Podcast
Questions and Answers
What is the primary function of the Brunner's glands in the superior duodenum?
What is the primary function of the Brunner's glands in the superior duodenum?
- Neutralizing acidic chyme with mucous and bicarbonate (correct)
- Releasing hormonal triggers for the gallbladder and pancreas
- Producing enzymes for protein digestion
- Regulating the flow of bile into the duodenum
Which part of the duodenum is most commonly associated with duodenal ulcers?
Which part of the duodenum is most commonly associated with duodenal ulcers?
- Horizontal portion
- Ascending portion
- Superior portion (correct)
- Descending portion
What is the function of the spleen in infection control?
What is the function of the spleen in infection control?
- Filtering out bacteria from the circulation
- Recognizing and eliminating infected red blood cells (correct)
- Activating complement proteins to fight infection
- Producing antibodies against specific pathogens
What is the primary site of delivery for the stomach contents?
What is the primary site of delivery for the stomach contents?
What is the main function of the duodenum in digestion?
What is the main function of the duodenum in digestion?
What is the anatomical feature of the duodenum that distinguishes it from the jejunum and ileum?
What is the anatomical feature of the duodenum that distinguishes it from the jejunum and ileum?
What is the primary function of Brunner's glands in the duodenum?
What is the primary function of Brunner's glands in the duodenum?
What is the term for organs located behind the parietal peritoneum, without a mesentery?
What is the term for organs located behind the parietal peritoneum, without a mesentery?
What is the name of the duct that drains a portion of the head of the pancreas?
What is the name of the duct that drains a portion of the head of the pancreas?
What are the enzymes produced by the exocrine cells of the pancreas typically released in?
What are the enzymes produced by the exocrine cells of the pancreas typically released in?
Where is pancreatic pain typically felt?
Where is pancreatic pain typically felt?
What can cause pancreatic injury and/or pain if a duct is blocked?
What can cause pancreatic injury and/or pain if a duct is blocked?
What is the term for inflammation of the pancreas?
What is the term for inflammation of the pancreas?
What is the job of the gallbladder?
What is the job of the gallbladder?
What is the type of epithelium found in the mucosa of the gallbladder?
What is the type of epithelium found in the mucosa of the gallbladder?
What type of symptoms might one have after a cholecystectomy?
What type of symptoms might one have after a cholecystectomy?
What is the primary composition of cholesterol gallstones?
What is the primary composition of cholesterol gallstones?
What is the term for the liquid bile salts that are either more highly concentrated than normal or less motile than normal?
What is the term for the liquid bile salts that are either more highly concentrated than normal or less motile than normal?
What is the main reason why estrogen increases the incidence of gallstones?
What is the main reason why estrogen increases the incidence of gallstones?
What is the term for the phenomenon where the gallbladder is unable to empty properly, leading to bacterial overgrowth and inflammation?
What is the term for the phenomenon where the gallbladder is unable to empty properly, leading to bacterial overgrowth and inflammation?
What is the term for the inability to break down lactose into glucose and galactose?
What is the term for the inability to break down lactose into glucose and galactose?
What is the term for the phenomenon where food moves too quickly from the stomach into the small intestine, leading to diarrhea and cramping?
What is the term for the phenomenon where food moves too quickly from the stomach into the small intestine, leading to diarrhea and cramping?
What is the term for the process by which bile salts emulsify fats, making them absorbable?
What is the term for the process by which bile salts emulsify fats, making them absorbable?
What is the term for the removal of portions of the GI tract, leading to malabsorption?
What is the term for the removal of portions of the GI tract, leading to malabsorption?
What is the term for the inflammation of the intestine or colon, leading to malabsorption?
What is the term for the inflammation of the intestine or colon, leading to malabsorption?
What is the term for the phenomenon where the body is unable to absorb fats, leading to fatty stools and weight loss?
What is the term for the phenomenon where the body is unable to absorb fats, leading to fatty stools and weight loss?
What is the primary goal of giving a somatostatin agonist to a patient with dumping syndrome?
What is the primary goal of giving a somatostatin agonist to a patient with dumping syndrome?
What is the main characteristic of ulcerative colitis?
What is the main characteristic of ulcerative colitis?
What is the most common complication of mechanical bowel obstruction?
What is the most common complication of mechanical bowel obstruction?
What is the primary mechanism of constipation?
What is the primary mechanism of constipation?
What is the primary difference between ulcerative colitis and Crohn disease?
What is the primary difference between ulcerative colitis and Crohn disease?
