle that forms a wide vertical strap on either side of the midline
- The transversus abdominis muscle is the deepest of the flat muscles
- The internal oblique muscle is a broad, thin, muscular sheet that lies deep to the external oblique
Nerve Supply
- The dermatome of T7 is located in the epigastrium over the xiphoid process
- The dermatome of T10 includes the umbilicus and that of L1 lies just above the inguinal ligament and the symphysis pubis
- The cutaneous nerve supply to the anterolateral abdominal wall is derived from the anterior rami of the lower six thoracic and the first lumbar nerves
Blood Supply
- Branches of the superior and inferior epigastric arteries supply the skin near the midline
- Branches of the intercostal, lumbar, and deep circumflex iliac arteries supply the skin of the flanks
- The superficial epigastric, superficial circumflex iliac, and superficial external pudendal arteries supply the skin in the inguinal region
Structures of the Spermatlc Cord
- The spermatlc cord consists of the vas deferens, testicular artery, testicular veins (pamplnlform plexus), testicular lymph vessels, autonomic nerves, remains of the processus vaginalis, and genital branch of the genitofemoral nerve.
Vas Deferens
- The vas deferens is a cordlike structure located in the posterior aspect of the spermatlc cord.
- It is a thick-walled muscular duct that transports spermatozoa from the epididymis to the urethra.
- It can be palpated between the finger and thumb in the upper part of the scrotum.
Testicular Artery
- The testicular artery is a branch of the abdominal aorta (at the level of the second lumbar vertebra).
- It is a long and slender artery that descends on the posterior abdominal wall.
- It traverses the inguinal canal and supplies the testis and the epididymis.
Testicular Veins
- The testicular veins form a plexus that leaves the posterior border of the testis.
- The plexus ascends and becomes reduced in size, forming a single testicular vein at about the level of the deep inguinal ring.
- The testicular vein drains into the left renal vein on the left side and into the inferior vena cava on the right side.
Autonomic Nerves
- The autonomic nerves supply the testis and the epididymis.
- Sympathetic fibers run with the testicular artery from the renal or aortic sympathetic plexuses.
- Afferent sensory nerves accompany the efferent sympathetic fibers.
Testicular Lymph Vessels
- The testicular lymph vessels ascend through the inguinal canal and pass up over the posterior abdominal wall.
- They reach the lumbar (para-aortic) lymph nodes on the side of the aorta at the level of the first lumbar vertebra.
Genital Branch of the Genitofemoral Nerve
- The genital branch of the genitofemoral nerve supplies the cremaster muscle.
- It is responsible for the elevation of the testis.
Spermatlc Cord Coverings
- The coverings of the spermatic cord are three concentric layers of fascia derived from the layers of the anterior abdominal wall.
- The external spermatic fascia is derived from the external oblique aponeurosis.
- The cremasteric fascia is derived from the internal oblique muscle.
- The internal spermatic fascia is derived from the transversalis fascia.
Inguinal Canal Development
- The inguinal canal is formed from the processus vaginalis, a peritoneal diverticulum that passes through the layers of the lower part of the anterior abdominal wall.
- The processus vaginalis acquires a tubular covering from each layer as it passes through the layers of the anterior abdominal wall.
- The testicular artery, testicular veins, and testicular lymph vessels traverse the inguinal canal.
Embryology Notes
- The processus vaginalis forms before the descent of the testis and the ovary from their site of origin high on the posterior abdominal wall.
- The testis descends through the pelvis and inguinal canal during the 7th and 8th months of fetal life.
- The normal stimulus for the descent of the testis is testosterone, which is secreted by the fetal testes.
