Podcast
Questions and Answers
A patient with an infected non-healing foot ulcer due to diabetes requires an amputation to prevent sepsis. Which of the following indications for amputation does this scenario represent?
A patient with an infected non-healing foot ulcer due to diabetes requires an amputation to prevent sepsis. Which of the following indications for amputation does this scenario represent?
- Congenital Deformity
- Tumor
- Trauma
- Peripheral Vascular Disease (PVD) (correct)
An above-the-elbow amputation (AEA) involves the removal of the limb through the radius and ulna.
An above-the-elbow amputation (AEA) involves the removal of the limb through the radius and ulna.
False (B)
List three aspects of pre-operative nursing care for a patient undergoing amputation.
List three aspects of pre-operative nursing care for a patient undergoing amputation.
Assessment of overall health, psychological preparation, and patient education.
__________ amputation is defined as ankle disarticulation.
__________ amputation is defined as ankle disarticulation.
Why is it important to monitor vital signs frequently in the post-operative period following an amputation?
Why is it important to monitor vital signs frequently in the post-operative period following an amputation?
Match the type of amputation with the corresponding anatomical location:
Match the type of amputation with the corresponding anatomical location:
A patient who underwent a below-the-knee amputation is at risk for developing which type of contracture if not properly positioned?
A patient who underwent a below-the-knee amputation is at risk for developing which type of contracture if not properly positioned?
Psychological preparation for a patient undergoing amputation focuses solely on providing information about the surgical procedure and expected physical outcomes, while disregarding their emotional and body image concerns.
Psychological preparation for a patient undergoing amputation focuses solely on providing information about the surgical procedure and expected physical outcomes, while disregarding their emotional and body image concerns.
What is the primary purpose of applying compression bandages to the residual limb after an amputation?
What is the primary purpose of applying compression bandages to the residual limb after an amputation?
Early ambulation post-amputation is discouraged to prevent complications like pneumonia and DVT.
Early ambulation post-amputation is discouraged to prevent complications like pneumonia and DVT.
Name three potential complications that can arise following an amputation.
Name three potential complications that can arise following an amputation.
A common post-amputation condition characterized by pain originating from the removed limb is known as _______ _______ pain.
A common post-amputation condition characterized by pain originating from the removed limb is known as _______ _______ pain.
Match the following post-amputation care aspects with their respective benefits:
Match the following post-amputation care aspects with their respective benefits:
When should prosthetic fitting typically begin after an amputation?
When should prosthetic fitting typically begin after an amputation?
Occupational therapy is not helpful in teaching patients how to perform activities of daily living with a prosthesis.
Occupational therapy is not helpful in teaching patients how to perform activities of daily living with a prosthesis.
List three feelings or emotions that a patient might experience following an amputation.
List three feelings or emotions that a patient might experience following an amputation.
Encouraging a patient to focus on their strengths and abilities, and to set _________ goals for recovery is important for psychological support following amputation.
Encouraging a patient to focus on their strengths and abilities, and to set _________ goals for recovery is important for psychological support following amputation.
Which of the following is NOT a key nursing intervention following an amputation?
Which of the following is NOT a key nursing intervention following an amputation?
It is not important to educate the patient and family about post-operative care after an amputation.
It is not important to educate the patient and family about post-operative care after an amputation.
Besides medication, name one non-pharmacological pain management technique that can be used to help manage post-amputation pain.
Besides medication, name one non-pharmacological pain management technique that can be used to help manage post-amputation pain.
Hip and knee ___________ can develop if a patient is not properly positioned after amputation.
Hip and knee ___________ can develop if a patient is not properly positioned after amputation.
What should patients avoid to maintain healthy circulation of the residual limb and reduce risk of complications?
What should patients avoid to maintain healthy circulation of the residual limb and reduce risk of complications?
Why is a diet high in protein, vitamins, and calories important for a patient post-amputation?
Why is a diet high in protein, vitamins, and calories important for a patient post-amputation?
Flashcards
Amputation
Amputation
Removal of a limb or part of a limb.
Above-the-knee amputation (AKA)
Above-the-knee amputation (AKA)
Amputation through the femur (thigh bone).
Below-the-knee amputation (BKA)
Below-the-knee amputation (BKA)
Amputation through the tibia and fibula (lower leg bones).