What is the primary complication of fecal impaction?
What is the primary complication of fecal impaction?
What is the primary mechanism of inflammatory bowel disease?
What is the primary mechanism of inflammatory bowel disease?
What is the primary treatment for dumping syndrome?
What is the primary treatment for dumping syndrome?
What is the primary difference between normal transit constipation and slow-transit constipation?
What is the primary difference between normal transit constipation and slow-transit constipation?
What is the primary characteristic of Crohn disease?
What is the primary characteristic of Crohn disease?
Which type of diarrhea is caused by the inhibition of net sodium absorption or excessive mucosal secretion of chloride or bicarbonate-rich fluid?
Which type of diarrhea is caused by the inhibition of net sodium absorption or excessive mucosal secretion of chloride or bicarbonate-rich fluid?
What is the primary complication of intestinal inflammation?
What is the primary complication of intestinal inflammation?
What is the primary goal of treatment for diarrhea?
What is the primary goal of treatment for diarrhea?
What is the name of the condition characterized by out-pouchings of colonic mucosa through weakened areas in the muscular wall of the large intestine?
What is the name of the condition characterized by out-pouchings of colonic mucosa through weakened areas in the muscular wall of the large intestine?
What is the name of the medication that is an opiate and is used to treat diarrhea?
What is the name of the medication that is an opiate and is used to treat diarrhea?
What is the name of the condition characterized by inflammation of an out-pouching, usually caused by bits of fecal material trapped within the opening of the out-pouchings?
What is the name of the condition characterized by inflammation of an out-pouching, usually caused by bits of fecal material trapped within the opening of the out-pouchings?
Flashcards are hidden until you start studying
Study Notes
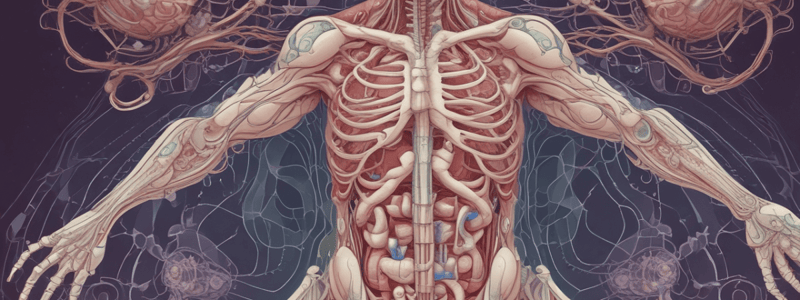
Foregut
- The spleen is not part of the GI system, but it plays a crucial role in:
- Early hematopoiesis
- Mechanical filtration of aging/injured erythrocytes
- Infection control, effective against pathogens within RBCs, like Malaria
- Clearance of bacteria from the circulation
- Clearance of microorganisms that the individual hasn't made a specific host antibody against
Duodenum
- The duodenum is the site of delivery for the stomach, pancreas, liver, and gallbladder
- Acidic chyme from the stomach must be neutralized in the duodenum to prevent:
- Duodenal ulcer, most commonly occurring in the superior portion
- The duodenum is responsible for:
- All types of digestion (protein, carbs, fats, nucleic acids)
- A large part of digestion, while other areas focus on absorption
- Anatomic features of the duodenum:
- Shortest segment of the small intestine
- Starts at the pyloric sphincter and ends at the Ligament of Treitz
- Almost completely retroperitoneal, not freely mobile in the abdominal cavity
- The pancreatic head nestles within its "C" curve
- Segments of the duodenum:
- Superior: releases hormonal triggers for the gallbladder and pancreas
- Descending: pancreatic duct and common bile duct empty here
- Horizontal: digestion occurs here; crosses the IVC and aorta
- Ascending: continued digestion; connects to the jejunum
- Brunner's glands:
- Unique to the proximal duodenum
- Release bicarbonate and mucous to neutralize chyme
- Rapidly neutralize high-pH chyme to protect the intestinal mucosa and enable intestinal enzymes to function
- Also secrete urogastrone, which inhibits the stomach's chief cells and parietal cells
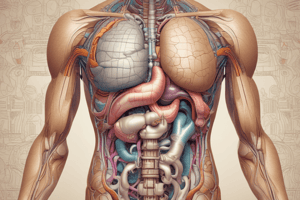
Pancreas
- The pancreas has both exocrine and endocrine functions
- It is retroperitoneal, arising from the wall of the duodenum
- Located mainly at L2, with parts including:
- Head
- Neck
- Body
- Tail
- The pancreatic ducts:
- The main pancreatic duct runs the entire length of the pancreas
- Empties its exocrine products at the Ampulla of Vater, where it joins the common bile duct
- A portion of the head of the pancreas usually drains via a different duct (the accessory pancreatic duct) at the Ampulla of Santorini
