Podcast
Questions and Answers
Which nephron segment is primarily responsible for reabsorbing sodium, potassium, and chloride?
Which nephron segment is primarily responsible for reabsorbing sodium, potassium, and chloride?
- Glomerulus
- Distal Convoluted Tube
- Descending Loop of Henle
- Proximal Convoluted Tubule (correct)
At which part of the nephron do loop diuretics such as Lasix exert their primary effect?
At which part of the nephron do loop diuretics such as Lasix exert their primary effect?
- Collecting Duct
- Distal Convoluted Tube
- Ascending Loop of Henle (correct)
- Proximal Convoluted Tubule
What is the primary function of erythropoietin produced by the kidneys?
What is the primary function of erythropoietin produced by the kidneys?
- Stimulates red blood cell production (correct)
- Regulates blood pressure
- Increases urine output
- Balances electrolytes in urine
What role do aldosterone and ADH play in the nephron?
What role do aldosterone and ADH play in the nephron?
Which waste product is primarily excreted by the kidneys as a result of amino acid metabolism?
Which waste product is primarily excreted by the kidneys as a result of amino acid metabolism?
What is the normal range for the Anion Gap?
What is the normal range for the Anion Gap?
Which of the following is NOT a common cause of Acute Kidney Injury (AKI)?
Which of the following is NOT a common cause of Acute Kidney Injury (AKI)?
What urine pH indicates a normal acidic urine?
What urine pH indicates a normal acidic urine?
Which diagnostic criteria suggests a decrease in urine volume in Acute Kidney Injury?
Which diagnostic criteria suggests a decrease in urine volume in Acute Kidney Injury?
What is the normal range for Creatinine Clearance?
What is the normal range for Creatinine Clearance?
An increase in serum creatinine by how much within 48 hours indicates a potential Acute Kidney Injury?
An increase in serum creatinine by how much within 48 hours indicates a potential Acute Kidney Injury?
Which imaging study requires the injection of contrast dye?
Which imaging study requires the injection of contrast dye?
What is a common consequence of fluid overload in patients with kidney dysfunction?
What is a common consequence of fluid overload in patients with kidney dysfunction?
During the recovery phase of kidney injury, which of the following changes can be expected?
During the recovery phase of kidney injury, which of the following changes can be expected?
What electrolyte imbalance is commonly observed in the early stages of acute kidney injury?
What electrolyte imbalance is commonly observed in the early stages of acute kidney injury?
What is the expected duration of the diuretic phase following acute kidney injury?
What is the expected duration of the diuretic phase following acute kidney injury?
In chronic kidney disease, what characterizes stage 3?
In chronic kidney disease, what characterizes stage 3?
What is the most common cause of Acute Tubular necrosis in Acute Kidney Injury?
What is the most common cause of Acute Tubular necrosis in Acute Kidney Injury?
Which phase of Acute Kidney Injury is characterized by urine output being less than 0.5 ml/hour?
Which phase of Acute Kidney Injury is characterized by urine output being less than 0.5 ml/hour?
What does Hyperkalemia indicate in the context of Acute Kidney Injury?
What does Hyperkalemia indicate in the context of Acute Kidney Injury?
What is a common risk factor for Postrenal Acute Kidney Injury?
What is a common risk factor for Postrenal Acute Kidney Injury?
Which condition is least likely to directly lead to intrinsic Acute Kidney Injury?
Which condition is least likely to directly lead to intrinsic Acute Kidney Injury?
What typically happens during the Recovery Phase of Acute Kidney Injury?
What typically happens during the Recovery Phase of Acute Kidney Injury?
What is a primary initial insult that can lead to Acute Kidney Injury?
What is a primary initial insult that can lead to Acute Kidney Injury?
In what scenario would a patient most likely experience Oliguric Phase?
In what scenario would a patient most likely experience Oliguric Phase?
Which of the following provides the least indication of an acute kidney injury?
Which of the following provides the least indication of an acute kidney injury?
What is a key characteristic of prerenal Acute Kidney Injury?
What is a key characteristic of prerenal Acute Kidney Injury?