Above-the-elbow amputation (AEA)
Above-the-elbow amputation (AEA)
Signup and view all the flashcards
Below-the-elbow amputation (BEA)
Below-the-elbow amputation (BEA)
Signup and view all the flashcards
Syme's amputation
Syme's amputation
Signup and view all the flashcards
Peripheral vascular disease (PVD)
Peripheral vascular disease (PVD)
Signup and view all the flashcards
Post-operative Nursing Care (Amputation)
Post-operative Nursing Care (Amputation)
Signup and view all the flashcards
Compression Bandages (Amputation)
Compression Bandages (Amputation)
Signup and view all the flashcards
Early Ambulation (Post-Amputation)
Early Ambulation (Post-Amputation)
Signup and view all the flashcards
Phantom Limb Pain
Phantom Limb Pain
Signup and view all the flashcards
Neuroma
Neuroma
Signup and view all the flashcards
Contractures (Post-Amputation)
Contractures (Post-Amputation)
Signup and view all the flashcards
Stump Care Basics
Stump Care Basics
Signup and view all the flashcards
Prosthetic Rehabilitation
Prosthetic Rehabilitation
Signup and view all the flashcards
Psychological Support (Amputation)
Psychological Support (Amputation)
Signup and view all the flashcards
Pain Management (Post-Amputation)
Pain Management (Post-Amputation)
Signup and view all the flashcards
Wound Care (Amputation)
Wound Care (Amputation)
Signup and view all the flashcards
Positioning (Post-Amputation)
Positioning (Post-Amputation)
Signup and view all the flashcards
Edema Control (Amputation)
Edema Control (Amputation)
Signup and view all the flashcards
Education (Post-Amputation)
Education (Post-Amputation)
Signup and view all the flashcards
Mobility (Post-Amputation)
Mobility (Post-Amputation)
Signup and view all the flashcards
Psychological Impact of Amputation
Psychological Impact of Amputation
Signup and view all the flashcards
Study Notes
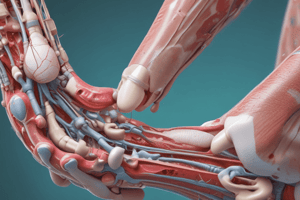
- Amputation involves the removal of a limb or part of a limb
Types of Amputation
- Amputations are categorized by the level of the limb that is removed
- Above-the-knee amputation (AKA) means amputation through the femur
- Below-the-knee amputation (BKA) means amputation through the tibia and fibula
- Above-the-elbow amputation (AEA) means amputation through the humerus
- Below-the-elbow amputation (BEA) means amputation through the radius and ulna
- Syme's amputation is ankle disarticulation
- You can have a Toe or partial foot amputation which is the removal of one or more toes or part of the foot
- You can have a Finger or partial hand amputation which is removal of one or more fingers or part of the hand
Indications for Amputation
- Peripheral vascular disease (PVD), often associated with diabetes, is a common cause for lower extremity amputations because of poor circulation and tissue necrosis
- Trauma can result in amputation if a limb is crushed, severely damaged, or cannot be adequately reconstructed
- Infection, such as osteomyelitis or sepsis, may necessitate amputation to prevent the spread of infection
- Tumors, both benign and malignant, in the bone or soft tissues of a limb may require amputation
- Congenital deformities may be corrected with amputation and prosthetics
Pre-operative Nursing Care
- Assessment includes evaluating the patient's overall health, including cardiovascular status, nutritional status, and the presence of infection
- Psychological preparation involves addressing the patient's fears, anxieties, and concerns about the surgery, body image, and future mobility
- Patient education includes explaining the surgical procedure, the expected outcome, post-operative care, pain management, and rehabilitation
- The affected limb should be assessed for skin integrity, circulation, and sensation
- Baseline vital signs, including blood pressure, heart rate, and respiratory rate, are recorded
Post-operative Nursing Care
- Vital signs should be monitored frequently to detect any signs of instability, such as hypotension or tachycardia
- The surgical site should be assessed for bleeding, edema, redness, drainage, and odor
- Pain should be managed with prescribed analgesics, and the patient's pain level is regularly assessed using a pain scale
- Proper positioning helps prevent contractures, especially hip and knee flexion contractures after lower extremity amputation
- Wound care involves keeping the surgical site clean and dry, changing dressings as ordered, and monitoring for signs of infection
- Compression bandages are applied to the residual limb to reduce edema, support the soft tissues, and promote shaping of the limb for prosthetic fitting
- Early ambulation, as tolerated, helps improve circulation, prevent complications such as pneumonia and deep vein thrombosis (DVT), and promote independence
- The patient should be encouraged to express their feelings about the amputation, and be provided with emotional support and counseling if needed