- Pancreatic juice:
- A secretion of pancreatic enzymes in a clear alkaline medium
- Enzymes produced by the exocrine cells of the pancreas
- Alkaline mucous liquid from the pancreatic ductal cells
- Flows to the duodenum via the pancreatic duct system
- Enzymes typically released in inactive form and activated by membrane-bound activators in the duodenum
- Pancreatic pain:
- May be felt in the mid-epigastric region (foregut) and/or the back due to the retroperitoneal location
- Can be caused by zymogens (pre-enzymes) of the pancreas activating early and causing tissue damage
Pancreatitis
- Inflammation of the pancreas
- Can occur when:
- A duct is blocked, causing zymogens to activate early and cause tissue damage
- Enzymes are activated prior to arriving at the duodenum
- Secondary to infection, trauma, or pancreatic carcinoma
- Symptoms of pancreatitis:
- Portions of the pancreas can autolyze (auto-digest)
- Cellular damage causes pancreatic enzymes to escape into the bloodstream at higher-than-normal rates
- Elevated amylase and lipase are markers for pancreatitis
Gallbladder
- The gallbladder's primary function is to store bile made by the liver and release it when needed
- Histology of the gallbladder:
- Mucosa with folds to allow for enlargement
- Simple columnar epithelium
- Lots of mucosal folds to enable enlargement and shrinkage
- Muscularis externa for contractions
- Adventitia to hold the gallbladder in place
- The normal biliary tree:
- Bile exits the liver via the left and right hepatic ducts
- Bile can travel into the gallbladder via the cystic duct
- Bile leaves the gallbladder via the cystic duct and enters the common bile duct
- There is only one way into and out of the gallbladder
- The gallbladder and pancreas share the same exit point (Sphincter of Oddi) into the duodenum
Gallbladder Problems
- Most common problems:
- Duct blockage
- Inflammation
- Infection
- Symptoms after a cholecystectomy:
- Fatty stools
- Poor tolerance of high-fat meals
- Dyspepsia
- Nausea and vomiting
Cholelithiasis
- Gallstones are crystallized/packed/solidified stones of gallbladder content
- Typically made of bile salts, cholesterol, and other substances
- Pathogenesis of cholesterol gallstones:
- More cholesterol in bile than can be dissolved
- Bile in stasis for longer than normal
- "Gallbladder sludge" increases the risk of gallstones
- Decreased gallbladder motility, often caused by estrogen, increases the risk of gallstones
- Pregnancy increases the incidence of gallstones
Inflammatory Bowel Disease
- Chronic, relapsing/recurring bowel inflammation of unknown origin
- Genetics: familial, most commonly diagnosed in those 20 to 40 years old
- Pathophysiology:
- Alterations of epithelial barrier functions
- Immune system reactions to intestinal flora
- Abnormal T-cell responses
- Presence of autoantibodies
- Two main types:
- Ulcerative colitis
- Crohn disease
Ulcerative Colitis
- A chronic inflammatory disease that causes ulceration of the colonic mucosa
- Sigmoid colon and rectum are most commonly affected
- Characteristic lesions:
- Continuous with no skipped lesions
- Limited to the mucosa
- Not transmural
- Diarrhea (10 to 20 bowel movements per day)
- Bloody stools
- Cramps
- Increased risk for colon cancer
Crohn Disease
- Granulomatous inflammation of the GI tract
- Can affect any part of the digestive tract
- Lesions:
- Cobblestone appearance
- Multilayer
- Transmural
- Abdominal pain and diarrhea are the most common signs
- More than five stools per day
- Anemia may develop due to malabsorption of vitamin B12 and folic acid
Mechanical Bowel Obstruction
- Blockage in the small or large bowel
- Small bowel contents cannot travel "downstream"
- Risk factors:
- Prior surgery
- Presence of carcinoma
- Diseases causing gut inflammation/stricture (like IBD)
- Volvulus and intussusception
- Clinical manifestations:
- Gas/chyme builds up and the bowel distends
- Venous flow in the GI wall slows
- Arterial flow slows
- Bowel wall starts to die
- Edema and bacteria escape from the bowel into the peritoneum
- Peritonitis and bowel perforation are common
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.