Flashcards are hidden until you start studying
Study Notes
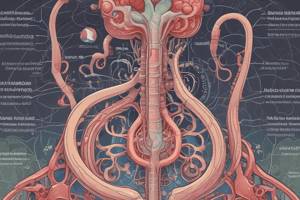
Anatomy of the Kidney
- Each kidney contains about 1 million nephrons.
- These nephrons filter fluid and solutes from the blood.
Nephron Function
- Glomerulus: Filters fluid and solutes from the blood.
- Proximal Convoluted Tubule: Reabsorbs sodium, potassium, chloride, bicarbonate, glucose, and amino acids.
- Descending Loop of Henle: Site of action for osmotic diuretics (like Mannitol).
- Ascending Loop of Henle: Site of action for loop diuretics (like Lasix).
- Distal Convoluted Tubule: Reabsorbs water, acid-base balance is affected by ADH and aldosterone. Site of action for thiazides (like HCTZ).
- Collecting Duct: Last step in water and waste balance, site of action for potassium-sparing diuretics (like Spironolactone).
Renal System Functions
- Regulates ions in the blood, including sodium, potassium, calcium, chloride, and phosphate.
- Regulates blood volume by adjusting the volume of blood or eliminating it in the urine.
- Regulates hydrogen ion excretion in the urine.
- Produces hormones:
- Calcitriol: Calcium homeostasis.
- Erythropoietin: Production of red blood cells. Renal patients are prone to anemia due to lack of erythropoietin.
- Renin: Helps regulate blood pressure, leading to increased blood pressure.
- Excretes waste products like:
- Ammonia and urea: Amino acid breakdown.
- Creatinine: Creatinine phosphate breakdown.
- Other functions include:
- Acid-base balance
- Erythropoiesis
- Toxin removal
- Diuretic control
- Electrolyte balance
- Vitamin D activation
Labs
- BUN (Blood Urea Nitrogen): 5-20 mg/dL
- Creatinine: 0.5 - 1.2 mg/dL
- BUN to Creatinine Ratio: 20:1
- Creatinine Clearance: 110-120 mL/min (men)
- 90-110 mL/min (women)
- Osmolarity: 275-293 mOsm/kg
- Anion Gap: 8 - 16 mEq/L
- Hemoglobin: 13.5-17.5 g/dL (men)
- 12-16 g/dL (women)
- Hematocrit: 37-47% (men)
- 34-44% (women)
- Albumin: 3.5 - 5.0 g/dL
- Urine output: 1-2 liters/day (normal)
- High output can contribute to electrolyte imbalance and dehydration.
Urine Dipstick
- Appearance: Color, clarity, and odor.
- Urine pH: Normal urine is acidic (4.5 to 8).
- Protein: Greater than or equal to 150 mg/day may indicate kidney injury.
- Glucose: Monitor for hyperglycemia (diabetes mellitus).
- WBC: Indicates an infection. Cystitis can cause high WBC counts in urine.
- Blood: Few red blood cells are normal. High amounts are abnormal and can be caused by UTI’s, kidney infections, cancer, trauma, medications, or irritation.
Imaging Studies
- Ultrasound: Visualizes the kidneys.
- KUB (Kidneys, Ureters, Bladder): X-ray image of the kidneys, ureters, and bladder.
- Angiography: Injects contrast dye to visualize the urinary tract.
- CT: Computerized tomography image. Provides better detail than a regular X-ray.
- MRI: Magnetic resonance imaging. Provides detailed images of the urinary tract.
Acute Kidney Injury (AKI)
- Characterized by a sudden increase in creatinine levels.
- Caused by a decrease in glomerular filtration rate (GFR) and retention of blood products normally excreted by the kidneys.
- Most common causes of AKI include:
- Sepsis
- Hypovolemia
- Medications or medication-induced injury
- Cardiogenic shock
- Diagnostic criteria:
- Serum creatinine increase of > 0.3 mg/dL within 48 hours
- Serum creatinine increase of > 1.5 mg/dL from baseline within 7 days.
- Urine volume decreases to < 0.5 ml/kg/hr for 6 hours.
- Risk factors:
- Sepsis
- Burns
- Trauma
- Chronic kidney disease
- Advanced age
- Diabetes mellitus
- Rhabdomyolysis: Damage to muscles release myoglobin which clogs the glomeruli (can occur in trauma, sepsis, or prolonged immobility).