Posterior Abdominal Wall Muscles
- Psoas major muscle: runs downward following the course of the psoas muscle, appears as a swelling in the upper part of the thigh below the inguinal ligament
- Insertion: lower border of the 12th rib and the transverse processes of the upper four lumbar vertebrae
- Anterior surface: covered by lumbar fascia, thickened above to form the lateral arcuate ligament and below to form the lumbar ligament
Transversus Abdominis Muscle
- Fully described with the muscles of the anterolateral abdominal wall
- Psoas abscess present, with swellings in the right groin above and below the right inguinal ligament
Iliacus Muscle
- Fan-shaped, arises from the upper part of the iliac fossa
- Fibers join the lateral side of the psoas major tendon, and the combined muscles are referred to as the iliopsoas
- Iliopsoas is the major flexor of the thigh, or the major flexor of the trunk against the thigh
Posterior Abdominal Wall
- Quadratus lumborum muscle: fixes the 12th rib during inspiration and depresses the 12th rib during forced expiration, laterally flexes the vertebral column of the same side
Embryology Notes
- Abdominal wall development: lateral plate mesoderm splits into a somatopleuric and splanchnic layer associated with ectoderm and entoderm, respectively
- Muscles of the anterior abdominal wall are derived from the somatopleuric mesoderm
- Rectus abdominis retains indications of its segmental origin, as seen by the presence of tendinous intersections
Umbilical Cord and Umbilicus Development
- The umbilical cord is a twisted, tortuous structure that measures about 0.75 in (2 cm) in diameter
- It increases in length until, at the end of pregnancy, it is about 20 in (50 cm) long, the same length as the child
- The umbilical cord contains two arteries that carry deoxygenated blood from the fetus to the chorion (later the placenta) and two veins that convey oxygenated blood from the placenta to the fetus
Clinical Notes
- At birth, the cord is tied off close to the umbilicus, leaving about 2 in (5 cm) of cord between the umbilicus and the ligature
- Occasionally, the cavity of the allantois persists, and urine passes from the bladder through the umbilicus onto the body surface
Abdominal Incisions
- Anatomic structures penetrated to reach the parietal peritoneum: skin, fatty layer, superficial fascia, deep fascia, linea alba, transversalis fascia, extraperitoneal fat, and parietal peritoneum.
- Types of incisions:
- Paramedian incision: medial and parallel to the lateral margin of the rectus muscle, exposing the segmental nerves entering its posterior surface.
- Muscle-splitting incision (McBurney's incision): used for cecostomy and appendectomy, gives limited exposure, and may require an infraumbilical right paramedian incision if diagnosis is unclear.
- Transverse incision: can be made above or below the umbilicus, small or large, and extends from flank to flank.
- Complications:
- Damage to segmental nerves, resulting in postoperative rectus muscle weakness.
- Perforation of the gut, mesenteric blood vessels, or vessels on the posterior abdominal wall or pelvic walls.
- Bleeding from the epigastric vessels, producing a false-positive result.
- Perforation of a full bladder.
- Wound infection.
Peritoneal Lavage
- Anatomic structures penetrated to reach the parietal peritoneum: skin, superficial fascia, deep fascia, linea alba, transversalis fascia, extraperitoneal fat, and parietal peritoneum.
- Common sites used: midline and laterally.
- Important to secure small blood vessels in the superficial fascia to prevent bleeding into the peritoneal cavity, which may produce a false-positive result.
Endoscopic Surgery
- Anatomic structures traversed by instruments: similar to those enumerated for peritoneal lavage.
- Important to preserve the integrity of segmental nerves as they course down from the costal margin to supply the abdominal musculature.
- Advantages: minimal disruption of anatomic and physiologic features of the anterior abdominal wall, and brief convalescence.
Subphrenic Abscess and Hernial Plug
- Infection can spread from the peritoneum to the pleura via the diaphragmatic lymph vessels.
- A patient with a subphrenic abscess may complain of pain over the shoulder, which is also true for collections of blood under the peritoneum.
- The skin of the shoulder is supplied by the supraclavicular nerves (C3 and 4), which have the same segmental origin as the phrenic nerve, which supplies the peritoneum.
Greater Omentum
- The greater omentum is referred to as the "abdominal policeman" by surgeons.
- It can plug the neck of a hernial sac and prevent the entrance of coils of small intestine.
- The greater omentum can be used to buttress an intestinal anastomosis or in the closure of a perforated gastric or duodenal ulcer.
- It can undergo torsion, which may cause necrosis if the blood supply is cut off.
Peritoneal Space and Intestines
- The peritoneum is a space between the parietal peritoneum (lining the abdominal wall) and the visceral peritoneum (covering the abdominal organs).
- The lower six thoracic nerves and the first lumbar nerve supply the parietal peritoneum lining the anterior abdominal wall.
- The large intestine arches around and encloses the coils of the small intestine, and tends to be more fixed than the small intestine.
- The cecum is a blind-ended sac that projects downward in the right iliac region below the ileocecal junction.
- The appendix (vermiform appendix) is a worm-shaped tube that arises from the medial side of the cecum.
Mesenteries and Peritoneal Ligaments
- Mesenteries are two-layered folds of the peritoneum connecting parts of the intestines to the posterior abdominal wall.
- The peritoneal ligaments, omenta, and mesenteries serve as bridges that permit blood, lymph vessels, and nerves to reach the viscera.
- The lesser sac lies behind the stomach and the lesser omentum.
Peritoneal Functions
- The peritoneal fluid is pale yellow and somewhat viscid, and contains leukocytes.
- It ensures that the mobile viscera glide easily on one another due to the movements of the diaphragm and the abdominal muscles, together with the peristaltic movements of the intestinal tract.
- The peritoneal fluid is not static.
- The peritoneal coverings of the intestine tend to stick together (adhere) in the presence of infection.
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.