- Assess the patient's nutritional status and provide a diet that is high in protein, vitamins, and calories to promote wound healing
Potential Complications
- Infection at the surgical site can occur, leading to delayed healing, further tissue damage, or systemic infection
- Hemorrhage can occur post-operatively, requiring intervention to control bleeding
- Phantom limb pain is the sensation of pain in the amputated limb; it is a common complication that can be difficult to treat
- Neuroma: A tumor formed of nerve tissue
- Contractures, especially hip and knee flexion contractures, can develop if the patient is not properly positioned and does not perform range-of-motion exercises
- Skin breakdown can occur due to pressure from the cast or prosthetic; regular skin assessment is crucial
- Deep vein thrombosis (DVT) and pulmonary embolism (PE) are risks in post-operative patients, especially those with limited mobility
Phantom Limb Pain
- Phantom limb pain is a common condition experienced by individuals after amputation characterized by the sensation of pain originating from the removed limb
- Symptoms can vary widely, including shooting, stabbing, burning, cramping, or aching sensations
- The exact cause of phantom limb pain is not fully understood but it is believed to involve a combination of peripheral and central nervous system factors
- Treatment options include medications (such as analgesics, antidepressants, and anticonvulsants), nerve blocks, TENS, and complementary therapies such as acupuncture and massage
- Psychological support and counseling are important in helping patients cope with chronic pain
Stump Care
- Residual limb care is essential to promote healing, prevent complications, and prepare the limb for prosthetic fitting
- Wash the residual limb daily with mild soap and water, and dry thoroughly
- Inspect the skin for signs of breakdown, irritation, or infection
- Apply a clean compression bandage to reduce edema and promote shaping of the limb
- Perform range-of-motion exercises to prevent contractures and maintain joint mobility
- Encourage the patient to participate in activities of daily living to promote independence
- Avoid prolonged sitting or immobility, which can impair circulation and increase the risk of complications
Prosthetic Rehabilitation
- Prosthetic fitting usually begins several weeks or months after amputation, once the residual limb has healed and edema has subsided
- A prosthetist will assess the patient's needs and goals and fabricate a custom-made prosthesis
- Physical therapy is crucial to teach the patient how to use the prosthesis effectively, improve balance and coordination, and increase strength and endurance
- Occupational therapy may be helpful in teaching the patient how to perform activities of daily living with the prosthesis
- Regular follow-up appointments are important to monitor the fit and function of the prosthesis and make adjustments as needed
Psychological Support
- Amputation can have a profound psychological impact on patients, leading to feelings of grief, loss, anxiety, depression, and body image disturbances
- Encourage the patient to express their feelings and concerns
- Provide emotional support and counseling, and refer the patient to a mental health professional if needed
- Support groups can provide a sense of community and shared experience
- Encourage the patient to focus on their strengths and abilities and to set realistic goals for recovery and rehabilitation
Key Nursing Interventions
- Pain Management: Administer prescribed analgesics, assess pain levels, and use non-pharmacological pain management techniques
- Wound Care: Monitor the surgical site for signs of infection, change dressings, and promote wound healing
- Positioning: Prevent contractures by positioning the patient properly and encouraging range-of-motion exercises
- Edema Control: Apply compression bandages to reduce edema and promote shaping of the residual limb
- Psychological Support: Provide emotional support and counseling to help the patient cope with the psychological impact of amputation
- Education: Educate the patient and family about post-operative care, prosthetic rehabilitation, and potential complications
- Mobility: Encourage early ambulation and participation in physical therapy to improve strength, balance, and coordination
NCLEX-Style Questions Considerations
- Focus on prioritizing interventions based on patient assessments and potential complications
- Knowledge of expected post-operative findings versus signs of complications is essential
- Understanding of the psychological aspects of amputation and appropriate support strategies is important
- Be familiar with proper stump care techniques and the role of the nurse in prosthetic fitting and rehabilitation
- Safety is a key consideration, especially in preventing falls and ensuring proper use of assistive devices
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.