Causes of Acute Kidney Injury
- Pre-renal AKI: Caused by decreased blood flow to the kidneys. Often reversible with treatment.
- Intra-renal AKI: Direct damage to the nephrons. This can be caused by acute tubular necrosis (most common).
- Post-renal AKI: Caused by obstruction of the urinary tract, such as blockage of ureters, prostate, or bladder.
Four Phases of Acute Kidney Injury
- Initiation: Initial insult that triggers the AKI.
- Oliguric: Decreased urine output (< 0.5 mL/kg/hr).
- Diuretic: Increased urine output.
- Recovery: Gradual return to normal kidney function.
Initiation Phase of Acute Kidney Injury
- Initial Insult: Insult that triggers the AKI.
- Urine output less than 0.5 mL/kg/hr for at least 6 hours.
- Lasts for hours to days.
- Ends when the Oliguric Phase begins.
Oliguric Phase of Acute Kidney Injury
- Decreased GFR: Reduced filtration rate.
- Dark urine: High concentration of waste products in urine.
- Specific gravity elevated above 1.010: Indicates concentrated urine due to reabsorption of water.
- Hyperkalemia: Elevated blood potassium levels due to decreased excretion.
- Hyperphosphatemia: Elevated blood phosphate levels.
- Hypocalcemia: Low blood calcium levels due to decreased production of calcitriol (vitamin D) by the kidneys.
- Urinary casts: Casts of cells and protein in urine, indicating kidney damage.
- Elevated blood urea nitrogen (BUN) and creatinine: Indicates reduced kidney filtration.
- Decreased serum osmolarity: Dilution of body fluids.
- Uremia: Build-up of waste products in the blood due to decreased kidney filtration.
- Hyponatremia: Low blood sodium levels.
- Increased retention of fluid: Fluid overload.
- Metabolic acidosis: Occurs due to the inability of the kidneys to excrete acids effectively.
- Clinical manifestations: Symptoms of fluid overload, such as:
- Decreased urine output
- Fluid volume overload
- Fatigue
- Distended neck veins
- Bounding pulse
- Edema
- High blood pressure (HTN)
- Pulmonary edema
- Heart failure
- Nausea and loss of appetite
Diuretic Phase of Acute Kidney Injury
- Lasts for 1-3 weeks.
- High urine output (2-5 liters/day): Occurs due to osmotic diuresis (high levels of waste products in the tubules causing increased water excretion).
- Dilute urine: Body loses fluid and electrolytes.
- Monitor for decreased:
- Fluid volume
- Blood pressure
- Sodium levels
- Potassium levels
Recovery Phase of Acute Kidney Injury
- Can take up to 12 months.
- Urine output normalizes: Kidney function gradually improves.
- Electrolyte imbalances resolve: Electrolyte levels return to normal.
- Fluid imbalances balance improves: Fluid levels normalize.
- Acid-base balance improves: Acid-base balance returns to normal.
Chronic Kidney Disease (CKD)
- Stages:
- Stage 1: Normal GFR but albuminuria is present.
- Stage 2: GFR 60-89 mL/min. Albuminuria is present.
- Stage 3: GFR 30-59 mL/min.
- Stage 4: GFR 15-29 mL/min.
- Stage 5: CKD requiring renal replacement therapy. This stage is also called End Stage Renal Disease (ESRD).
- **Normal GFR in young adults is 120 mL/min/1.73m2. **
- Causes:
- Diabetes mellitus
- Polycystic kidney disease
- High blood pressure
- Recurrent kidney infections
- Glomerulonephritis
- Prolonged use of medications like NSAIDs
- Prolonged blockages in the urinary tract.
- Symptoms:
- Fatigue and weakness
- Muscle cramps
- Changes in urination patterns
- Edema (legs, ankles, feet)
- Itchy skin
- Nausea or vomiting
- Shortness of breath
- Loss of appetite
- Difficulty sleeping
Cardiorenal Syndrome (CRS)
- CRS: Heart failure that results in acute kidney injury.
- Type 1 CRS: Acute heart failure that results in AKI.
- Type 2 CRS: Chronic heart failure that results in AKI.
- Type 3 CRS: AKI that results in acute heart failure.
- Type 4 CRS: AKI that results in chronic heart failure.
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.